Keywords
INTRODUCTION
Type 2 diabetes mellitus (DM) has become one of the most severe health problems of our time. The situation in Spain is worrying: the various cross-sectional studies carried out in this country show that the prevalence of DM has increased over the last decade. Currently, the estimated prevalence of type 2 DM in the adult population is 10%-15%.1,2 More worrying still is the fact that at least half of these persons are unaware that they have the disease (undiagnosed or unknown DM).1,2 This is due to the fact that this form of diabetes often remains undiagnosed for many years because the hyperglycemia develops gradually, with a long asymptomatic, preclinical phase. Nevertheless, chronic hyperglycemia, even in the absence of symptoms, is associated with an increased risk of diabetic microangiopathy and cardiovascular disease (CVD), which can even start with degrees of dysglycemia below current diagnostic levels of DM.3 Most studies on CVD, death and health costs related with DM are based solely on the proportion of diagnosed or known DM. Less is known about the impact of persons with unknown or undiagnosed DM or of the early stages of carbohydrate metabolism disorders. The demonstration of an increase in mortality in these stages could reinforce the importance of screening programs and early intensive treatment in these persons.
The aim of this study was to evaluate the risk of death in persons with diagnosed DM, undiagnosed DM, and prediabetes as compared with persons with normoglycemia in a representative cohort of the general population from the province of Asturias, in the north of Spain.
METHODS
Asturias Study
The Asturias Study is a population-based prospective cohort study of DM and cardiovascular risk factors that is taking place among the whole population of the province of Asturias, in northern Spain.4-7 The first phase took place over the years 1998-1999 and was designed to determine the prevalence of type 2 DM, both diagnosed and undiagnosed, and of prediabetes in the population of Asturias, which is 1 073 761 inhabitants, mostly Caucasian. About half the population live in urban areas. The sample was selected using a 2-stage cluster sampling technique: 15 basic health areas were randomly selected from among the 76 in Asturias, with a probability proportional to the number of health cards from persons aged 30 to 75 years in each area. A computer program was then used for the random selection of 125 persons in each basic health area. The final sample selected was 1875 persons. A total of 87 persons were excluded for various reasons (type 1 DM, pregnancy, severe disease, hospitalization, treatment with hyperglycemic drugs). Another 162 were excluded because their contact data were not complete. The final sample was 1626 persons, of whom 1034 (63.6%) participated in the study.
The study was approved by an Ethics Committee of the Principality of Asturias Health Service and all the participants gave their informed consent.
All the participants completed a health questionnaire, which included data on demographics, smoking, physical activity, socioeconomic status, and a family history of DM.
The height and weight were measured with the participant in light clothing and without shoes, and the BMI was calculated (weight in kilograms divided by the square of the height in meters). The blood pressure (BP) was measured using a digital sphygmomanometer (OMROM MX3, OMROM Healthcare, Tokyo, Japan) with the person seated and at rest. The mean of 2 BP measurements, taken 1-2 min apart, was used for this analysis.
All the participants, except those with diagnosed DM, underwent an oral glucose tolerance test (OGTT), with extraction of venous blood at baseline and after 2 h, in accordance with the recommendations of the World Health Organization8; 15 min after each extraction the blood was centrifuged in situ using a portable centrifuge. The samples were transported daily in a portable fridge (4-6°C) for processing at the Clinical Biochemistry laboratory of the Hospital Universitario Central de Asturias. Measurements were made of blood glucose fasting and after the OGTT (glucose-hexokinase enzyme method, Hitachi 747 analyzer, Roche Diagnostics, Mannheim, Germany). Measurements were also made of concentrations of total cholesterol, high-density lipoprotein cholesterol (HDL-C), triglycerides (colorimetric enzyme method, Hitachi 747 analyzer, Roche Diagnostics, Mannheim, Germany), low-density lipoprotein cholesterol (LDL-C) (Friedewald equation),9 and glycohemoglobin (HbA1c) (high power liquid chromatography [HPLC], Jokoh HS-10 analyzer). The participants were notified by letter of the results of their OGTT, and those who had undiagnosed DM or glucose intolerance were advised to contact their primary care physician for follow-up and control.
Follow-up and identification of Fatal Events
In December 2004, prior to starting the second phase of the Asturias Study, the vital status was verified of the whole cohort that participated in the first phase of the study (1998-1999). Data obtained from the health card provided by the central services of the Principality of Asturias Health Service were used to record all deaths and their dates. This information was verified by checking the medical registries of the whole cohort; 19 persons who had moved their residence away from Asturias before the start of the second phase were excluded from this re-evaluation, as their vital status could not be verified. In total, the registry included 1015 persons, with a follow-up time of six years (December 1998 to December 2004).
