Keywords
INTRODUCTION
Heart failure (HF) is a syndrome of high prevalence, especially in the elderly. This is because of the advanced age among the population in developed countries, the high prevalence of heart diseases (especially ischaemic) in this particular population and the fact that HF, regardless of its aetiology, constitutes the diseases' final progressive form. From an epidemiological perspective, its prognosis can be established quite reliably. Therefore, it is estimated that 50% of the patients die within 4 years following the diagnosis, while the figure for those who have limited daily basic activities, where death occurs within 30 days after an episode of acute decompensated heart failure, reaches 16%.1-4
In this regard, a progressive disease with known prognosis is the ideal setting for patients to receive comprehensive information on the progression of their disease and to participate in important decisions regarding interventions carried out and health care received at the end of their life, in a quiet and introspective manner. The final and most elaborate expression of this process would be the drafting, according to the patient's choice, of an advance healthcare directive or living will (LW). This document is the legal instrument with which patients may record their wish regarding any decisions made at the end of their life on the assumption that, once that moment has come, they themselves could not express it. In Spain, the legal regulation of this process began in Catalonia in 20015 and, currently, it has already been established in all autonomous communities and at state level.6 However, it seems that, in general, this process is not rooted in our society and among cardiac patients in particular. Therefore, in a recent review published in this journal, there was no Spanish study conducted among the elderly with terminal heart disease that addressed the patients' autonomy and living will.7 Meanwhile, for Emergency Medicine, where patients with acute decompensated heart failure (ADHF) are often examined, and ethically important decisions are often made quickly, we do not know, at least subjectively, if adequate information is available in most cases.8-13 Therefore, this study investigates the degree of awareness of the progressive nature of heart failure, the possibility of drafting a LW and the willingness to do so, in patients with HF. It also explores the factors associated with a good knowledge of the disease and a willingness to draft a LW.
METHOD
This is a cross-sectional multicentre study, with prospective inclusion of patients and without intervention. The study was conducted in the emergency departments of three Spanish tertiary hospitals: the Barcelona Clinical Hospital (BCH), which covers a population of approximately 500,000 inhabitants and attends to about 120 000 annual emergency cases; the Alicante General Hospital (AGH), with a population of 270 000 inhabitants and 106 000 annual emergency cases; and the San Carlos Clinical Hospital in Madrid (SCCHM), with a population of 500 000 inhabitants and 150 000 annual emergency cases.
For two 3-month periods (from January 1 to March 31, 2009 and from January 15 to April 14, 2010), we included consecutively all the patients treated between 8 am and 3 pm from Monday to Friday (the authors' working hours), whose primary diagnosis was acute heart failure. The diagnosis of HF was accepted if it was already established in previous hospital admissions by a clinic that met the Framingham criteria.14 We also included patients who, while not having gone to the emergency department during the above-mentioned periods, were in the observation area of the emergency department during those periods. The exclusion criteria were as follows: first episode of HF, cognitive impairment to respond to the questionnaire or refusal to participate in the study. The interviews were conducted privately and individually, once the patient was in a stable condition, and before discharge or admission. The study was approved by the Ethics and Clinical Research Committee of the BCH.
The following clinical and demographic variables were recorded for the patients included in the study: age, gender, level of education completed, marital status, type of household, number of people living at home and existence of prior admissions to hospital or intensive care units (ICU). We held a preliminary meeting between the researchers of the three centres to combine the criteria for inclusion, the dynamics of the interview and the type of information to be provided, so that the questionnaire could be carried out as homogeneously as possible. The first four questions concerned the degree of objective information that the patient had received about the possible progression of their disease. The following four questions were related to the patients' subjective perceptions and specific demands for information and participation, while the last four questions concerned the LW. Eleven of these twelve questions were structured into a dichotomous response (yes/ no), and they were as follows:
