This study aimed to describe the cardiovascular risk profile of working young adults from Spain and its association with lifestyle.
MethodsParticipants (18-30 years) were recruited from a nationwide cohort of economically active adults insured by a large occupational risk prevention company, with data obtained from routine medical assessments. The participants were categorized as having an “unhealthy” cardiovascular risk profile based on the presence of prediabetes/diabetes, prehypertension/hypertension, or hypercholesterolemia, or a “healthy” profile if these conditions were completely absent. The association with lifestyle factors (weight, physical activity, sleeping characteristics, alcohol consumption, smoking) was assessed.
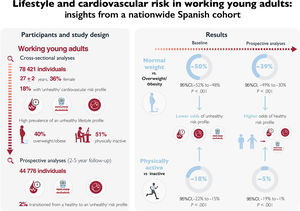
ResultsA total of 78 421 young adults (27±2 years, 36% female) were evaluated at baseline. The “unhealthy” cardiovascular risk profile was prevalent (18%) and inversely associated (OR, 0.64; 95%CI, 0.57-0.80) with an optimal lifestyle (normal weight, regular physical activity, no drinking/smoking, and good sleep). The latter condition was found in only 3.5% of the participants. On the other hand, prospective analyses in 44 776 participants (median follow-up=2 [range 2-5] years) showed that 2.0% transitioned from a “healthy” to an “unhealthy” profile. Being physically active (OR, 0.95; 95%CI, 0.81-0.99) and having a normal weight (OR, 0.61; 95%CI, 0.51-0.70) were associated with a lower likelihood of this transition. No consistent associations were found for other lifestyle factors.
ConclusionsThe prevalence of cardiovascular risk factors is high in economically active young Spanish adults. An unhealthy cardiovascular risk profile is inversely associated with an optimal lifestyle, but the latter is highly infrequent in this population.
Keywords
The prevalence of cardiovascular risk factors has risen in young adults in the last 2 decades, which contrasts with a decreasing trend in people aged more than 50 years.1 Notably, the incidence of cardiovascular events (eg, stroke, myocardial infarction) has increased considerably in people younger than 30 to 40 years in the USA and Europe.2,3 Primary cardiovascular prevention has therefore become a priority not only in middle-aged or older adults, but also in younger individuals.1
There have been major changes in lifestyle-related factors over the last few decades, particularly in younger adults, including an increase in the rates of obesity and physical inactivity,1 both of which are also cardiovascular risk factors per se.4,5 Indeed, the prevalence of overweight and obesity in young European adults (30 years or less) is currently 23.4% and 8.2%, respectively,6 and is even higher in the USA (where the prevalence of obesity in people younger than 40 years increased from 30% to 40% from 2007 to 2018).7
Physical inactivity starts early in life. A recent analysis of cross-sectional survey data (from 146 countries) found that more than 80% of adolescents failed to meet international recommendations for physical activity,8 and the data for people aged 16 to 30 years suggested a decline in the levels of moderate-to-vigorous physical activity during the transition from adolescence to adulthood.9 Other lifestyle factors can also contribute to the upward trend of cardiovascular risk in young adults, including tobacco use,10 alcohol consumption,10 and inadequate sleep.11
The main aim of the present study was to determine the prevalence and incidence of cardiovascular risk factors, as well as their association with lifestyle, in economically active young adults (18-30 years) from Spain.
METHODSParticipants and study designThe present study followed both a cross-sectional and a prospective design and adhered to the “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) reporting guidelines. Participants were recruited from a nationwide cohort of active Spanish adults (aged 18-65 years) insured by a large occupational risk prevention company.12 The participants underwent routine (∼1 each year) medical examinations between 2012 and 2016 by this company. All individuals of the cohort aged 18 to 30 years were identified, and cross-sectional analyses were performed using the first available medical examination (baseline) during the study period. Prospective analyses were also performed (from baseline to the last available examination) in those participants with at least 2 assessments who were free of cardiovascular risk factors at baseline. Participants provided oral consent, and the local ethics committee approved the protocol (CEI20-004). All procedures were performed in accordance with the Declaration of Helsinki and its later amendments. Individual data cannot be made available to other researchers as per ethics regulations.
