The End of Some Dogmas
A dogma is any point of doctrine that is believed to be unquestionable and certain. In this sense, in electrocardiographic diagnosis, the dogma that there was a posterior wall of the left ventricle and that post-infarction patients in which a tall R wave appeared in V1 through V2 had an infarction of that wall was considered certain and unquestionable. Besides, the presence of QS morphology in VL was considered as a manifestation of a high lateral infarction. Lastly, it was believed, ever since Myers et al1-3 anatomopathologic correlation study, in the 1940s, that the localization of a Q wave infarction was as follows: Q in V1 through V2 indicated septum infarction, V3 through V4 anterior, V5 through V6 low lateral, I through VL high lateral, and II, III, VF inferior.
How the Dogma That the Posterior Wall Existed and That a Posterior Infarct Originated an R Wave in V1 Through V2, the High Lateral Infarction Led to the QS Morphology in VL, and the Anteroseptal Infarct Generated a Q Wave in V1 Through V4 Was Generated and Perpetuated
In 1940s, just after the implementation of the precordial leads, it was generally considered that there was an anterior infarct (Q in I and VL, and precordials), and a posterior one (Q in II, III, VF).4 In the 1950s, some authors5 indicated that the posterior, which was the one that was in contact with the diaphragm, would be better called inferior or diaphragmatic. When Perloff6 coined the concept of a strict posterior infarct to explain the RS morphology in V1 through V2, the expression was considered fortunate because it explained what was clear for this electrocardiographic patent, since this necrosis affected the basal part of the inferior wall that was thought to go always upwards and that, for this reason, was denominated the authentic or strict posterior wall. He was then correct to think that the infarct of what was called the strictly posterior wall originated a vector of necrosis that travelled from the back to the front and that was manifested by an RS in V1 through V2, an expression of the Q wave that was registered in the back (Figure 1A). Naturally, if the infarct only occupied the medial and apical part of the wall that rests on the diaphragm, the authentic inferior wall originated a Q wave in II, III, VF that was considered as an expression of an inferior wall infarctionand, therefore, the infarct occupied the inferior wall and the authentically posterior corresponded to an inferoposterior infarct (Q in II, III, VF + RS in V1 through V2) (Figure 1A).
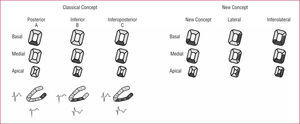
Figure 1. The classical concept of the myocardial infarction classification due to the occlusion of the right coronary artery or the circumflex artery (inferolateral zone) is shown here. The basal segment of the wall in contact with the diaphragm (inferior wall) was considered as an upward curve and this portion of the wall was named the posterior wall. Because it was believed that the posterior wall infarction explained the presence of SR in V1 (an equivalent to the Q wave) the myocardial infarction of the inferolateral zone was divided in groups: inferior (Q in II, III. and VF), posterior (RS V1, V2), and lateral (pathologic Q in laterals leads). In infarctions involving 2 or 3 of these areas it receives the corresponding name (inferoposterior, inferolateral, posterolateral). To the left the area involved in the case of the inferior, posterior, and inferoposterior infarction is shown, with ECG patterns in a chronic phase. To the right: with the newly exposed concept, the RS patent in V1 is explained by a lateral myocardial infarction and the infarction of the inferobasal segment of the inferior wall (classically called the posterior wall) does not generate a Q wave because it is a zone of delayed depolarization. In this way, inferolateral zone infarcts are divided in 3 groups: inferior (Q in II, III, and VF), lateral (RS V1 and/or pathologic Q waves in lateral leads), and inferolateral (both patterns).
Although some authors7 manifested that the anatomopathological correlation that the R on V1 was more easily explained by a lateral infarct tan a posterior one, their studies had no echo or were obscured by the prestige of Perloff and the journal in which he published his paper, as well as by the enormous capacity that humans have to transmit wrong information when we believe it to be an article of faith. Even recently there has been evidence, in an age of radionuclide imaging studies8 and magnetic resonance,9,10 that the infarct that originates a R wave in V1 is lateral and not posterior. In spite of that, in all of the textbooks, including ours, task forces and guidelines11-18 have taken for granted the fact that the posterior infarction was the lesion that generated a tall R wave in V1. It was never questioned whether Perloff could be wrong, probably because their research had never been cast in doubt. All of the electrocardiographists had assimilated and copied in different forms his sagital slicing of the heart6 in which the localization of the posterior wall infarction originated a necrosis vector that traveled forward and gave place to the R wave on V1.
In a similar manner, during the 1950s, the idea arose that a high lateral infarction originated changes in I and VL (QR, QS, r with a negative T) without an apparent modification in the precordial leads. The Mexican school vigorously defended this concept high lateral infarction when the image with a Q (QS QR) was seen, especially in VL and sometimes in I, and of a low lateral infarction when it was seen especially in V5 through V6.5,19 The fact that I, VL, and V5 through V6 are high and low lateral leads, respectively, facilitated this correlation. This concept was also transformed into dogma and perpetuated in most cardiology and ECG (electrocardiogram) books, ours included.