1. The doctors have explained to me that I suffer from a chronic disease.
2. The doctors have explained to me that my illness is progressive.
3. The doctors have explained to me that my illness may require admission to an ICU.
4. The doctors have explained to me that my illness may require mechanical ventilation.
5. I consider myself well informed regarding the progression of my illness.
6. I would like to have received more information than I did.
7. I consider that I have been involved in the medical decision-making process concerning my disease.
8. I would have liked to be more involved in the decision-making process concerning my disease than I was.
9. I am aware of and I know what LW entails.
10. The doctors have explained to me what LW is and what it entails.
11. I agree to make a LW in the future.
Lastly, the twelfth question, the response of which was not dichotomous but open, was as follows: who shall be designated as your representative in your LW? Before answering the last two questions, the interviewer explained in detail to the patient, following a script previously agreed by the centres, what the LW entails, its purpose and its development mechanism.
We defined 2 dependent variables. The first related to the proper understanding of the disease. Therefore, we established that patients had a good knowledge concerning the chronic characteristics and the progression possibilities of their disease if they answered affirmatively at least 3 of the first 4 questions. The second dependent variable was the patients' willingness to draft a LW after having received appropriate explanations on it (question 11). The clinical and epidemiological data, the rest of the interview responses and the centre where the patient was recruited were considered as independent variables.
The variables were expressed as mean (standard deviation) if they were quantitative and in percentages if they were qualitative. The comparison between groups was performed using the Student t-test for the quantitative variables.
For the qualitative variables we used the c2 test or, alternatively, Fisher's exact test when the numbers calculated were <5. In those tables with a distribution exceeding 2x2, we merged categories to dichotomise all the variables. Concerning age, the cut was made at age 75 because this age defines geriatric patients. A multivariate analysis was performed using a binary logistic regression model by following the "enter" method. The model included all the variables that obtained a P value of <.05 in the univariate analysis. The goodness-of-fit was estimated using the Hosmer-Lemeshow test by calculating the chi-square of a table of type 2xg frequencies that were observed and expected, where g is the number of groups included in the multivariate analysis. We calculated the odds ratios for the independent variables, and we considered statistically significant those variables where the P value was <.05 and where the confidence interval of the odds ratio excluded the value 1.
RESULTS
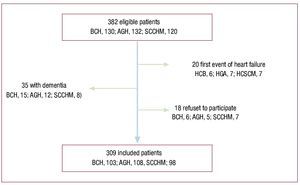
Of the total 382 patients who were identified as eligible, in the end 309 were included in the study (Figure 1), of whom 103 (33.3%) were from the BCH, 108 (35%) from the AGH and 98 (31.7%) from the SCCHM.
Figure 1. Eligible patients and those finally included in the study by centre.
Table 1 shows the characteristics of these patients. As can be seen, there were some differences between the centres: the AGH included a higher percentage of patients with primary education, while the SCCHM included more patients who lived alone, at an erderly nursing home and had previously been admitted to an ICU. Furthermore, we identified a significant variability between the centres concerning the response to the questionnaire, since there were statistically significant differences in 7 of the 12 questions (Table 2). In general, 79% considered themselves subjectively well informed and 56.3% felt they had participated in the decision-making process. This finding contrasted with the fact that 39.8% and 54.7%, respectively, of patients demanded more information and participation in the decision-making process than they had had. Only 13.3% knew what a LW entailed and a mere 4.9% had received this information from their doctor.
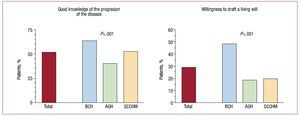
Overall, 51.5% of the patients with HF were objectively well informed, and 28.8% were willing to draft a LW in the future. As shown in figure 2, there were significant differences between the centres, with a lower percentage of well-informed patients at the AGH and a higher percentage of patients willing to draft a LW at the BCH.
Figure 2. Overall results of the dependent variables studied and results by centre.