MeasuresAll variables were assessed and registered by the physicians of the insurance company. Demographic/descriptive variables assessed at baseline included age, sex, and socioeconomic status. The latter–a combination of occupation variables (including professional activity and professional status of the household)–was obtained from the Spanish census. Thus, a territorial indicator was assigned to each record by merging census street map and territorial indicator information (Spanish census and individuals’ postal code), as reported elsewhere.13
We also assessed lifestyle-related factors at baseline. The physician used standard procedures to assess weight and height, which were measured to the nearest 0.1kg and 0.1cm to calculate body mass index (BMI). Participants were categorized as having normal weight (BMI below 25.0kg/m2), overweight (BMI between 25.0 and 29.9kg/m2), or obesity (BMI equal to or over 30.0kg/m2). Self-reported levels of leisure-time aerobic physical activity were assessed as explained elsewhere.12 Briefly, participants completed a questionnaire assessing the frequency and intensity of aerobic activities during a typical week, and were considered physically “active” or “inactive” based on minimum World Health Organization determined recommendations for aerobic physical activity (at least 150 or 75minutes per week of moderate or vigorous activity, respectively, or a combination thereof).14 Participants also completed a questionnaire detailing self-reported sleep duration (“normal” [6 to 9hours/d] or “abnormal” [less than 6 or more than 9hours/d]) and quality (“restful” or “unrestful”, and whether they had difficulties falling asleep).11 Those reporting abnormal sleep duration, unrestful sleep and/or difficulties falling asleep were considered as having “poor” sleep, whereas those with normal sleep duration, restful sleep, and no difficulties falling asleep were considered as having “good” sleep. Smoking habits and alcohol intake (1 drink per day or more) were assessed through a personal interview with the physician.15
The presence of cardiovascular risk factors was assessed both at baseline (for all participants) and at the end of the follow-up (for those participants included in prospective analyses) as explained elsewhere.16 The physician in charge assessed the presence of prediabetes (fasting glycemia 100-125 mg/dL), diabetes (on medication or fasting glycemia higher than 125mg/dL), hypercholesterolemia (on medication or total blood cholesterol over 239mg/dL), prehypertension (office systolic/diastolic blood pressure 130-139/85-89mmHg) and hypertension (on medication or office systolic/diastolic blood pressure ≥ 140/90mmHg). Participants showing none or 1 or more of the aforementioned 5 risk factors were categorized as having a “healthy” or “unhealthy” cardiovascular risk profile, respectively.16
Statistical analysesResults are expressed as No. (%) or mean±standard deviation. Logistic regression analyses were performed to determine the independent association between each lifestyle factor and the prevalence (cross-sectional analysis) or incidence (prospective analysis) of cardiovascular risk factors. Analyses for each risk and lifestyle factor were adjusted for age, sex, socioeconomic status, calendar year (2012-2016), and length of follow-up (expressed in its logarithmic form), as well as for the remainder of risk and lifestyle factors (eg, the analysis of physical activity, prehypertension and hypertension was adjusted for prediabetes, diabetes and hypercholesterolemia, as well as for BMI category, sleep, and drinking and smoking habits). Missing data were not imputed for prospective analyses in participants with only 1 (baseline) assessment. In this effect, elucidating the missing data pattern in a given cohort can be challenging, as 3 different scenarios are possible that are difficult to discern objectively: a) missing data completely at random (no relationship between the missingness of the data and any values, observed or missing); b) at random [presence of a systematic relationship between the propensity of missing values and the observed (but not the missing) data]; or c) not at random (also known as nonignorable missingness, ie, the data is neither missing completely at random nor missing at random, with the value of the missing variable related to the reason it is missing).17 In this effect, the exploration of potential associations between absent data variables, complemented by thorough visual examination, can help to formulate informed hypotheses regarding the characteristics of the pattern of missing data. Consequently, we used the phi correlation coefficient (also known as Cramér's V and denoted as φc) to explore potential associations among missing variables, alongside visual examination (to explore whether any of the patterns displayed a higher degree of repetition). Statistical analyses were done with Stata 14.0 (StataCorp LLC, USA) and the level of significance was set at .05.
