INTRODUCTION
There has been considerable debate about the relative merits of a conservative compared to an invasive approach in non-ST-segment elevation acute coronary syndrome, particularly since stents began to be used in coronary angioplasty. The invasive strategy has generally been preferred. The benefit of such an approach has been demonstrated in randomized trials1-4 and in observational registries,5 particularly in high risk subgroups with ST-segment depression or elevated troponin levels.6,7 The situation is not so clear, however, in diabetic patients. The FRISC II study found a non-significant tendency towards a better prognosis in diabetic patients when an invasive strategy was used,1 whilst in the TACTICS study, although the absolute difference in the primary endpoint (death, infarction or re-admission for acute coronary syndrome within 6 months) was greater in diabetics than in non-diabetics (7.6% vs 2.2%), no significant differences were observed in terms of relative benefit between these 2 groups.3,8 However, neither of these studies took into account diabetic patients' medical treatment, and results for long-term diabetic patients were not analyzed separately.
Several factors could limit the benefits of an invasive strategy in diabetic patients, including: a) the high prevalence of diffuse coronary artery disease, which reduces the options for revascularization9; b) poorer evolution after angioplasty due to higher rates of restenosis and a more rapid evolution of atherosclerosis;10 and c) a higher rate of cardiac and non-cardiac related surgical mortality.11 All of these situations are more frequent in long-term diabetic patients, and particularly in insulin-dependent patients.11,12
The present study included patients with advanced diabetes, managed using an invasive strategy, who were sent for a coronary angiogram because of non-ST-segment elevation acute coronary syndrome. Optimal medical treatment was provided together with invasive treatment. The study objectives were: a) to study the prevalence of diffuse coronary artery disease and its predictors, and b) to study the outcomes after 1 year in patients who underwent revascularization compared to those who did not.
METHODS
Study Population
This was an observational, prospective study performed from October 2002 to June 2004 which included 141 patients from 5 hospitals, 3 of which had a an interventional unit. All patients had been sent for cardiac catheterization due to the presence of non-ST-segment elevation acute coronary syndrome and advanced diabetes mellitus. The invasive strategy consisted of coronary angiography on admission and revascularization when the patient's anatomic characteristics allowed. Diagnosis of acute coronary syndrome was based on the presence of chest pain and at least one of the following conditions on admission: a) elevated troponin levels; b) depressed ST-segment (a minimum of 1 mm in 2 or more contiguous leads) or T wave inversion (a minimum of 1 mm in 2 or more contiguous leads); c) history of angiographically documented ischemic heart disease; and d) signs of ischemia on the stress test when the previous 3 criteria were absent. Advanced diabetes was defined as either: a) insulin-dependence prior to admission, or b) at least 5 years of treatment with oral antidiabetic drugs. Patients with advanced diabetes were included on the basis of results from earlier studies in which insulin-dependent diabetic patients with non-ST-segment elevation acute coronary syndrome had been shown to have a poor prognosis, probably as the result of long-term metabolic disease.13,14 Patients who had been treated with oral antidiabetic drugs for at least 5 years were included to increase patient numbers. Patients were excluded if they had renal insufficiency (creatinine >2.5 mg/dL) or if they had undergone a revascularization procedure in the previous 6 months.
In all 5 hospitals, an invasive strategy was recommended for this type of patient, although the final decision regarding the treatment strategy to follow was left to the interventional cardiologist. Twenty patients were excluded, 14 because of co-morbidity, 5 because of non-revascularizable disease, and 1 because the patient refused to participate. A further 3 patients who were scheduled for inclusion died before catheterization could be performed.
On admission, treatment consisted of aspirin 100 mg/day, clopidogrel (300 mg loading dose and 75 mg daily), and enoxaparin 1 mg/kg every 12 h given subcutaneously. The use of beta-blockers, statins, and angiotensin-converting enzyme inhibitors (ACEI) or angiotensin II receptor blockers (ARB) was also recommended.