The cause of death was determined by systematic review of the clinical records, both at their health centers and in the corresponding referral hospital. If necessary, the cases were commented on in person with the primary care physician. Additional data from death certificates were also available for 93% of the cases. The cause of death was coded according to the IDC-10 of the World Health Organization.10 Cardiovascular death was defined with codes I00-I99 ("diseases of the circulatory system") or R96 ("other sudden death, cause unknown"), because sudden death is generally of cardiovascular origin.11 Death due to cancer was defined with the codes C00-D48 ("neoplasms").
Statistical Study
All the statistical analyses were done with SPSS 12.0 (SPSS, Chicago, IL) and Epibasic 1.0 (University of Aarhus, Nordre Ringgade, Denmark). The reported P values are based on a 2-tailed test with a limit of statistical significance of P<.05.
Evaluation of the risk for death in the different categories of dysglycemia was done by classifying the persons included in the registry of deaths into four groups, according to the results of the OGTT during the first study (World Health Organization 1999 criteria)9: normoglycemia (fasting glycemia <110 mg/dL and 2 h post OGTT glycemia <140 mg/dL), prediabetes (fasting glycemia 110-126 mg/ dL and/or 2 h post OGTT glycemia 140-200 mg/ dL), undiagnosed DM (fasting glycemia ≥126 mg/ dL and/or 2 h post OGTT glycemia ≥200 mg/dL), and diagnosed DM.
Comparisons between groups for quantitative variables were done with an analysis of variance (ANOVA). Multiple comparisons between pairs were adjusted with the Bonferroni test. The χ2 test was used for comparison of proportions.
The person-years of follow-up were estimated for each group, as was the number of events (deaths), calculating the mortality rates for each 1000 inhabitant-years (95% confidence interval [CI]), which was adjusted for age and sex by the direct method, using the age and sex structure of the normoglycemic group as the reference.
Cox regression analysis was used to analyze the accumulated impact curves and the corresponding relative risks (RR) of death, adjusted for age and sex and multivariable (adjusted for age, sex, BMI, systolic BP, diastolic BP, smoking, LDL-C and the prior presence of CVD) in the different groups.
RESULTS
A total of 42 deaths were recorded during the follow-up period. The causes of death were: cardiovascular origin, 17 (40.5%); cancer, 19 (45.2%); other causes, 6 (14.3%).
Table 1 shows a comparison of the metabolic and cardiovascular risk parameters according to the different clinical categories of dysglycemia during the first phase of the study (1998-1999). The age increased with the category of dysglycemia, and was maximum in the group with diagnosed DM. The percentage of men was higher in all the groups as compared with the reference group that had normoglycemia. The cardiovascular risk profile worsened progressively from normoglycemia to prediabetes to DM in most of the study parameters, including systolic BP, diastolic BP, BMI, HDL-C, and triglycerides. Those persons with undiagnosed DM had similar figures for systolic BP, diastolic BP, HDL-C, and triglycerides to the persons with diagnosed DM. However, persons with diagnosed DM had similar, or even lower figures for total cholesterol and LDL-C to the general population without dysglycemia, values that were maximum in the group with prediabetes and undiagnosed DM. A possible explanation for this is the greater use of lipid-lowering drugs in persons with diagnosed DM. Likewise, there was a progressive increase across the groups for the figures of fasting glycemia, 2 h post OGTT glycemia and HbA1c. Of note was the fact that the mean levels of HbA1c in the group with undiagnosed DM were almost within the range of normality.
Around 10% of the persons with prediabetes or undiagnosed DM already had some symptom of CVD at the start of the study, which was only present in 2.1% of the general population with normoglycemia (P<.01). In the group with diagnosed DM, 17.4% had CVD at the start of the study.
Only 39.1% of the diagnosed diabetic patients were taking treatment with hypertension drugs and 15.6% with lipid-lowering drugs.
Table 2 shows the number of deaths, the mortality rates for each 1000 inhabitant-years adjusted for age and sex and the risk of death adjusted for age and sex and multivariable in the different groups.
Both those with diagnosed DM and those who had undiagnosed DM had a risk of mortality almost 3-fold greater than persons with normoglycemia in the analysis adjusted for age and sex; these levels remained just slightly lower after the multivariate analysis. The group with prediabetes also had an increase in mortality as compared with the control group, although the difference was not statistically significant. Using the American Diabetes Association 2003 criteria for the diagnosis of prediabetes showed the relative risk of death to be similar in the model adjusted for age and sex: RR=1.5 (0.7-3.3), and slightly lower in the multivariate model: RR=1.3 (0.5-3.0) as compared with the normoglycemic group. The risk of death in those with DM, both diagnosed and undiagnosed, versus those with normoglycemia was 2.9 (1.4-5.9) in the model adjusted for age and sex, and 2.6 (1.2-5.7) in the multivariate model.