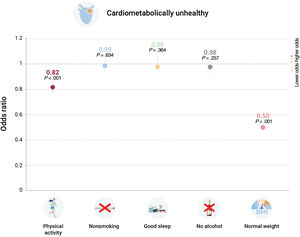
RESULTSCross-sectional analysesOur analyses were based on 78 421 young adults (27±2 years, 36% female) with complete data (table 1). The first main finding was that prevalence of an “unhealthy” cardiovascular risk profile was high (18%) at baseline. Approximately half of the participants was physically inactive (51%), and a similar proportion was overweight/obese (40%). This “unhealthy” subgroup was older and had a higher proportion of men compared with their healthy peers (table 1). The second main finding was that the unhealthy risk profile was inversely associated (odds ratio [OR],−36%; 95% confidence interval [95%CI],−43% to−20%) with an optimal lifestyle (normal weight, regularly active, no drinking/smoking, good sleep) compared with not having at least 1 “healthy” lifestyle factor. Nevertheless, only a minority (3.5%) of the participants had an optimal lifestyle. Being physically active (OR,−18%; 95%CI, −22% to −15%), and, particularly, having a normal weight (OR, -50%; 95%CI, −52% to −48%) was individually associated with a lower likelihood of having an unhealthy risk profile; no association was found for the remaining lifestyle factors (figure 1 and table 1 of the supplementary data). Subanalyses based on specific cardiovascular risk factors confirmed that having a normal weight was associated with a much lower prevalence of prehypertension (OR, -37%; 95%CI, −40% to −15%), hypertension (OR, −67%; 95%CI, −71 to −66%), prediabetes (OR, −39%; 95%CI, −43% to −34%), diabetes (OR, −18%; 95%CI, −35% to −5%), and hypercholesterolemia (OR, −47%; 95%CI, -49% to −45%), whereas an inverse association (albeit of lower magnitude) was also found between being physically active and the prevalence of hypertension (OR, −12%; 95%CI, −19% to −4%), prediabetes (OR, −17%; 95%CI, −23% to −10%), diabetes (OR, −26%; 95%CI, −42% to −3%), and hypercholesterolemia (OR, −14%; 95%CI, −19% to −9%) (figure 2 and table 2 of the supplementary data). Nonsmoking was also associated with a lower risk of hypertension (OR, −11%; 95%CI, −18% to −2%), prediabetes (OR, −9%; 95%CI, −15% to −3%), and no alcohol consumption with a lower risk of prediabetes (OR, −8%; 95%CI, −15% to −1%) but no significant associations were found for the remaining cardiovascular risk factors (figure 2 and table 2 of the supplementary data).
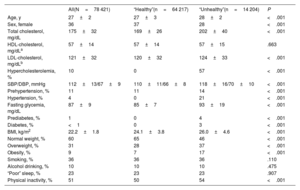
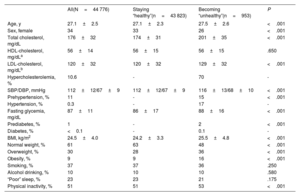
Descriptive characteristics of study participants (economically active young adults, aged 18-30 years) at baseline with respect to their cardiovascular risk profile (ie, “healthy” [prehypertension, no hypertension, prediabetes, diabetes, or hypercholesterolemia] or “unhealthy” [having ≥ 1 of these conditions])
| All(N=78 421) | “Healthy”(n=64 217) | “Unhealthy”(n=14 204) | P | |
|---|---|---|---|---|
| Age, y | 27±2 | 27±3 | 28±2 | <.001 |
| Sex, female | 36 | 37 | 28 | <.001 |
| Total cholesterol, mg/dL | 175±32 | 169±26 | 202±40 | <.001 |
| HDL-cholesterol, mg/dLa | 57±14 | 57±14 | 57±15 | .663 |
| LDL-cholesterol, mg/dLb | 121±32 | 120±32 | 124±33 | <.001 |