The independent predictors that the patient was well informed included a previous hospitalisation in an ICU, the subjective consideration of oneself as well informed, sufficient participation in the decision-making process and agreeing to draft a LW (Table 3). On the other hand, the following variables constituted independent predictors of the patients' willingness to draft a LW (Table 4): being a patient at the BCH; being less than 75 years of age; wanting more information; being knowledgeable about LW; and being objectively well informed about the progression possibilities of their disease. As mentioned above, being objectively well informed about the disease and having a willingness to draft a LW were largely associated with both models.
DISCUSSION
For the first time ever, this study explores the degree of knowledge concerning a variety of progressive aspects of the disease and the patients' awareness and position with respect to LW in Spanish patients suffering from HF. The sample of patients with HF included in this study, with an average age of 77 years and with a female predominance, can be considered as representative of the prototype of patients with HF who are treated in Spanish emergency departments.15
Overall, our study suggests that these aspects of knowledge of the disease's chronic status and of the LW are developed in a suboptimal manner in this population. Therefore, the information given to patients with HF should be improved as an essential part of the doctor-patient relationship. However, several findings that emerge from this study deserve to be discussed in detail.
First, we wish to draw attention to the patients' low level of progressive knowledge concerning their disease (only half can be considered as objectively well informed), in contrast to the high percentage who say they are well informed (almost 80%). From our data, it is difficult to explore the cause of this discrepancy. We could guess that patient complacency, together with the persistence of the Spanish traditional paternalistic medicine, may be one of the main causes. This complacency is manifested in the patients' adoption of a passive role towards the decisions that affect them with regard to treatment, and in a desire not to have more information than that which is provided by doctors at their own discretion. The low percentage of patients who called for further information, which was only 39.8%, would be in favour of the previous statement. This aspect is similar to what has already been mentioned in other pathologies, such as patients with chronic obstructive lung disease16 or those infected with HIV,17 where the demand for more medical information did not exceed 20% in both cases. Formiga et al.18 analysed objectively the lack of knowledge of the disease by patients with terminal HF (3%) and their families (25%), which has been transferred to the clinical history.
Second, even worse is the knowledge on LW: only 13.3% knew what it entailed and less than 5% had talked about it with their doctor. As demonstrated by a study carried out in the field of primary healthcare, the low awareness of LW is a generalised reality that goes beyond the specific environment of patients with HF.19 This shows that, despite legislative efforts made in recent years in favour of the patients' right to decide about important situations that concern them, its significance for the population is limited.20-26 In fact, the number of documents recorded in 2008 in Spain was less than 50 000 (0.1% of the general population), of which 21 500 corresponded to Catalonia (0.3% of the Catalan population), 12 360 to Andalusia (0.15% of the Andalusian population), 5700 to Valencia (0.1% of the Valencian population) and 1729 to Madrid (0.03% of the Madrid population).27 In this study, we cannot analyse whether the administration's efforts to provide information, as well as of those involved in the process, have been sufficient or adequate. Regarding the patients, the most active and knowledgeable groups were the Jehovah's Witnesses, members of the "Right to die with dignity" association and similar groups, while professional associations, medical associations and others institutions worked at a medical staff level and issued original documents.28-31 In either case, if associations of patients and medical professionals agree on the need emerging from this attitude, we believe that we should all make an effort to overcome the current lack of information, in the sense that patients can actively demand it and professionals can spontaneously offer it.