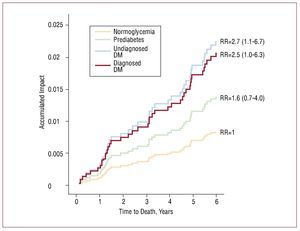
Figure 1 shows the accumulated mortality curves for the four groups. The mortality curves in the groups with diagnosed DM and undiagnosed DM were practically the same.
Figure 1. Accumulated all-cause mortality curves for the groups with normoglycemia, prediabetes, undiagnosed diabetes mellitus, and diagnosed diabetes mellitus (model adjusted for age, sex, body mass index, diastolic blood pressure, systolic blood pressure, smoking, low-density lipoprotein cholesterol, and presence of previous cardiovascular disease).
The specific analysis for cardiovascular death showed the same trend, although this analysis was rejected because of the low number of cases available.
DISCUSSION
The main finding of this study was that both persons with diagnosed DM and those with undiagnosed DM had a risk of death 2.5 to 3 times greater than those with normoglycemia, a risk that was similar in both groups. We also found an excess mortality in persons with prediabetes, though the difference was not statistically significant.
The data from this registry are alarming, as the different cross-sectional studies that have been carried out in Spain (see the "Introduction") suggest that at least half those persons with DM remain undiagnosed whilst the disease remains asymptomatic, even over many years. Diagnosis during this preclinical phase is only possible by screening or incidentally. The fact that those persons with undiagnosed DM have a significantly higher risk of death than the control group with normoglycemia and a similar risk to those with diagnosed DM underlines the importance of detection in these persons.
Of note, though, is the fact that, unlike other diseases that require a screening test and a diagnostic test, for persons with DM the same test can be used for both screening and diagnosis of the disease, ie, the OGTT. Furthermore, this screening has the added advantage of being able to diagnose persons who have prediabetes, and who could thus benefit from possible preventive strategies.
Admittedly, it is true that no direct evidence exists that early detection and multifactorial treatment of persons with asymptomatic DM results in an improvement in prognosis.12 However, it is also true that the lack of evidence for this is due to the absence of studies investigating this hypothesis and, for obvious ethical reasons, it is unlikely that any rigorously controlled studies will be carried out to provide any direct proof. What we do have, though, is the indirect evidence that aggressive multifactorial treatment aimed not only at reducing the HbA1c, but also at lowering LDL-C, BP, and anti-platelet aggregation, produces effective reductions in vascular complications and the risk of death in persons with type 2 DM.13,14 Thus, there appears to exist no reason for supposing that early detection and aggressive intensive therapy of asymptomatic persons should not produce similar results.
This intensive therapy was not optimal in our cohort of patients with diabetes, not even in the case of the group with diagnosed DM. As can be seen from Table 1, the mean values of the LDL, as well as the systolic BP and the diastolic BP and the percentage of persons who were receiving treatment with hypertension drugs and lipid-lowering drugs were all well below the optimal objectives for control in patients with type 2 DM according to current clinical practice guidelines.15 It is possible that aggressive treatment of cardiovascular risk factors during the follow-up might have led to a lower risk of death. In the group of persons with undiagnosed DM, intensive treatment of cardiovascular risk factors was even lower; in fact, during the re-evaluation of the cohort, we found that a high number of these participants (around 40%) had not even told their primary care physicians about the results of the OGTT, and there was no record in their clinical histories. At the end of the follow-up period, the percentages of patients receiving hypertension drugs, lipid-lowering drugs and anti-platelet aggregators were 64%, 36%, and 44% in the group with diagnosed DM, as compared to 46.3%, 22%, and 7.3%, respectively, in the group with undiagnosed DM (data corresponding to 700 participants in the second phase of the Asturias Study, 2004-2005). This could account for the fact that the excess mortality in this group was similar to that of the group with diagnosed DM, even though their age, HbA1c levels and the initial presence of CVD were all lower. This study was not designed as an intervention study, but rather an observation study, and what we saw may reflect the true situation facing us: it is estimated that fewer than half of those persons who have a cardiovascular risk factor are aware of their diagnosis, that fewer than half of these are receiving non-specific treatment and, that fewer than half of those who are receiving treatment reach the therapeutic aims recommended by the clinical practice guidelines.16
These data have important public health implications. The impact of persons with undiagnosed hyperglycemia on CVD and overall risk of death in our populations is an undervalued problem, the dimensions of which could surpass any estimate. The Euro Heart Survey on Diabetes and the Heart, in which 4196 patients with coronary disease were recruited from 110 centers in 25 countries, produced convincing findings: 22% of patients seen for an acute coronary syndrome were found to have undiagnosed DM after undergoing an OGTT and 36% had impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT); normoglycemia is less common in these patients than dysglycemia. The overall proportion of persons with DM, both diagnosed and undiagnosed, was estimated to be around 45%.17 Studies carried out in stroke patients have found similar results, with just a minority of patients showing normoglycemia after undergoing an OGTT.18 The impact on overall mortality is unknown.