| Hypercholesterolemia, % | 10 | 0 | 57 | <.001 |
| SBP/DBP, mmHg | 112±13/67±9 | 110±11/66±8 | 118±16/70±10 | <.001 |
| Prehypertension, % | 11 | 11 | 14 | <.001 |
| Hypertension, % | 4 | 0 | 21 | <.001 |
| Fasting glycemia, mg/dL | 87±9 | 85±7 | 93±19 | <.001 |
| Prediabetes, % | 1 | 0 | 4 | <.001 |
| Diabetes, % | <1 | 0 | 3 | <.001 |
| BMI, kg/m2 | 22.2±1.8 | 24.1±3.8 | 26.0±4.6 | <.001 |
| Normal weight, % | 60 | 65 | 46 | <.001 |
| Overweight, % | 31 | 28 | 37 | <.001 |
| Obesity, % | 9 | 7 | 17 | <.001 |
| Smoking, % | 36 | 36 | 36 | .110 |
| Alcohol drinking, % | 10 | 10 | 10 | .475 |
| “Poor” sleep, % | 23 | 23 | 23 | .907 |
| Physical inactivity, % | 51 | 50 | 54 | <.001 |
BMI, body mass index; DBP, diastolic blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SBP, systolic blood pressure.
Unless otherwise specified, the data are expressed as mean±standard deviation.
Cross-sectional association between lifestyle and unhealthy cardiovascular profile among young, economically active individuals. Data are shown as odds ratios with 95% confidence intervals, with individuals not meeting the lifestyle factor as a reference. Analyses for each lifestyle factor were adjusted by age, sex, socioeconomic status, calendar year, and the remaining lifestyle factors (eg, the analysis of physical activity was adjusted for smoking, sleep, alcohol intake, and body mass index).
Cross-sectional association between lifestyle factors and cardiovascular risk factors among young, economically active individuals. Data are shown as odds ratios with 95% confidence intervals, with individuals not meeting the lifestyle factor as a reference. Analyses for each lifestyle factor were adjusted by age, sex, calendar year and socioeconomic status, as well as for the remaining lifestyle factors (eg, the analysis of physical activity was adjusted for smoking, sleep, alcohol intake, and body mass index) and cardiovascular risk factors (eg, the analysis of prehypertension was adjusted for the presence of hypertension, hypercholesterolemia, prediabetes, and diabetes).
A total of 44 776 participants (27±2 years, 34% female) who had a healthy cardiovascular risk profile at baseline were followed up for a median of 2 [2 to 5] years (table 2). As shown in table 3 of the supplementary data, participants with follow-up data showed some differences compared with those for which only baseline data were available (ie, slightly younger age, greater proportion of men, slightly higher levels of total cholesterol, blood pressure and BMI, and a higher proportion of participants who smoked, albeit with a lower proportion of physically inactive individuals and of individuals with poor sleep). Despite these differences between participants with and without follow-up data, respectively, the absence of significant φc coefficients between missing variables, as well as the visual inspection (which failed to identify any discernible pattern of increased frequency in missing data) overall suggested that the loss of data during the follow-up period may have followed a completely random pattern.
