INTRODUCTION
Myocardial diseases (MD) form an infrequently occurring heterogeneous group of potentially lethal abnormalities in children and young adults. Recent epidemiological studies have shown that dilated and hypertrophic cardiomyopathy are the most frequent morphological substrata of cardiomyopathy in children.1,2 Furthermore, MD have been associated with unexpected sudden death (SD) in apparently healthy people younger than 35 years old.3-9 Acute myocarditis and hypertrophic cardiomyopathy are the leading causes of SD in this age group. In addition, arrhythmogenic right ventricular cardiomyopathy/dysplasia has been recognized as a relatively frequent cause of SD in South European countries.4,9,10 In some cases, SD is the first manifestation of the disease, although sometimes the child or young adult has had some symptom during their lifetime.11 Some of these MD can be diagnosed during the patient's lifetime and thus SD avoided if treated. In addition to identifying high-risk patients, recognizing the factors that trigger acute ventricular arrhythmias is important in preventing SD due to cardiac causes.11,12
The actual incidence and distribution of cardiac SD by sex and age group in well-defined populations is poorly characterized. Only a few observational studies have assessed this problem in children and young adults. Most studies have been done in selected samples or in reference centers, with the consequent bias making it impossible to provide epidemiological data. A population-based observational retrospective study was carried out in children and young adults under 35 years old in the Spanish province of Biscay between 1991 and 2002 with the aims of assessing the epidemiological and clinical data on MD mortality and determining the causes of SD and non-sudden death (NSD).
PATIENTS AND METHODS
The study was done in Biscay (approximate population 1 200 000), an industrial province of the Basque Country, which has a homogeneous population. Foreigners form 0.7% of the total. All patients aged 1 to 35 years old who died due to an MD during the period ranging from 1 January 1991 to 31 December 2002 were included in this study. The cases were classified as SD or NSD as follows: SD was defined as that occurring naturally (non-violently), unexpectedly and instantaneously, or less than 6 h from the onset of premonitory symptoms or collapse, in a person in an apparently good state of health, not admitted to hospital, and while carrying out their habitual activities at the time of the fatal event.6,13 In line with legislation, a forensic autopsy is required for deaths due to violence or where crime is suspected. The latter include sudden unexpected natural deaths in nonhospitalized children and young people. The Biscay Forensic Pathology Service is in charge of investigating those occurring in Biscay.
In non-sudden natural deaths, legislation requires a medical death certificate signed by the physician who was treating the patient for a previously known disease. In Biscay, all such death certificates are supervised by the Forensic Pathology Service. In the case of the death of a child or young adult outside hospital, a preliminary investigation is done and, assuming that there are signs of violent death or an unexpected SD (for forensic purposes unexpected SD involves a potentially a criminal activity ), a forensic autopsy is requested and the medical death certificate is annulled (Figure 1).
Figure 1. Chart showing typical medical action taken after the death of a child or young adult in Biscay during the study period.
Subsequently, all medical death certificates and forensic autopsy reports are coded according to the underlying cause of death in the Mortality Registry of the Basque Country Autonomous Community, following the International Classification of Diseases (ICD-9) (Figure 1).
To achieve the aim of this work, Mortality Registry data were analyzed and the files of the Biscay Forensic Pathology Service were checked for the period 1991 to 2002, inclusive. All sudden deaths occurring in people aged 1 to 35 years old were examined. In all cases a complete autopsy and toxicological and histopathological studies had been carried out. The cardiac conduction system was studied via a simplified method previously described.14 Clinical data and the circumstances surrounding the death were also reviewed. This information was obtained from physicians' and forensic doctors' reports, official police statements and interviews with members of the dead person's family. It was not possible to review the physicians' reports on NSD patients.
Statistical Analysis
The total incidence rates and those for each sex and age group were calculated according to the population census data for Biscay province for the years 1991, 1996, and 2001. For the non-census years, year interpolations were calculated for the population for each sex and age group, assuming a linear yearly increase or decrease in the population. For the year 2002, the population projection was calculated assuming a growth rate equal to the 5 previous years.6 In the period 1991-2002, there was an average of 523 951 inhabitants aged 1 to 35 years old in Biscay.
In a previous study,6 where the incidence of SD was calculated by 5-year age-groups, we found that mortality was lowest in the pediatric age-group and that the figures increased progressively from 24 years old onward. Thus, in the present paper, we selected an initial group corresponding to the 5-year pediatric age group (children from 1 to 14 years old); the remaining population was classified into 2 groups, one corresponding to the 5-year adolescent/young adult group (from 15 to 24 years old) and the other to the older young adult group (from 25 to 35 years old).