Finally, the name anteroseptal infarction for those cases with a Q wave from V1 to V4 has been questioned for a long time.20,21 Q waves in V1 through V2 only appear when the middle and lower parts of the septum6 are affected and different imaging techniques, starting by echocardiography20 and magnetic resonance,22,23 have demonstrated that in the case of a Q wave further tan V2 the affected zone is clearly apical, with more or less affection of the anterior, septal, and inferior walls according to the length of the anterior descending artery. Because of this, the most appropriate name in our opinion is apical/anterior.24
Demonstration That Often the Posterior Wall Does Not Exist and That the R Wave in V1 Owes Itself to a Lateral Infarction and the QS Morphology in VL Is Due to a Medial-Anterior Infarction
We have had our doubts about the anatomopathological correlation in electrocardiography for years,1-3 fundamentally for 2 reasons: a) because the placing of the precordial electrodes has changed slightly over time, and in the same patient the morphology of the ECG can be changed by moving the precordial leads making the Q wave appear and disappear; the presence of Q in V5 and, in consequence, we can no longer perform the diagnosis of a lateral infarction. We can, therefore, turn a lateral infarction into an anterior one to our liking, and vicecersa; and b) because we could not see clearly, when verifying with the anatomy atlas,25 that the whole basal part of the wall was evidently resting on the diaphragm, named diaphragmatic or inferior, was directed upwards in a true manner and authentically became posterior.
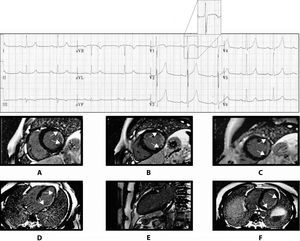
We know of the reliability of magnetic resonance imaging (MRI) with gadolinium contrast (MRI-G) to identify and locate the presence of an infarct,26,27 we decided, together with the Imaging Unit of the Hospital de Sant Pau, to study the ECG-MRI correlation in cases of Q wave infarction. We immediately proved in a sagital scan of the heart that in more than two-thirds of the cases the posterior wall did not exist, because the basal part of the inferior wall was simply a continuation of said wall in the same direction. That was in agreement with the diagrams observed in most anatomy books.25 We then correlated the cases that theoretically corresponded to an inferior infarction exclusively, because they had an uptake of gadolinium in segment 4 that, according to the Expert Committee of the American Heart Association (AHA),28 corresponded to what previously was known as the exclusive posterior wall, and we were able to prove that in V1, contrary to what was expected, there was an rS morphology instead of RS. The images in MRI, in the horizontal scans, gave us the solution because it allowed us to prove that the heart was not situated in an exclusive posteroianterior sense (Figure 2A), following what is said by anatomists that study the heart out of the thorax, the form of Saint Valentine,29 but presented an rS morphology instead of an RS one. It was in an oblique posteroanterior and right-left direction (Figures 2B y C). Therefore, in the case of an infarct of the previously named posterior wall, now and according to the AHA consensus, inferobasal segment of the inferior wall, the necrosis vector headed towards V3, showing no increase in the R wave in V1 because it was being masked in the RS morphology because it normally exists in V3 (Figures 2B and 3). In contrast, the lateral infarction shows a vector of necrosis that explains the tall R wave in V1 (Figures 2C and 4).
Figure 2. A: the posterior wall (inferobasal) in its erroneously considered location. With this localization, the infarct vector in the inferior infarction (segments 4 and 10 in thin individuals) is directed towards V1 through V2 and explains the RS patent in said leads. B and C: real anatomical localization of the inferior wall (inferobasal) and lateral infarction. The infarction vector of the inferobasal and medial segments in thin individuals is directed to V3 through V4 and not toward V1, and can contribute to the RS patent that is seen in such leads. On the contrary, the infarct vector of the lateral wall is directed to V1 and explains the RS patent in this derivation.
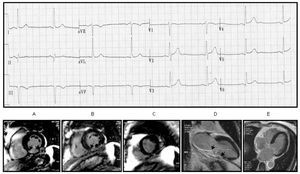
Figure 3. An example of an inferior myocardial infarction with compromising segments 4 and 10 (A and D), and an rS morphology in V1. There is no compromise of the lateral (E) or septal wall.
Figure 4. An example of a lateral myocardial infarction with an RS morphology in V1 but without a q in V5 through V6. The magnetic resonance images (A-F) show a compromise of the lateral wall (A-D and F) without a compromise of the inferior wall (E). The sagital section (E) shows an inferior wall that is not compromised. Lateral compromise is evident in all other sections.