Third, and in relation to the previous point, we believe that it is well established that a well-informed patient is a patient willing to draft a LW, since both variables have been associated in the two predictive models as independent factors that positively influence each other. Similar to giving informed consent, patients should have freedom, competence and adequate information about their disease, progression, and alternative treatments in order to decide on their preference regarding the decision-making at the end of their life, on the assumption that when that moment comes, they will not be able to express it.32
Fourth, there are other factors that are associated with good knowledge of the disease and/or willingness to draft a LW. Regarding the former, we highlight its association with admission to ICUs. Contact with advanced stages of the disease and with mechanisms that thereby take place would increase the patients' knowledge of the progressive nature of their disease to a greater degree than their follow-up during routine medical consultations. This is a somewhat paradoxical fact, since it is in such consultations where the ideal conditions converge to deal with these ethical aspects and to develop into a decision, which, sooner or later, patients with advanced HF will face.7,18
Meanwhile, we found that patients who believed to have participated sufficiently in the decision-making process and who believed they were well informed were more likely to be so. In general, there is often a close relationship between information and decision-making, although surprisingly this seems to be delayed or non-existent in these patients due to poorly explored reasons: fear, taboo, superstition, etc.33 Future studies analysing these reasons should allow for a more precise psychological approach to this subgroup of patients, which would perhaps aid them in making a decision. At present, this does not appear to be the case.
Lastly, we believe it is interesting to note that the willingness to draft a LW was largely associated with the hospital of origin. In particular, the patients included in the BCH were more likely to draft a LW than the rest. Perhaps this last finding could be attributed to the fact that Catalonia was a pioneer community in the establishment of legal mechanisms that could lead to the drafting of a LW.5 This could also be accredited to the existence of active campaigns on different fronts,5,30,31 which have resulted in a greater percentage of the population drafting a LW, as discussed above. Furthermore, although meetings were held and information was standardised, we cannot exclude bias of the type of information the informant provided prior to the question, since the person who administered the questionnaire was different in each centre.
Among the limitations of this study, we mention the fact that only 3 Spanish hospitals were included. Therefore, and especially in the light of some discrepancies found among them, the results cannot be directly extrapolated to all patients with HF treated in Spain. On the other hand, the sample was selected from patients who attended emergency departments due to an exacerbation of their HF, which has led to assume bias in the selection of the sample.34 Therefore, it is possible that the degree of knowledge of the disease and the living will, as well as the willingness to draft the latter, is even lower in the general population of patients with HF. Furthermore, those requiring urgent care are patients who are in advanced stages of their disease and where, therefore, these aspects should have been previously addressed. Emergency professionals are especially aware of this pathology,4,15,35,36 since it is highly prevalent in our departments37 and often leads us to make quick decisions without sufficient information.10,12,13 On the other hand, given the modest size of the sample, we cannot exclude categorically that there was a beta error in some estimates, as suggested by some of the confidence intervals of the odds ratios, which have proved to be somewhat wide and may, therefore, be unstable. However, this study constitutes the first of its kind to be conducted in Spain, and by considering it in some way as a pilot programme, we could not perform a priori calculation of the sample size.
CONCLUSIONS
In conclusion, we can say that patients with heart failure receive inadequate information concerning the progression possibilities of their disease and the option of drafting a living will. In addition, their willingness to draft the latter is still limited. Therefore, we believe that doctors who usually treat them in times of clinical stability and who control the progression of their disease (particularly cardiologists, family doctors and interns) should be actively involved in correcting these deficiencies of information, as an integral part of the doctor-patient relationship.
ABBREVIATIONS
AGH: Alicante General Hospital
BCH: Barcelona Clinical Hospital
ICU: Intensive care unit
LW: living will
SCCHM: San Carlos Clinical Hospital in Madrid
SEE ARTICLE ON PAGES 1396-8
Funding: Dr Óscar Miró received a research enhancement grant from the Carlos III Institute in 2009. The research was partly made possible by a grant from the Generalitat of Catalonia to the Consolidated Research Team "Emergencies: processes and pathologies" for the period 2009-2013 (SGR 1385)
Correspondence: Dr. A. Antolin.
Área de Urgències. Hospital Clínic.
Villarroel, 170. 08036 Barcelona. Spain.
E-mail: ANTOLIN@clinic.ub.es
Received June 5, 2010.
Accepted for publication June 28, 2010.