The relative risk (RR) (and its 95% confidence interval [CI] of SD due to MD compared to NSD was calculated for the total and for the different age and sex groups. Similarly, the RR (and its 95% CI) of SD and NSD were compared between sex and between age groups (1-14 and 15-35 years old). Epi Info 6 (version 6.04) software was used. On the other hand, using the Fisher exact test, the difference in distribution of the absolute frequency of SD was calculated regarding the activity carried out at the time of death (physical activity vs another activity) between the SD due to MD groups and SD due to other causes. The significance level was set at P<.05.
RESULTS
Epidemiological and Demographic Data
According to Mortality Registry data, there were 8299 deaths in people aged 1 to 35 years old (6130 males and 2169 women) in Biscay from 1991 to 2002. The cause of death was MD in 40 cases. In 30 cases, a forensic autopsy for SD was carried out; although the physician had issued the medical death certificate for 1 of these cases, this was annulled by the forensic system as SD was suspected, and a forensic autopsy was done. In the other 10 cases, the appropriate medical death certificate was issued as no evidence indicative of SD due to suspected crime was found by the Forensic Pathology Service, and thus they were included in the NSD group. No case of NSD due to MD was investigated by the Forensic Pathology Service.
Of the 40 cases of death due to MD, 29 were male and 11 female, with an average of age of 25.30±7.17 years. All were Caucasian. The mortality rate due to MD was 0.64/100 000 inhabitants/year. This was higher for males than for women, and for the 15-24 and 25-35 year old age groups than for children 1-14 years old (Table 1). The RR of SD was significantly higher than that of NSD, especially between adolescents and young males (Table 1). The RR of SD was significantly higher in males than in females (3.17; 95% CI, 1.36-7.38) and in young adults than in children (11.39; 95% CI, 1.55-83.65).
Causes of Death
Analysis of the Forensic Pathology Service data showed 170 cases of SD in people aged 1 to 35 years old, 30 of which were due to MD (Table 2).
The MD were myocarditis, dilated cardiomyopathy, arrhythmogenic cardiomyopathy, hypertrophic cardiomyopathy, and idiopathic concentric left ventricular hypertrophy (CLVH) (Figure 2). Myocarditis was the most frequent cause of SD (33.3%), followed by arrhythmogenic cardiomyopathy (23.3%), whereas dilated cardiomyopathy was the most frequent cause of NSD (80%). Myocarditis was the most frequent cause in the 15-24 year old group (37%) and dilated cardiomyopathy in the 25-35 year old group (30%).
Figure 2. Distribution of myocardial diseases according to the manner of death.
Pathological Findings in the Sudden Death Group
Of the 10 cases of myocarditis, the left ventricle was affected in 3 cases, the right ventricle in 3, and both ventricles in 4. There were 4 cases of acute myocarditis (myocyte necrosis with lymphocytic inflammatory infiltrate) (curiously, in these cases pulmonary thromboembolism was also was found); 4 of subacute myocarditis (areas of myocyte necrosis replaced by young connective tissue and with scarce lymphocytic infiltrate); and in the other 2 cases, extensive interstitial fibrosis with patent coronary arteries was found, compatible with myocarditis sequelae.
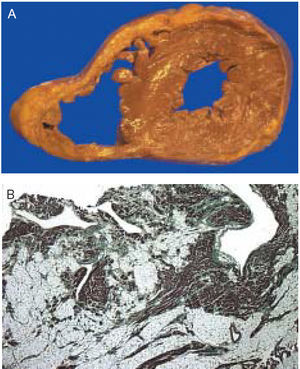
In the 7 cases of arrhythmogenic cardiomyopathy, extensive fibrofatty infiltration was found in the right ventricle (n=3) (Figure 3), in the left ventricle (n=2), or in both (n=2), without significant myocytic necrosis or coronary heart disease.10,15,16 In 6 cases there were morphological findings characteristic of hypertrophic cardiomyopathy, with hypertrophy of the anterior septum (type I) in 2, hypertrophy of the entire septum (type II) (Figure 4A) in 3, and hypertrophy of the septum and anterior wall of the left ventricle in 1 (type III).15 The maximum wall thickness of the interventricular septum varied between 20 and 40 mm and was ≥30 mm in 3 hearts. (It is worth recalling that the correspondence between wall width in diastole measured echocardiographically and at autopsy is low, since hearts are found in different degrees of contraction.) When the hypertrophic areas were viewed macroscopically, the myocardium had a whorled appearance and small scars were found. When viewed under microscope, all presented marked hypertrophy and disorganized myocytes, intramural coronary artery dysplasia, and fibrotic patches (Figure 4B), all of which are diagnostic lesions of hypertrophic cardiomyopathy.
Figure 3. A: arrhythmogenic myocardiopathy observed in a 31-year-old male who died suddenly while playing football. The right ventricle is dilated where the free wall is extensively substituted by adipose tissue. B: histologically, the myocardium is widely replaced by fibrofatty tissue (trichromic, Mag. ×4).
