The age of heart transplant recipients and donors is progressively increasing. It is likely that not all donor-recipient age combinations have the same impact on mortality. The objective of this work was to compare survival in transplant recipients according to donor-recipient age combinations.
MethodsWe performed a retrospective analysis of transplants performed between 1 January 1993 and 31 December 2017 in the Spanish Heart Transplant Registry. Pediatric transplants, retransplants and combined transplants were excluded (6505 transplants included). Four groups were considered: a) donor <50 years for recipient <65 years; b) donor <50 years for recipient ≥ 65 years; c) donor ≥ 50 years for recipient ≥ 65 years, and d) donor ≥ 50 years for recipient <65 years.
ResultsThe most frequent group was young donor for young recipient (73%). There were differences in the median survival between the groups (P <.001): a) younger-younger: 12.1 years, 95%CI, 11.5-12.6; b) younger-older: 9.1 years, 95%CI, 8.0-10.5; c) older-older: 7.5 years, 95%CI, 2.8-11.0; d) older-younger: 10.5 years, 95%CI, 9.6-12.1. On multivariate analysis, independent predictors of mortality were the age of the donor and the recipient (0.008 and 0.001, respectively). The worst combinations were older-older vs younger-younger (HR, 1.57; 95%CI, 1.22-2.01; P <.001) and younger-older vs younger-younger (HR, 1.33; 95%CI, 1.12-1.58; P=.001).
ConclusionsAge (of the donor and recipient) is a relevant prognostic factor in heart transplant. The donor-recipient age combination has prognostic implications that should be identified when accepting an organ for transplant.
Keywords
In recent decades, the age of heart transplant (HTX) recipients has been progressively increasing.1–3 This is because new drugs and devices for the treatment of heart failure (HF) have delayed the development of advanced HF at older ages.4,5 As a consequence, patients reach older ages in better physical and psychological condition. Moreover, greater knowledge of heart preservation and the vast amount of accumulated experience in transplantation has increased the use of hearts from older donors.6–8
Taking into account the age trend of donors and recipients described in the Spanish Heart Transplant Registry3 and in other annual registries,2,9,10 it would appear that there has been an increase in the implantation of younger hearts in older patients and vice versa. However, there is a knowledge gap regarding the frequency of these types of implantations, a lack of comparisons between the different groups (younger donor, older donor, younger recipient, older recipient) and between survival rates in these groups, and little information on the actual risk entailed by some of these combinations.
Our working hypothesis was that donor-recipient age combinations have a different impact on survival and that the worst combinations should be identified and possibly not used.
The objective of this study was to analyze the impact of donor-recipient age combinations on survival in HTX recipients.
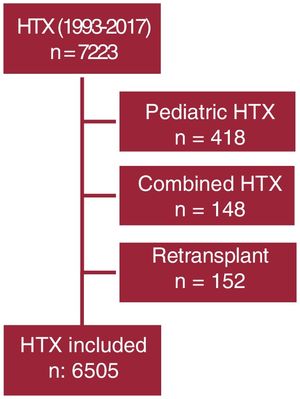
METHODSWe conducted a retrospective analysis of all transplants performed in Spain between January 1, 1993 and December 31, 2017. Pediatric transplants (under 16 years old), retransplants, and combined transplants (kidney, liver, or lung) were excluded. The final number of transplants was 6505 (figure 1).
The data analyzed were obtained from the Spanish Heart Transplant Registry, which includes all transplants performed in Spain (HTX is currently performed in 16 Spanish centers). Transplant data are prospectively entered into an online database. The registry includes more than 100 variables related to recipient, donor, intervention, immunosuppression, and follow-up (table 1 of the supplementary data. The Spanish Heart Transplant Registry is an official registry of the Spanish Ministry of Health and the Spanish Government. The appendix of the supplementary data shows the list of centers and collaborators of the Spanish Heart Transplant Registry. This subanalysis was approved by the Clinical Research Ethics Committee of the Hospital Universitari i Politècnic La Fe (Valencia, Spain).