Cardiac Catheterization
A contrast left ventriculogram and coronary angiography were performed. Ventriculography was used to calculate the ejection fraction, with values of <55% being considered indicative of depressed ventricular function. Coronary angiography was used to quantify the extent of coronary artery disease by dividing the coronary tree into 29 segments using the BARI scheme.15 Each segment was assigned a score as follows:16 0=normal, 1<30% stenosis, 2=30%-70% stenosis, 3=70%-90% stenosis, and 4=occlusion. The total sum of points represented the extent of coronary artery disease. The number of main vessels (anterior descending, circumflex and right) with ≥70% stenosis was also analyzed, as was the presence of ≥50% stenosis in the left main coronary artery. The diameter of the distal beds of the 2 main vessels, i.e. the anterior descending artery and the other dominant vessel (right coronary or circumflex), was estimated by comparison with the catheter (6 Fr in all cases). The distal bed was defined as narrow if the diameter was less than that of the catheter (2 mm) in the 2 main vessels. Angiographic analysis was performed by a single observer (JS) with no prior knowledge of patient characteristics.
The decision as to whether to perform angioplasty or surgery was left to the interventional cardiologist and the surgeon. When a revascularization procedure was performed, creatine kinase MB isoenzyme (CK-MB) concentration was determined at 12 h and 24 h after the procedure.
Follow-Up
A clinical assessment was performed during outpatient visits at 2, 6, and 12 months. Treatment with aspirin, clopidogrel, statins, beta-blockers, ACEI, or ARB was recommended during the one year follow-up period.
The following events were recorded after catheterization: a) death from any cause; b) acute myocardial infarction (defined as a new episode of chest pain with elevated troponin concentrations or elevated CK-MB in patients with previously elevated troponin concentrations, or elevation of CK-MB to >3 times normal value after angioplasty, or >5 times normal values after heart surgery); and c) readmission for angina, defined as chest pain of likely coronary origin with ECG, abnormalities or abnormal stress test, or coronary arteriography results. The primary endpoint was a combined event of death, acute myocardial infarction, or readmission for angina.
Statistical Analysis
Both angiographic and clinical endpoints were used in the study. The first consisted of the extent of coronary artery disease and the presence of narrow distal beds, and the second was a combined event at 1 year.
The relationship between angiographic and clinical variables was analyzed. Clinical variables included in this analysis were age, sex, insulin dependence, active smoking, arterial hypertension, hypercholesterolemia, family history of ischemic heart disease, previous coronary angioplasty, previous heart surgery, antecedents of stroke, peripheral arterial disease and Killip grade >1 on admission, depressed ST-segment, elevated troponin concentrations, and left ventricular ejection fraction. In the univariate analysis, Student's t test for unpaired data was used to compare the extent of coronary artery disease, introduced as a continuous variable (number of points), between groups defined by dichotomous variables. The relationship between the extent of coronary artery disease and age and ejection fraction was tested using the Pearson correlation coefficient. Stepwise multiple regression analysis was used to identify variables which independently predicted the extent of coronary artery disease; models included all variables which were statistically significant at P<0.1 in the univariate analysis, with a probability-of-F-to-enter ≤0.05 and a probability-of-F-to-remove ≥0.1.
The presence of narrow distal beds in the 2 main coronary vessels was treated as a dichotomous variable. The univariate analyses were performed using the χ2 test for categorical variables and Student's t test for unpaired data for the variables of age and ejection fraction. In the multivariate analysis, binary logistic regression was used with the forward conditional method, with a probability-of-F-to-enter ≤0.05 and a probability-of-F-to-remove ≥0.1.