Descriptive characteristics of study participants (economically active young adults, aged 18-30 years) at follow-up with respect to their cardiovascular risk profile (ie, staying “healthy” [no development of prehypertension, hypertension, prediabetes, diabetes, or hypercholesterolemia at follow-up] or “unhealthy” [developing ≥ 1 of these conditions])
| All(N=44 776) | Staying “healthy”(n=43 823) | Becoming “unhealthy”(n=953) | P | |
|---|---|---|---|---|
| Age, y | 27.1±2.5 | 27.1±2.3 | 27.5±2.6 | <.001 |
| Sex, female | 34 | 33 | 26 | <.001 |
| Total cholesterol, mg/dL | 176±32 | 174±31 | 201±35 | <.001 |
| HDL-cholesterol, mg/dLa | 56±14 | 56±15 | 56±15 | .650 |
| LDL-cholesterol, mg/dLb | 120±32 | 120±32 | 129±32 | <.001 |
| Hypercholesterolemia, % | 10.6 | - | 70 | - |
| SBP/DBP, mmHg | 112±12/67±9 | 112±12/67±9 | 116±13/68±10 | <.001 |
| Prehypertension, % | 11 | - | 15 | <.001 |
| Hypertension, % | 0.3 | - | 17 | - |
| Fasting glycemia, mg/dL | 87±11 | 86±17 | 88±16 | <.001 |
| Prediabetes, % | 1 | - | 2 | <.001 |
| Diabetes, % | <0.1 | - | 0.1 | - |
| BMI, kg/m2 | 24.5±4.0 | 24.2±3.3 | 25.5±4.8 | <.001 |
| Normal weight, % | 61 | 63 | 48 | <.001 |
| Overweight, % | 30 | 28 | 36 | <.001 |
| Obesity, % | 9 | 9 | 16 | <.001 |
| Smoking, % | 37 | 37 | 36 | .250 |
| Alcohol drinking, % | 10 | 10 | 10 | .580 |
| “Poor” sleep, % | 23 | 23 | 21 | .175 |
| Physical inactivity, % | 51 | 51 | 53 | <.001 |
BMI, body mass index; DBP, diastolic blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SBP, systolic blood pressure.
Unless otherwise specified, the data are expressed as mean±standard deviation.
The majority (98%) of participants included in prospective analyses maintained their risk profile throughout the follow-up period, with 2% transitioning to an unhealthy lifestyle; specifically, 0.04%, 0%, 0.32%, 0.36% and 1.49% developed prediabetes, diabetes, prehypertension, hypertension, and hypercholesterolemia, respectively. Additionally, there was a higher proportion of women and individuals who remained “healthy”.
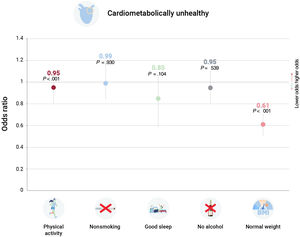
Adjusted analyses showed that having all “healthy” lifestyle factors at baseline was associated with a considerably lower risk of transitioning to an unhealthy risk profile (OR, −38%; 95%CI, -49% to -23%). Analyses focusing on specific lifestyle factors confirmed that having a normal weight (OR, −39%; 95%CI,-49% to −30%) and performing regular physical activity (OR, −5%; 95%CI, −19% to −1%) at baseline were associated with a lower odds of transitioning to an unhealthy profile, with no associations observed for the remaining lifestyle factors (figure 3 and table 4 of the supplementary data). Subanalyses focusing on specific cardiovascular risk factors confirmed that having a normal weight was associated with a lower risk of developing prehypertension (OR, −50%; 95%CI, −66% to −35%), hypertension (OR, −50%; 95%CI, −66% to −43%), and hypercholesterolemia (OR, −32%; 95%CI, −37% to −26%) (figure 4 and table 5 of the supplementary data). Similarly, being physically active was also associated with a lower risk, albeit to a lesser extent, of developing prehypertension (OR, −20%; 95%CI, −35% to −1%), hypertension (OR, −14%; 95%CI, −26% to −1%), prediabetes (OR, −15%; 95%CI, −55% to −2%) and hypercholesterolemia (OR, −1%; 95%CI, −9% to −1%), while nonsmoking was also associated with a reduced risk of developing hypercholesterolemia (OR, −9%; 95% CI, −20% to −2%) (figure 4 and table 5 of the supplementary data). No significant associations were found for the remaining risk factors.
Prospective association between lifestyle and unhealthy cardiovascular risk profile among young, economically active individuals. Data are shown as odds ratios with 95% confidence intervals, with individuals not meeting the lifestyle factor as a reference. Analyses for each lifestyle factor were adjusted by age, sex, socioeconomic status, length of follow-up (expressed in its logarithmic form), and the remaining lifestyle factors (eg, the analysis of physical activity was adjusted for smoking, sleep, alcohol intake, and body mass index).