An older recipient was defined as one more than or equal to 65 years. An older donor was defined as one more than or equal to 50 years. Four combinations were analyzed: younger donor-younger recipient (donor <50 years - recipient <65 years), younger donor-older recipient (donor <50 years - recipient ≥ 65 years), older donor-younger recipient (donor ≥ 50 years - recipient <65 years), and older donor-older recipient (donor ≥ 50 years - recipient ≥ 65 years). We also analyzed the predictive variables of mortality.
Variables are expressed as mean±standard deviation, or the median [interquartile range] in the absence of normality, and percentages. Differences between groups were analyzed using the chi-square test for qualitative variables and the Kruskal-Wallis test for quantitative variables. Survival curves were calculated using the Kaplan-Meier method and comparisons between them using the log-rank test. Cox proportional hazards model was used to adjust the multivariate model of donor-recipient age groups. In addition to the donor-recipient ages, we initially included variables of known clinical relevance and those that had a P value greater than 1 in the univariate analysis. Recipient age was included in the model via the combined donor-recipient age variable. Because recipient age is a categorical variable with more than 2 categories, its inclusion in the model entailed its transformation into dummy variables. A dummy variable is a dichotomous (binary) variable that can only take the value 0 or 1, indicating the absence or presence of a certain characteristic, respectively. The final model was obtained by using a backward procedure to simplify the nonsignificant variables included in the adjustment.
RESULTSDistribution of the number of transplants by age group and clinical profileWe selected 7223 HTXs that were performed between 1993 and 2017 (figure 1). Of these, 418 pediatric transplants, 148 combined transplants, and 152 retransplants were excluded: thus, the final analysis included 6505 HTXs
The proportion of recipients aged more than or equal to 65 years was 10.81%. The proportion of transplant patients with donors more than 50 years was 19.67%. The distribution of the combinations was as follows: donor less than50 years for recipient less than65 years, 73%; donor less than50 years for recipient more than or equal to 65 years, 7.33%; donor more than or equal to 50 years for recipient less than65 years, 16.20%; and donor more than or equal to 50 years for recipient more than or equal to 65 years, 3.48%.
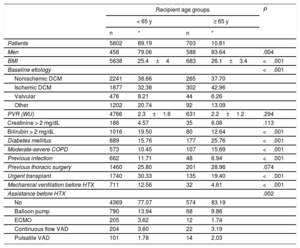
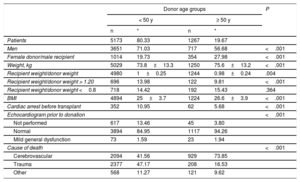
Demographic characteristics of donors and recipientsTable 1 and table 2 shows the clinical profile of the recipients and donors included in the study. The statistical comparison of the recipients showed that those aged more than or equal to 65 years had more comorbidities (diabetes mellitus and chronic obstructive pulmonary disease), although the percentage of urgent transplants was lower. Nonischemic dilated cardiomyopathy and valvular heart disease were more frequent among younger recipients, whereas ischemic dilated cardiomyopathy was more frequent among older recipients. Urgent transplantation was performed more frequently in recipients younger than 65 years than in older recipients. Thus, there was greater use of short-term ventricular assist devices as a bridge to transplant in younger recipients. This aspect may partly explain the higher prevalence of pretransplant infection in recipients less than 65 years (patients fitted with circulatory/ventricular assist devices with prolonged stays in critical care units). Stroke as a cause of death was more frequent among donors aged more than or equal to 50 years and affected more women than men.