Due to differences in the demographic, clinical, and angiographic characteristics of patients who underwent revascularization compared to those who did not, a propensity score was used to assess the likelihood that a patient would undergo revascularization.17,18 The aim of this score was to minimize the bias inherent in the decision to revascularize. In order to avoid the confounding effect of including the 10 patients without significant coronary stenosis, who were obviously not revascularized, these were excluded from the analysis of the effect of revascularization. The propensity score was calculated by determining which variables were associated with the likelihood of revascularization (P≤0.2), and adding age and sex. Covariants included were insulin-dependent diabetes, smoking, arterial hypertension, history of hypercholesterolemia, previous heart surgery, extent of coronary artery disease, narrow distal beds, interaction between insulin-dependent diabetes and extent of coronary artery disease, interaction between being male and hypercholesterolemia, interaction between age and narrow distal bed, interaction between insulin-dependent diabetes and stroke, and interaction between peripheral arterial disease and extent of coronary artery disease. Cox's multivariable regression analysis was used to analyze the effect of revascularization after adjusting by the propensity score, which was introduced as a continuous variable.
Statistical analyses were performed in SPSS 9.0 and STATA.
RESULTS
Population Characteristics
The diagnosis of acute coronary syndrome in the 141 patients included in the study was based on elevated troponin concentrations in 97 cases (69%), on depressed ST-segment with normal troponin concentrations in 20 (14%), on T wave inversion with normal troponin concentrations in 8 (6%), on documented angiographic evidence of ischemic heart disease without elevated troponin concentrations or alterations on the ECG in 10 (7%), and on induced ischemia in the stress test in 6 (4%). Table 1 shows the socio-demographic and clinical characteristics of the study population. The sub-group of 20 patients who were excluded from the study were significantly different from those included in terms of age (75±10 vs 68±9 years; P=.005) and the frequency of Killip grade >1 on admission (55% vs 16%; P=.0001).
Cardiac catheterization was performed 4±2 days after admission. Revascularization was performed in 85 patients (60%), 59 using coronary angioplasty and 26 using surgery. Drug-eluting stents were used (rapamycin or paclitaxel) in 73% of the angioplasties, and abciximab in 36%. At discharge, 92% of patients were receiving treatment with aspirin, 72% with clopidogrel, 78% with beta-blockers, 82% with statins, and 81% with ACEI or ARA-II.
Fifteen patients died during follow-up (10.6%), 28 (20%) either died or had acute myocardial infarction, and 39 (27.7%), either died, suffered an infarction, or were readmitted for angina. Eight infarctions and 1 death were associated with the revascularization procedure. No patients were lost to follow-up. The sub-group of patients who were not included had a higher mortality rate (30%; P=.03) and a higher frequency of the triple combined event (55%; P=.02).
Angiographic Findings
The mean extent of coronary artery disease was 16±8 points (median, 17 points). Eighteen patients (12.8%) presented narrow distal beds. One vessel coronary artery disease was observed in 18 patients (13%), 2 vessel disease in 29 (20%), and 3 vessel in 84 (60%). Significant coronary stenosis was not observed in 10 patients (7%). The mean number of affected vessels was 2.3±1, and revascularization was performed in a mean of 1±1 vessels. Revascularization was incomplete in 38 patients (27%). The left main coronary artery was affected in 9 cases (6%).
Table 2 shows the relationship between demographic and clinical variables and the extent of coronary artery disease (points) according to the results of the univariate analysis. The extent of coronary artery disease correlated inversely and significantly with ejection fraction (r=0.37; P=.0001) but did not correlate with age (r=0.14; P=.1). Stepwise multiple regression analysis showed an association between the extent of coronary artery disease and antecedents of heart surgery (β=0.23; P=.03), depressed ST-segment (β=.19; P=.01), Killip grade >1 (β=.19; P=.02) and ejection fraction (β=.30; P=.0001). The population was then further divided into 4 groups according to whether they presented 0 (n=36), 1 (n=54), 2 (n=37), or 3 (n=14) of these variables (no patient presented all 4 variables). The extent of coronary artery disease (12±7, 15±7, 21±6, and 23±7 points; P=.0001) increased in parallel with an increase in the number of predictive variables (Figures 1 and 2), and the differences were statistically significant between patients with ≥2 variables compared to patients with <2 variables. On the other hand, the frequency of revascularization showed a tendency to decrease (77%, 67%, 57%, and 50%; P=.2) as the number of these predictive variables increased. This was particularly true of coronary angioplasty (68%, 49%, 27%, and 28%; P=.004).
