To the Editor,
Patent foramen ovale (PFO) is an incomplete closure of the interatrial septum. This is a frequent finding in healthy individuals. Under conditions in which there is an increase of pressure in the right chambers of the heart, a right-left shunt may arise, with variable degrees of secondary hypoxaemia.
A 26-year-old male was admitted for craniocephalic trauma, which evolved without complications, and chest trauma, with pneumothorax and lung contusion. The patient was treated with bed rest, mechanical ventilation (MV) and insertion of a pleural drainage. The patient was kept in controlled-assisted ventilation with a FiO2 of 0.4 and without PEEP. On the second day he developed hypoxaemic respiratory failure secondary to lung infection, which required a FiO2 of 1. PEEP was increased, but no significant changes were seen in oxygenation or ventilation.
On day 10 it was necessary to start noradrenaline administration. A transthoracic echocardiogram (TTE) was performed that did not detect any alteration.
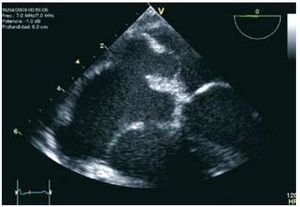
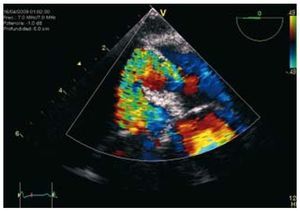
On day 12 PEEP had reached 20 cmH2O and respiratory failure persisted. A chest computed tomography (CT) was taken, this showed lung condensation, with no other complications, and a cranial CT was taken, that showed an acute ischaemic lesion. A transesophageal echocardiogram (TEE) was performed that showed an aneurysm in the interatrial septum and a patent foramen ovale (PFO) (Figures 1 and 2). The administration of shaken saline fluid as bubble contrast confirmed the shunt. PEEP was reduced from 20 to 5 cmH2O and SaO2 improved immediately from 75% to 92%.
Figure 1. Aneurysm of the interatrial septum 20 mm from the base and 11 mm from the septum and 10 mm patent foramen ovale.
Figure 2. Doppler colour image of flow through the patent foramen ovale.
Simultaneously, thrombosis of the left jugulosubclavianaxillary axis was detected by catheterisation. The stroke was attributed to paradoxical embolism through the persistent foramen ovale (PFO).
As the patient continued to require a FiO2 of 1, the percutaneous closure of the PFO was planned. Twenty-four hours before placement of the device the patient presented pneumothorax. Drainage was performed, but respiratory failure persisted and the patient died.
A PFO is an incomplete closure of the interatrial septum. This condition is present in 25%-30% of healthy individuals, with similar prevalence in both sexes. Its cause is unknown, but it is possible there may be a genetic component. It can be associated with aneurysm of the interatrial septum or a Chiari network or a more prominent Eustachian valve.
PFO is diagnosed by TEE; TTE, or transcranial Doppler. Transesophageal echocardiogram (TEE) is the most sensitive and specific of these techniques and makes it possible to study other associated structures. Transthoracic echocardiogram (TTE) has a high specificity, but less sensitivity and is more operator-dependent and acoustic window-dependent, which makes it of more limited use in ventilated patients with positive pressure.
Most individuals with PFO are asymptomatic. Its importance has been classically associated with ischaemic stroke caused by paradoxical embolism. For it to take place the pressure gradient between the atria must become inverted.
PFO has also been implicated in paradoxical embolisms of other kinds: fatty, tumour and air (in decompression accidents) and is associated with migraine, vascular headache and platypnea-orthodeoxia syndrome.
Application of a PEEP >5 cmH2O in acute lung conditions has been shown to improve oxygenation.1 However, it increases the pressure of the right chambers and reduces cardiac output, especially if the patient is hypovolaemic and/or the PEEP is excessive.2 For that reason, a high PEEP favours left-right shunts through the PFO. The degree of shunt is affected by the anatomy of the right atria, the size of the PFO and the interatrial pressure gradient.3 Bedside echocardiography makes it possible to control the haemodynamic effects of MV non-invasively.4
The usual indication for PFO closure is stroke recurrence, but it is also indicated in platypneaorthodeoxia syndrome with significant hypoxaemia.5 For this reason we considered it in our patient.
We have presented a case of persistent foramen ovale, a diagnosis to be considered in all patients with hypoxaemic respiratory failure and MV that do not improve or even worsen when PEEP is increases or on a ventilation strategy that causes auto-PEEP.