Demographic characteristics of the recipients
| Recipient age groups | P | ||||
|---|---|---|---|---|---|
| < 65 y | ≥ 65 y | ||||
| n | * | n | * | ||
| Patients | 5802 | 89.19 | 703 | 10.81 | |
| Men | 458 | 79.06 | 588 | 83.64 | .004 |
| BMI | 5638 | 25.4±4 | 683 | 26.1±3.4 | <.001 |
| Baseline etiology | <.001 | ||||
| Nonischemic DCM | 2241 | 38.66 | 265 | 37.70 | |
| Ischemic DCM | 1877 | 32.38 | 302 | 42.96 | |
| Valvular | 476 | 8.21 | 44 | 6.26 | |
| Other | 1202 | 20.74 | 92 | 13.09 | |
| PVR (WU) | 4766 | 2.3±1.6 | 631 | 2.2±1.2 | .294 |
| Creatinine > 2 mg/dL | 186 | 4.57 | 35 | 6.08 | .113 |
| Bilirubin > 2 mg/dL | 1016 | 19.50 | 80 | 12.64 | <.001 |
| Diabetes mellitus | 889 | 15.76 | 177 | 25.76 | <.001 |
| Moderate-severe COPD | 573 | 10.45 | 107 | 15.69 | <.001 |
| Previous infection | 662 | 11.71 | 48 | 6.94 | <.001 |
| Previous thoracic surgery | 1460 | 25.80 | 201 | 28.96 | .074 |
| Urgent transplant | 1740 | 30.33 | 135 | 19.40 | <.001 |
| Mechanical ventilation before HTX | 711 | 12.56 | 32 | 4.61 | <.001 |
| Assistance before HTX | .002 | ||||
| No | 4369 | 77.07 | 574 | 83.19 | |
| Balloon pump | 790 | 13.94 | 68 | 9.86 | |
| ECMO | 205 | 3.62 | 12 | 1.74 | |
| Continuous flow VAD | 204 | 3.60 | 22 | 3.19 | |
| Pulsatile VAD | 101 | 1.78 | 14 | 2.03 | |
BMI, body mass index; COPD, chronic obstructive pulmonary disease; DCM, dilated cardiomyopathy; ECMO, extracorporeal membrane oxygenation; HTX, heart transplant; PVR, pulmonary vascular resistance; VAD, ventricular assist device; WU, Wood units
P value obtained using the chi-square test and Kruskal-Wallis test.
Demographic characteristics of donors
| Donor age groups | P | ||||
|---|---|---|---|---|---|
| < 50 y | ≥ 50 y | ||||
| n | * | n | * | ||
| Patients | 5173 | 80.33 | 1267 | 19.67 | |
| Men | 3651 | 71.03 | 717 | 56.68 | <.001 |
| Female donor/male recipient | 1014 | 19.73 | 354 | 27.98 | <.001 |
| Weight, kg | 5029 | 73.8±13.3 | 1250 | 75.6±13.2 | <.001 |
| Recipient weight/donor weight | 4980 | 1±0.25 | 1244 | 0.98±0.24 | .004 |
| Recipient weight/donor weight > 1.20 | 696 | 13.98 | 122 | 9.81 | <.001 |
| Recipient weight/donor weight <0.8 | 718 | 14.42 | 192 | 15.43 | .364 |
| BMI | 4894 | 25±3.7 | 1224 | 26.6±3.9 | <.001 |
| Cardiac arrest before transplant | 352 | 10.95 | 62 | 5.68 | <.001 |
| Echocardiogram prior to donation | <.001 | ||||
| Not performed | 617 | 13.46 | 45 | 3.80 | |
| Normal | 3894 | 84.95 | 1117 | 94.26 | |
| Mild general dysfunction | 73 | 1.59 | 23 | 1.94 | |
| Cause of death | <.001 | ||||
| Cerebrovascular | 2094 | 41.56 | 929 | 73.85 | |
| Trauma | 2377 | 47.17 | 208 | 16.53 | |
| Other | 568 | 11.27 | 121 | 9.62 | |
BMI, body mass index
P value obtained using the chi-square test and Kruskal-Wallis test.
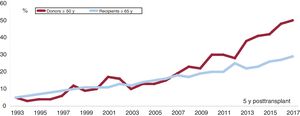
Figure 2 shows the percentage of recipients and donors in relation to total transplants each year. There was a gradual increase in both groups. However, from 2007 onward, the increase was no longer proportional as the progression curves began to separate.
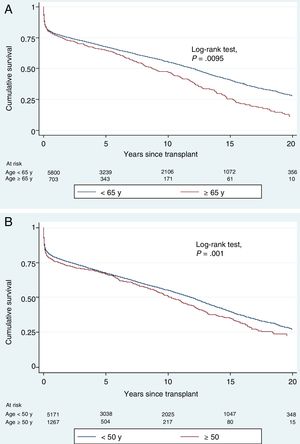
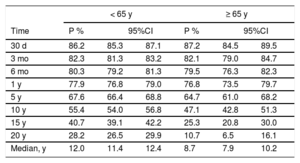
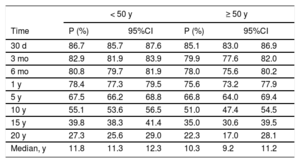
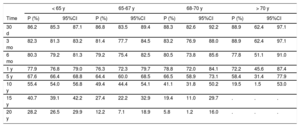
Survival by age groupTable 3 and table 4 show the probability of survival by age group, median survival, and confidence intervals over the entire follow-up period. The median survival of recipients less than 65 years was 12 years, whereas that of recipients more than or equal to 65 years was 8.7 years. However, the median survival of donors less than 50 years was 11.8 years, whereas that of donors more than or equal to 50 years was 10.3 years.