Prospective association between lifestyle and cardiovascular risk factors among young, economically active individuals. Data are shown as odds ratios with 95% confidence intervals, with individuals not meeting the lifestyle factor as a reference. Analyses for each lifestyle factor were adjusted by age, sex, length of follow-up (expressed in logarithmic form), and socioeconomic status, as well as for the remaining lifestyle factors (eg, the analysis of physical activity was adjusted for smoking, sleep, alcohol intake, and body mass index) and cardiometabolic conditions (eg, the analysis of prehypertension was adjusted for the presence of hypertension, hypercholesterolemia, prediabetes, and diabetes).
The present study reveals a worryingly high prevalence of cardiovascular risk factors among Spanish young adults, with 18% presenting with either prediabetes, diabetes, prehypertension, hypertension, or hypercholesterolemia at baseline. The overall unhealthy lifestyle profile of this nationwide cohort of young adults is another cause of concern, particularly with regards to physical activity habits and weight, as half of the participants failed to meet the minimum World Health Organization recommendations for physical activity and 40% had overweight/obesity despite their young age (below 30 years), with only a very small proportion (3.5%) having an optimal lifestyle. Indeed, in addition to other nonmodifiable factors such as an older age or male sex, being physically active and, particularly, having a normal weight was individually associated with a lower prevalence (−18% and −50%, respectively) and incidence (−5% and −39%) of an unhealthy cardiovascular risk profile in the short-term (figure 5).
Central illustration. There is a relatively high prevalence of cardiovascular risk factors in young, economically active Spanish adults, with 18% having either prediabetes/diabetes, prehypertension/hypertension, or hypercholesterolemia despite their young age. This unhealthy cardiovascular risk profile is associated with a worryingly high prevalence of adverse lifestyle factors, notably overweight/obesity and physical inactivity. 95%CI, 95% confidence interval.
Although young adults typically have a lower cardiovascular risk than their older peers,1 in western countries there is growing concern about the rising risk in the former.1 In a recent study with 12 924 young adults from the USA aged 20 to 44 years, the occurrence of hypertension and diabetes rose from 9.3% to 11.5% and from 3.0% to 4.1%, respectively, between 2009 and 2010 and 2017 and 2020.18 Another recent study found that only 1 in 4 young adults in the USA have an ideal cardiovascular health status-a marker defined from a combination of risk factors (blood pressure, glucose, and cholesterol) along with lifestyle factors (BMI, smoking, physical activity, diet, sleep).19 Likewise, in a longitudinal study of 4836 young adults followed up for 3 decades, cardiovascular health in late adolescence or early adulthood was inversely associated with the rates of premature cardiovascular disease and mortality during this period.20 Promoting measures aiming to improve cardiovascular health in young adults should therefore be a priority.19 Thus, despite the role of genetics in the development of cardiovascular risk factors, particularly in young individuals, adopting a healthy lifestyle can potentially reduce this risk even among individuals with a high genetic risk for cardiovascular disease.21
A major finding of the present study was the high prevalence of suboptimal lifestyle factors among young adults, with a considerable proportion of them (40%) presenting with overweight or obesity (31% and 9%, respectively). Alarmingly high rates of overweight and obesity have been previously reported in Spanish youths, including in younger cohorts. For instance, the Estudio Nutricional de la Población Española study, which analyzed 6800 participants, found a high prevalence of overweight and obesity (ie, 30% for both conditions) among individuals aged 9 to 18 years, with these 2 conditions being positively associated with cardiovascular risk factors (hypercholesterolemia, hypertension, diabetes mellitus).22 Similarly, another study in 2.5 million Spanish children and adolescents reported that obesity rates peaked at 7 to 9 years, with a prevalence of 17%-24%).23
These figures are in line with those from other European countries6 (eg, obesity rates have increased from 2.1%-5.5% to 9.2%-13.8% since 1997 to 2020 among French individuals aged 18-34 years)24 and an even a higher prevalence has been reported in the USA. For instance, a recent study showed that the prevalence of obesity in young US adults aged 20 to 44 years increased from 32.7% in 2009 to 40.9% in 2020.18 The growing prevalence of overweight/obesity can have important-yet preventable-clinical implications, as indicated in the present study. Particularly, preventing overweight/obesity seemed to be the main protective factor against cardiovascular risk in youths, being associated with a reduced odds (by as much as 47%) of transitioning to a healthy cardiovascular risk profile. Although a causal association cannot be inferred from the present study, strong evidence supports a causal association between obesity and cardiovascular risk factors (eg, type II diabetes, dyslipidemia, hypertension), cardiovascular disease (eg, coronary heart disease, heart failure, atrial fibrillation), and cardiovascular-specific mortality.25,26