Figure 4. A: hypertrophic myocardiopathy. Cross section of the ventricular myocardium of a 33-year-old male who died suddenly. The thickness of the interventricular septum was 25 mm. The dark zones correspond to extensive areas of acute myocardial infarction. B: disorganization of myocytes with increased interstitial collagen, characteristic of hypertrophic myocardiopathy (trichromic, Mag. ×10).
In 3 cases, the only pathological finding was severe CLVH in the absence of hypertension, valvular, ischemic or congenital heart disease, the histopathological signs characteristic of hypertrophic cardiomyopathy, and of a family history of this disease. These findings are compatible with a diagnosis of idiopathic CLVH.15 Finally, there were 4 cases of cardiomyopathy with morbid obesity,16 of which 2 corresponded to CLVH and the other 2 to dilated cardiomyopathy.
Medical History, Prodromes, and Circumstances Surrounding the Death
Only in 3 cases of SD had the MD been diagnosed during the patient's lifetime. All of them had hypertrophic cardiomyopathy and were under cardiological treatment, and 2 of them were under pharmacological treatment (1 with verapamil and the other with amiodarone). Some cardiovascular symptoms and/or electrocardiographic abnormalities were recorded in 10 people during their lifetimes, but without the disease being diagnosed before death (Table 3); the main diagnosis was arrhythmogenic cardiomyopathy (n=5) and myocarditis (n=3). In the other 17 cases, SD was the first manifestation of the disease. Comorbid conditions were reported in 6 patients: 2 with myocarditis had received medical care for viral gastroenteritis and 4 presented morbid obesity. Six patients (20%) had prodromic symptoms, mainly syncope and chest pain.
There was premature SD in 3 patients relating to family background. Two young adults with arrhythmogenic cardiomyopathy in this series were brothers. After a detailed cardiology study was done in the 3 relatives of these brothers, the disease was diagnosed in 1 of them. In addition to this family, another four first-degree relatives of another 2 patients with arrhythmogenic cardiomyopathy were studied; in 2 (1 in each family) right ventricular dysplasia was diagnosed. Cardiological study of the family of 1 patient with hypertrophic cardiomyopathy did not reveal signs of the disease.
In 25 cases cardiopulmonary resuscitation (CPR) maneuvers were carried out. In 9, the ECG obtained during CPR showed ventricular fibrillation, in 8, asystole, and in 1, ventricular tachycardia that degenerated into ventricular fibrillation.
Arrhythmia triggering factors were reported in 11 cases. In 3 young people, toxicological analysis detected the presence of ethanol. In 7 cases death occurred during practicing a sporting activity (3 during football, 2 during the Basque game of pelota, 1 while cycling, and 1 during basketball). In 1 case, information was obtained regarding acute psychological stress in the instant prior to death. Of the arrhythmogenic cardiomyopathy cases, 71% died during a sporting activity. Sudden death related to a sports activity occurred in 23.3% of the cases of MD (7 out of 30), compared to 9.3% (13 out of 140) of the remaining causes of SD (P=.05).
In 7 cases, the death was not witnessed and occurred in the bed, probably while sleeping. In 21 cases, death occurred within 15 min (almost instantly) and in 2 cases between 15 and 60 minutes. In 47% of cases the death occurred outside a hospital and 53% were admitted to the emergency ward in a state of cardiorespiratory arrest.
DISCUSSION
The incidence of mortality due to MD in people aged 1 to 35 years old is low and the risk of SD significantly higher than NSD. Thus, it is important to include forensic case studies, otherwise the incidence would be underestimated. In the present study, 75% of all the deaths due to MD were sudden. On the other hand, in a previous study conducted in Biscay with the same type of population, we found that the percentage of SD in relation to total mortality from natural causes was 4.5%, and in the group VII diseases of the ICD-9 (circulatory system) this was 22.6%.6 The incidence of SD due to MD found in Biscay is within the range described in other studies.3,5,7 In addition, the relative risk (RR) of SD is significantly higher in males, adolescents, and young adults compared to women and children. It is worth highlighting the low frequency of SD du e to MD in children 1-14 years old, which could indicate that cardiomyopathies (above all hypertrophic and arrhythmogenic) are clinically silent until adolescence, when they manifest as SD. These findings indicate that the main effort in preventing SD should focus on adolescent males and young adult males.