In addition, it must be recognized that during decades we have made an anatomical as well as electrophysiological mistake. Durrer et al30 demonstrated that the zones that corresponded to the previously called posterior wall, now inferobasal or segment 4, are depolarized after a delay, after 40 ms, and therefore cannot originate a Q wave Q (or an R wave as a mirror image in V1 through V2) because the QRS complex has already started to register. In any case, a modification of the second half of the QRS complex will be registered with a distortion in it31 and/or a reduction in its voltage. We have found that the RS morphology in V1 is very specific in a lateral infarct (100%), though not very sensitive, because it is well known that lateral infacts do occur with an almost normal ECG or with qr or a small r in I, VL and V5 through V6 (Figure 4).
We also were able to prove22,23 that, in the case of an infarct secondary to the occlusion of the first diagonal artery, a low voltage QS was often produced in VL with an occasional "qr" in I but without a pathological Q in V6, that was not due to a high lateral infarct that was the ECG dogma that had been established for decades, but to a medial anterior infarct (Figure 5). That is explained because the high lateral zone is irrigated by the circumflex artery and, therefore, the occlusion of the diagonal cannot produce necrosis. On the other hand, the basal lateral infarct, as occurs in the infarction of the previously named posterior wall, cannot originate a Q wave due to delayed depolarization.
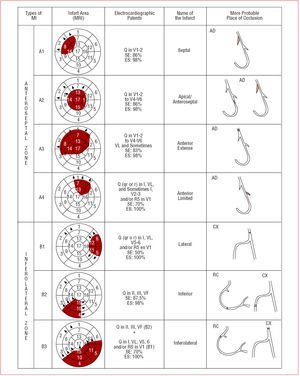
Figure 5. Localization and types of infarct (MI) according to the electrocardiographic patents (ECG). RC indicates right coronary; CX, circumflex; AD, anterior descending; MRI, magnetic resonance imaging.
Finally, we also demonstrated that Q wave infarcts in the precordial leads beyond V2 but without establishing the limiting derivation but without a Q wave in I and VL, corresponded to an apical infarct with a clear anterior affection (apical-anterior) (Figure 5).
How the New Q Wave Classification Was Originated
Because of our study of the ECG-MRI-G correlation showing a high agreement (88%),23 a new Q wave infarction classification has been reached and illustrated in Figure 5.
The 4 ECG patents of a Q wave infarction that we have defined in the anterior zone and the 3 in the inferolateral zone have correlated well with the areas of necrosis as detected by MRI-G (Figure 5).
All of these studies have served as a reflection to a group of experts named by the International Society of Holter and non-Invasive Electrocardiography (ISHNE), which after several meetings has elaborated a document that picks up all of these ideas with the contributions of its different members, and has recently been published as a Special Report in Circulation.25 At the same time, a committee named by the International Society for Computerized Electrocardiology has published32 in its recommendations for the interpretation of ECG that it prefers to wait before making these changes in terminology until there is new evidence that was not available when their report was published. They are aware though, of the fact that imaging techniques have shown a necessity for this change.22,23 Nonetheless, the Journal of Electrocardiology, the official organ of the International Society for Computerized Electrocardiology and the International Society of Electrocardiology, have published these new concepts and terminology on its cover, with an article and a cartoon in which the police give chase to a group of defenders of the term posterior infarction.33,34
We believe that all of this process of clarification allows us to reflect on the following:
1. The necessity for teamwork, in this case the better correlation between electrocardiographists and magnetic resonance experts.
2. Don´t believe in unmovable and life-lasting dogmas. It is possible that this new reality that now seems clear and evident is shown to be imperfect in the future.
3. One must travel to the source and consult the articles or books that have originated the dogmas. The article by Perloff6 is, in this sense, very demonstrative: a) the number of cases obtained from anatomopathologic study is very low, only 4; b) Perloff himself doubts about the localization of the so-called posterior wall when stating: "This dorsal portion of the left ventricle represents an area that is probably oriented posteriorly in the live subject"; and c) the impression given by the figure in which the location of the posterior infarction can be seen is that the heart is in a completely posteroanterior orientation. We have reviewed the scientific literature and all of the diagrams that make reference to this subject are variations of Perloffs' original in which the sagital plane is completely posteroanterior and not oblique, as in reality.
CONCLUSIONS
We believe that the body of doctrine is enough to reach the following conclusions: a) that the R wave in V1 is not originated by a posterior wall infarction, which generally does not exist, but in the lateral wall; b) that what many authors know as the lateral high infarction (Q in VL and occasionally I), is due to an infarct of the medial anterior wall; and c) that the name apical infarction (apical-anterior) is much better than the one of anteroseptal infarction for cases of infarction with QS in V1 through V4.
ACKNOWLEDGEMENT
We would like to thank the Imaging Unit of the Hospital de Sant Pau (Drs Pons, Carreras, Leta, and Pujadas) for their enthusiastic and useful help during this whole process.
Correspondence: Dr. A. Bayés de Luna.
Institut Català Ciències Cardiovasculars. Hospital de Sant Pau.
Sant Antoni M. Claret, 167. 08025 Barcelona. España.
E-mail: abayes@csic-iccc.org