Along with the high obesity rates, it is also noteworthy that half of the participants in the present study were physically inactive (not meeting minimum World Health Organization guidelines for aerobic physical activity). This is overall in accordance with the figures previously reported for Spanish youths. Notably, according to the Eurobarometer, 19.7% of Spanish youths (19-29 years) do not meet current physical activity guidelines.27 Similarly, a WHO report stated that 31.8% of Spanish adults aged 25 to 34 years do not meet these guidelines.28 These figures are also in line with those reported for other European countries, where nearly one-third of individuals aged 15 to 40 years reported not participating in any physical activity.29 Physical inactivity is an established cardiovascular risk factor in all populations and particularly in young adults,30 as corroborated in the present study, where not only avoidance of overweight/obesity but also being physically active was associated with a reduced risk of becoming “unhealthy” in the short-term, regardless of other lifestyle factors. In support of an inverse association between physical inactivity and cardiometabolic health, the Coronary Artery Risk Development in Young Adults (CARDIA) study, which involved 5115 participants, found that engaging in physical activity during young adulthood was associated with a reduced odds of developing cardiovascular risk factors (diabetes, hypertension, high triglyceride levels) during a 30-year follow-up, as well as with a lower incidence of premature cardiovascular events, particularly heart failure and stroke.30,31
Our results do not support an association between cardiometabolic health in young adults and some lifestyle factors such as smoking, alcohol consumption, and sleeping habits. Issues related to a western lifestyle, including mobile phone use or shift work, contribute to sleep disturbance in a large segment of the population, including younger individuals. Indeed, in line with the present study, in which 23% of participants reported poor sleep, around 30% to 40% of young adults are estimated to experience sleep disturbance.32 In the present study poor sleep was not associated with a higher prevalence of cardiovascular risk factors in young adults, but overall evidence suggests that sleep disturbance can increase the odds of having some risk factors such as hypertension and diabetes,19,33 even among adolescents.34 Similarly, strong evidence shows that smokers, especially those who start at a young age,35 are at higher cardiovascular risk, even when smoking only 1 cigarette a day.36 Last, alcohol consumption, which is widely associated with increased risk, is also a significant concern in young adults.37 This is in line with a recent study in 20 000 individuals with a median follow-up of 5 years, showing that even a single alcoholic drink per day can increase blood pressure.38 However, another study that followed 4711 individuals (aged 18-30 years) for 20 years revealed no association between baseline alcohol consumption and incident hypertension.39 Further research is therefore warranted to assess the complexity and interconnectedness of lifestyle factors and their impact on cardiovascular health.
Some limitations of the present study should be acknowledged, such as the use of self-reported lifestyle factors and the lack of information on dietary habits (which can also impact cardiovascular risk) or on participants’ specific occupations. Concerning the latter, we cannot infer if our results can be generalized to all socioeconomic strata of the same age in Spain. On the other hand, the fact that only 3.5% of the cohort presented with an optimal lifestyle profile might reflect the strictness of the chosen thresholds, such as analyzing not only participants’ sleep duration but also its perceived quality or establishing an optimal threshold for alcohol consumption at less than 1 drink per day. An additional potential limitation is that we focused solely on baseline and last available follow-up data for each participant, but we cannot discern whether variations occurred in the meantime (albeit only 6.1% of the participants underwent more than 2 observations). Furthermore, although missing data in this study may have followed a completely random pattern overall, it should be noted that there were some differences between participants with and without follow-up data (ie, the former were apparently more unhealthy), which might have partly confounded our findings. In this effect, it would, however, be speculative to infer whether the results of the prospective analyses would have changed (and in which direction) in the absence of the aforementioned differences. Additionally, the timeframe of the data collection can be considered a limitation, since almost 10 years have elapsed since data were obtained. While the short follow-up can also be considered a study limitation, it provided interesting insights; for example, we observed that 2% of individuals transitioned to an unhealthy risk profile in 2 to 4 years. The lack of data on cardiovascular events (eg, stroke, mortality) can also be considered a limitation, although the present study focused on cardiovascular risk factors and not on cardiovascular events per se. Finally, we did not perform separate analyses by sex, but all results were adjusted for this variable to avoid this potential confounding effect. Conversely, the extensive sample size analyzed-one of the largest studies on this issue thus far-and the diverse range of lifestyle factors evaluated can be viewed as strengths.