In Spain, the only previous reference to the evaluation of the risk of death in persons with undiagnosed DM and prediabetic dysglycemia is the Lejona Study. Ten years after the initial study, the vital status of the cohort was evaluated. An excess all-cause mortality was found in patients with diabetes that was almost twice that of persons with normal glucose tolerance, an excess risk that proved to be mainly due to those persons with undiagnosed DM.19
Outside Spain, we can find several studies. Shaw et al20 analyzed longitudinal studies from the islands of Mauritius, Fiji, and Nauru, and found a risk for cardiovascular death in persons with undiagnosed DM that was 2-fold greater than in persons without DM only in those who had 2 h post-OGTT glycemic levels ≥200 mg/dL but not for persons with a fasting glucose of ≥126 mg/dL and 2 h post-OGTT <200 mg/dL.
A review of the second national NHANES survey in the United States, which included 3092 persons aged 30 to 74 years, found a relative risk of death of 2.26 (1.78-2.87) in persons with diagnosed DM, 1.76 (1.17-2.66) in persons with undiagnosed DM and 1.37 (1.05-1.79) in persons with IGT, compared with the control group with normoglycemia. The relative risks for cardiovascular death were similar.
The most conclusive data can be found in the DECODE study, which included 29 714 persons aged 30-89 years from 22 European cohorts. The study found an increase in the risk for all-cause mortality and cardiovascular mortality in persons with undiagnosed DM, especially for persons with 2 h post-OGTT glycemic levels ≥200 mg/dL, who had a relative risk of death that was similar to those persons with diagnosed DM.3
Our study has certain limitations: the main one is the low number of fatal events available for the analysis. The Asturias Study was designed as a cross-sectional study to estimate the prevalence of type 2 DM and IGT, as well as the proportion of persons with undiagnosed DM in the population of Asturias, and the sample size was sufficient for these estimations.4 Estimation of the risk of death in the different groups would probably have required a larger cohort or longer follow-up period in order to obtain greater precision in the results. Additionally, participation in the initial field study was not complete (64% of the persons initially selected). This rate of participation might affect the representativity of the sample and the extrapolation to the general population of the data obtained. Nevertheless, in spite of these limitations, inherent to the study design itself, we consider that the study presents the important advantage of analyzing a representative sample of the general population from the whole province, including both rural and urban areas, with a complete initial evaluation by means of an OGTT, which gave us the unusual opportunity of being able to evaluate mortality in a number of persons with prediabetes and undiagnosed DM, a fact that was almost unprecedented in Spain. Despite the relatively low number of fatal events studied, the data are concordant with earlier studies, which reinforces our results.
CONCLUSIONS
In summary, this study found a risk of mortality in persons with diabetes that was 2.5-3 times higher than in persons with normoglycemia, with a similar risk in both persons with diagnosed and undiagnosed diabetes. These results, which agree with those of previous studies, reflect the importance for public health of detection and intensive treatment of these persons.
ACKNOWLEDGMENTS
The authors wish to express special thanks to all those Asturian persons who participated in the 2 studies, without whose collaboration it would have been impossible to carry out. Also, to the primary care teams of the Basic Health Areas selected. To Ismael Huerta, Shura Rozada, and Enrique Bustillo. To the Servicio de Bioquímica Clínica of the Hospital Universitario Central de Asturias and to the Endocrinology group of Asturias.
The Asturias Study was undertaken with finance from the grant FIS 98/0462, a grant from the Consejería de Salud of the Principado de Asturias and a Pfizer grant. The CIBER de Diabetes y Enfermedades Metabólicas Asociadas (CB07/08/0019) is an initiative of the Instituto de Salud Carlos III.
ABBREVIATIONS
CVD: cardiovascular disease
DM: diabetes mellitus
OGTT: oral glucose tolerance test
Correspondence: Dr. S. Valdés.
Servicio de Endocrinología y Nutrición. Hospital Universitario Carlos Haya.
Pl. del Hospital Civil. 29009 Málaga. España.
E-mail: Sergio.valdes@hotmail.es
Received November 17, 2008.
Accepted for publication February 11, 2009.