Unlike the other MD, where death is mainly sudden and is caused by an arrhythmic mechanism, in dilated myocardiopathy NSD predominates, indicating that in this case death occurs in a more advanced period of the disease due to congestive heart failure.17
Myocarditis is one of the leading causes of SD in children and young adults,9,11 as our work also clearly shows. It is worth noting that the 4 cases of acute myocarditis also presented thrombi in the pulmonary arteries. This finding should be investigated in the future, although some studies have pointed out that acute viral myocarditis involves a considerable risk of thromboembolism.18
Arrhythmogenic cardiomyopathy, hypertrophic cardiomyopathy, and idiopathic CLVH8,16,19 are well-known causes of SD during sports activity, with geographical variations among them: the second is especially frequent in North America8 and the first, in Southern Europe.9,10,19 Arrhythmogenic cardiomyopathy is a disease of unknown origin and different theories have been considered, such as genetic and inflammatory ones.12,20 In some patients it could represent a form of myocarditis with scarring.
Idiopathic CLVH is a clinical condition where the heart is morphologically very similar to athlete's heart. Distinguishing between them is fundamental in professional athletes, but is not easy,8 as shown in the present series (Table 3). It has been suggested that there could be a non-familial variant of hypertrophic cardiomyopathy or a form of hypertrophic cardiomyopathy without typical morphological expression.16
Preventing deaths due to MD in children and young adults is a difficult task, as a high percentage occur suddenly and without the subject having experienced previous cardiovascular symptoms.11 One of the main findings in the study is the relatively high percentage of people with cardiovascular symptoms or electrocardiographic abnormalities before death, where the disease had not been diagnosed during life, although all the patients had been examined by a physician. It may have been possible to prevent death in some of them, especially in cases of arrhythmogenic cardiomyopathy and myocarditis. However, both diseases can be difficult to diagnose while the patient is alive. In contrast, half of the cases of hypertrophic cardiomyopathy had been diagnosed, which shows that the SD risk stratification is not easy due to its clinical heterogeneity. Both arrhythmogenic and hypertrophic myocardiopathy and are becoming an emerging indication for using an implantable cardioverter defibrillator.20 This could have been effective in 2 of our cases. Our results agree with the well-known greater risk of SD in people with morbid obesity.21 The prevention and treatment of obesity could be of interest regarding reducing mortality due to MD.
Certain triggering factors can precipitate lethal arrhythmias in a vulnerable myocardium and, among these, vigorous physical activity is the most important in the context of MD, especially in arrhythmogenic cardiomyopathy.9,10,19 Thus, in the young men diagnosed with this disease, the practice of vigorous sports activities12 should be advised against. In line with the protocol of the American Heart Association,22 at least 3 of our patients should have received this advice until a detailed cardiological examination had been done. One of the patients with myocarditis died during a cycling event, which supports the contraindication of sports activity during the acute phase of the disease.8 Although hypertrophic cardiomyopathy has been pointed out as the leading cause of SD in young adult athletes,8 none of the subjects diagnosed with this in the present series died during sports practice. In addition, to the best of our knowledge, no cases of SD during the Basque game of pelota have been published.
Alcohol intake can induce malignant ventricular arrhythmias in susceptible myocardium.23 Ventricular fibrillation is the rhythm most frequently found in SD,12 which we also observed. Thus, efforts should be made to achieve early defibrillation in cases of outside-hospital cardiac arrest, especially in sports centers.
We should mention some limitations of the present study. Although the clinical history of the cases where the medical death certificate had been issued were not available, we assumed that they did not fulfill the criteria for SD, since they involved in-hospital or outside-hospital deaths but which had undergone forensic examination when they occurred. As pointed out in other SD studies in Europe,7,13,24-26 it is highly unlikely that a medical-forensic investigation would not be carried out in the case of an outside-hospital SD in a child or young adult. On the other hand, the different distributions of MD in SD and NSD groups serves to give additional support to the reliability of the present results.
Clinical Implications
In all cases of SD in children and young adults, a forensic autopsy should be carried out for 2 fundamental reasons: on the one hand, it offers useful and reliable information for epidemiological and preventive studies; and on the other, since some MD are hereditary, a precise diagnosis can make it possible to prevent death in family members. In 3 of the families studied in our series, other asymptomatic members were diagnosed with arrhythmogenic cardiomyopathy. Genetic studies into MD are permanently ongoing.27 One of the aims is to find genetic mutations associated with a high risk of SD.27 Thus, it would be desirable that in the near future genetic studies are included in the autopsy protocol. On the other hand, it seems that death could have been prevented in some cases via early diagnosis of the disease, and by identifying and modifying the risk factors of the disease as well as the factors triggering SD. Finally, it would be useful to implement effective resuscitation programs for victims of cardiac arrest.
ACKNOWLEDGMENT
We express our gratitude to Dr Marta Pulido for her editorial support.
Correspondence: Dr. B. Morentin.
Servicio de Patología Forense de Bizkaia. Instituto Vasco de Medicina Legal.
Barroeta Aldamar 10, planta 1. 48001 Bilbao. España.
E-mail: morentin.b@aju.ej-gv.es
Received April 25, 2005.
Accepted for publication December 15, 2005.