CONCLUSIONSThe present nationwide population-based study shows a relatively large prevalence of cardiovascular risk factors among economically active young adults in Spain, with 18% having prediabetes/diabetes, prehypertension/hypertension, or hypercholesterolemia despite their young age. Moreover, a further 2% of young participants developed at least 1 of these risk factors in the short-term. This overall suboptimal cardiometabolic profile is associated with a worryingly high prevalence of unfavorable lifestyle factors, notably overweight/obesity (40%) and physical inactivity (50%). Our findings underscore the importance of early interventions and targeted public health efforts aimed at promoting healthy lifestyle habits among young adults to reduce the burden of cardiovascular conditions in this population.
- •
The prevalence of cardiovascular risk factors is rising among young adults, highlighting a growing public health challenge.
- •
Significant shifts in lifestyle-related factors have been observed in recent decades, particularly among the younger population, marked by increased rates of obesity and physical inactivity.
- •
This study sheds light on a troubling health trend among economically active young adults in Spain. Only 3.5% maintain an optimal lifestyle, while 18% already have an unhealthy cardiovascular risk profile, exhibiting at least 1 risk factor such as prediabetes/diabetes, hypercholesterolemia, or prehypertension/hypertension.
- •
Crucially, maintaining a normal weight and engaging in regular physical activity were identified as key protective factors, significantly reducing the odds of transitioning to an unhealthy risk profile in the short-term.
P.L. Valenzuela is funded by a postdoctoral contract granted by Instituto de Salud Carlos III (Sara Borrell, CD21/00138). Research by A. Lucia is funded by the Wereld Kanker Onderzoek Fonds (WKOF), as part of the World Cancer Research Fund International grant program (grant # IIG_FULL_2021_007). The funding body played no role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or in the decision to submit the manuscript for publication.
ETHICAL CONSIDERATIONSThe local ethics committee approved the protocol (Universidad Europea Miguel de Cervantes [CEI20-004]). All procedures were performed in accordance with the Declaration of Helsinki and its amendments. Participants provided verbal consent. Since the research (based solely on retrospective analyses of data obtained from routine medical assessments) presented no risk of harm to participants and involved no procedures for which written consent is normally required outside the research context, verbal (and not written) consent was considered to be sufficient. This implied that the participants verbally agreed that the data obtained from routine medical assessments could be confidentially used for epidemiological research purposes.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENo artificial intelligence was used in the preparation of this study.
AUTHORS’ CONTRIBUTIONSResearch idea and study design were led by A. Castillo-García, P.L. Valenzuela, A. Santos-Lozano, and A. Lucia. The statistical analysis was conducted by A. Santos-Lozano. All authors participated in the interpretation of the findings. A. Castillo-García and P.L. Valenzuela drafted the original version of the manuscript. A. Castillo-García oversaw the visualization. P.L. Valenzuela and A. Lucia supervised the work. A. Santos-Lozano and A. Lucia share senior coauthorship. All authors contributed important intellectual content during manuscript drafting or revision and agree to be personally accountable for their own contributions and for responding to any questions pertaining to the accuracy or integrity of any portion of the work.
CONFLICT OF INTERESTSThe authors declare no conflict of interests.
The authors acknowledge the collaboration of Quironprevención, which provided the anonymized data used in this study.