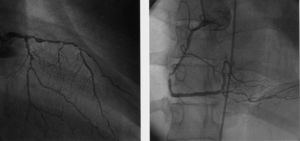
Figure 1. Predictive variables of the extent of coronary artery disease: prior history of heart surgery, depressed ST-segment, Killip class >1 on admission, and ejection fraction <55%. The greater the number of predictive variables, the more widespread the coronary artery disease (12±7, 15±7, 21±6, and 23±7 points; P=.0001), with differences between patients with 2 or more variables and those with less than 2 variables being statistically significant.
Figure 2. Example of angiographic findings in a patient with advanced diabetes and non-ST-segment elevation acute coronary syndrome. This patient showed a depressed ST-segment on the electrocardiogram and depressed ventricular function (FE=48%). Widespread coronary artery (26 points) can be observed.
Table 3 shows the relationship between socio-demographic and clinical variables and the presence of narrow distal beds using univariate analysis. Patients with narrow distal beds were older (72±4 vs 67±9 years; P=.06) and had a poorer ejection fraction (46±13% vs 56±14%; P=.004). Multivariate analysis showed an association between the presence of narrow distal beds and prior heart surgery (odds ratio [OR] =5.6; 95% CI, 1.5-20.9; P=.01), depressed ST-segment (OR=6.0; 95% CI, 1.7-21.5; P=.006), and ejection fraction (OR=0.95; 95% CI, 0.91-0.98; P=.009).
Clinical Evolution
During the one year follow-up, 10 (22%) non-revascularized patients died compared to 5 (6%) revascularized patients (P=.01); 14 (30%) non-revascularized patients either died or suffered an acute myocardial infarction compared to 14 (17%) revascularized patients (P=.08); and 21 (46%) non-revascularized patients either died, suffered an infarction or were re-admitted for angina compared to 18 (21%) revascularized patients (P=.005).
Table 4 shows the differences between revascularized and non-revascularized patients. The propensity score had an area under the ROC curve of 0.80 (0.72-0.87; P=.0001), which shows that the model discriminated adequately between revascularized and non-revascularized patients. Univariate analysis showed that patients who died, suffered infarction, or were re-admitted for angina had a lower propensity score (0.59±0.24 vs 0.69±0.23; P=.03). In the Cox multivariate analysis, revascularization was the only variable which correlated with the combined event (hazard ratio [HR] =0.43; 95% CI, 0.20-0.90; P=.02), while there was no significant association between the combined event and the propensity score (HR=0.90; 95% CI, 0.21-3.80; P=.9).
DISCUSSION
Angiographic Findings in Diabetic Patients With Non-ST-Segment Elevation Acute Coronary Syndrome
Several studies have highlighted the poorer angiographic profile of ischemic heart disease in diabetic patients when compared to non-diabetic patients with a higher prevalence of multi-vessel disease, narrow vessels, calcification, intracoronary thrombus and more poorly developed collaterals.19-22 Diffuse coronary artery disease with narrow vessels is particularly frequent in insulin-dependent diabetes, possibly because of the longer evolution and greater severity of the metabolic disease.
Our study confirms the severity of coronary artery disease in patients with advanced diabetes and non-ST-segment elevation acute coronary syndrome. Variables associated with the extent of coronary artery disease were also analyzed, thereby providing information which could be useful to the intervening cardiologist by providing prior knowledge of patients who would likely have a poorer anatomical profile of the coronary arteries and therefore a lower probability of receiving angioplasty. Variables associated with the extent of coronary artery disease were: prior history of heart surgery, depressed ST-segment, and alteration of the ventricular function reflected in a Killip grade >1 at the time of admission or a reduction in the ejection fraction in the left ventriculogram. Patients with 2 or more of these factors had more extensive coronary artery disease and therefore were less likely to undergo angioplasty.
The Invasive Strategy and Revascularization
Diabetes is an independent predictor of mortality in non-ST-segment elevation acute coronary syndrome,23-25 particularly in insulin-dependent diabetes,13,14 and prognosis is generally poorer in diabetic patients after coronary angioplasty because of a greater frequency of restenosis,26 again particularly in insulin-dependent patients.12 The introduction of drug-eluting stents has advanced the field of coronary angioplasty by reducing restenosis rates, even in diabetic patients.27 Nevertheless, some studies suggest that restenosis rates in insulin-dependent patients are still considerable.28 Prognosis after heart surgery is also poorer in diabetic patients, particularly insulin-dependent patients,11 because of greater co-morbidity and more extensive coronary artery disease.
All of these factors may limit the benefits of the invasive strategy in diabetic patients. Although randomized studies indicate that an invasive strategy should be used in diabetic patients with non-ST-segment elevation acute coronary syndrome,1-3,8 it should be remembered that: a) the results were obtained in a posteriori subgroup analysis; b) the differences found were not statistically significant; c) a differential analysis in patients with advanced diabetes was not carried out; and d) medical treatment was not controlled for in the analysis and drug-eluting stents were not used.
In the present study, advanced diabetes was defined as diabetes which had required over 5 years of pharmacological treatment, or which required insulin to achieve metabolic control. Two aspects of patient treatment stand out: a) medical treatment was optimized, as indicated by the high frequency of double antiplatelet therapy and of treatment with beta-blockers, statins, and ACEIs or ARBs; and b) drug-eluting stents were used in 73% of the angioplasties. The low use of abciximab can be explained by the fact that all patients were treated with double antiplatelet therapy from admission onwards. There were significantly fewer events in revascularized patients during follow-up, in spite of the fact that non-revascularized patients received optimal pharmacological treatment. Although the poorer prognosis in non-revascularized patients is surely related in part with the selection of patients with a better anatomical profile for revascularization, the benefits of the procedure persisted even after adjusting by the propensity score.
CONCLUSIONS
Patients with advanced diabetes and non-ST-segment elevation acute coronary syndrome have extensive coronary artery disease. Previous heart surgery, a depressed ST-segment and poorer ventricular function are associated with more extensive coronary artery disease. The follow-up results indicate that revascularization improves prognosis in these patients.
Limitations
In order to study the benefits of revascularization, a randomized trial is necessary in which patients with similar characteristics are treated using either the invasive or the conservative strategy. In the present study, the decision to revascularize, which was left to the individual investigators, introduced confounding variables which obscure the assessment of the benefits of revascularization and make it impossible to analyze this objective. Nevertheless, a propensity score was used to minimize the bias inherent in the decision to revascularize and after adjusting the predictive analysis by a propensity score with an adequate discriminatory power (C statistic=0.80), revascularization during the hospital stay reduced the likelihood of events after 1 year. On the other hand, patients with associated morbidity or heart disease which was known to preclude revascularization were not included in the study. Finally, due to the fact that the catheterization was performed on average 4 days after admission, 3 patients who died before catheterization could be carried out were also excluded from the study.
ACKNOWLEDGEMENTS
The authors are grateful to the Instituto Valenciano del Corazón (INSVACOR) for coordinating this study.
Correspondence: Dr. J. Sanchís.
Servei de Cardiologia. Hospital Clínic Universitari.
Blasco Ibáñez, 17. 46010 Valencia. España.
E-mail: sanchis_juafor@gva.es
Received June 23, 2005.
Accepted for publication January 27, 2006.