Probability of survival (P) and median survival by recipient age
| < 65 y | ≥ 65 y | |||||
|---|---|---|---|---|---|---|
| Time | P % | 95%CI | P % | 95%CI | ||
| 30 d | 86.2 | 85.3 | 87.1 | 87.2 | 84.5 | 89.5 |
| 3 mo | 82.3 | 81.3 | 83.2 | 82.1 | 79.0 | 84.7 |
| 6 mo | 80.3 | 79.2 | 81.3 | 79.5 | 76.3 | 82.3 |
| 1 y | 77.9 | 76.8 | 79.0 | 76.8 | 73.5 | 79.7 |
| 5 y | 67.6 | 66.4 | 68.8 | 64.7 | 61.0 | 68.2 |
| 10 y | 55.4 | 54.0 | 56.8 | 47.1 | 42.8 | 51.3 |
| 15 y | 40.7 | 39.1 | 42.2 | 25.3 | 20.8 | 30.0 |
| 20 y | 28.2 | 26.5 | 29.9 | 10.7 | 6.5 | 16.1 |
| Median, y | 12.0 | 11.4 | 12.4 | 8.7 | 7.9 | 10.2 |
95%CI, 95% confidence interval by recipient age group.
At 10 years, 15 years, and 20 years after transplant, the percentage of recipients younger than 65 years and older than or equal to 65 years falls to 65% and 49.8% (10 years), 33% and 17.7% (15 years), and 11% and 2.9% (20 years), respectively.
Probability of survival (P) and median survival by donor age
| < 50 y | ≥ 50 y | |||||
|---|---|---|---|---|---|---|
| Time | P (%) | 95%CI | P (%) | 95%CI | ||
| 30 d | 86.7 | 85.7 | 87.6 | 85.1 | 83.0 | 86.9 |
| 3 mo | 82.9 | 81.9 | 83.9 | 79.9 | 77.6 | 82.0 |
| 6 mo | 80.8 | 79.7 | 81.9 | 78.0 | 75.6 | 80.2 |
| 1 y | 78.4 | 77.3 | 79.5 | 75.6 | 73.2 | 77.9 |
| 5 y | 67.5 | 66.2 | 68.8 | 66.8 | 64.0 | 69.4 |
| 10 y | 55.1 | 53.6 | 56.5 | 51.0 | 47.4 | 54.5 |
| 15 y | 39.8 | 38.3 | 41.4 | 35.0 | 30.6 | 39.5 |
| 20 y | 27.3 | 25.6 | 29.0 | 22.3 | 17.0 | 28.1 |
| Median, y | 11.8 | 11.3 | 12.3 | 10.3 | 9.2 | 11.2 |
95%CI, 95% confidence interval by donor age group.
At 10 years, 15 years, and 20 years after transplant, the percentage of recipients less than 65 years and older than or equal to 65 years falls to 65% and 49.8% (10 years), 33% and 17.7% (15 years), and 11% and 2.9% (20 years), respectively.
Figure 3 shows the survival curves of the recipients and donors grouped by age. During the time period shown, the survival curves gradually separated and reached statistical significance.
Analysis of the influence of age on survival (in both figure parts death is the final outcome). A, comparison of recipients younger than 65 years and recipients older than or equal to 65 years. Log-rank test, P = .0095. B, comparison of donors younger than 50 years and donors older than or equal to 50 years. Log-rank test, P < .001.
Table 5 shows the distribution of the main causes of death of recipients by donor-recipient age groups.
Distribution (%) of the main causes of death of recipients by donor-recipient age group
| Donor-recipient age groups | Total (n=3540) | ||||
|---|---|---|---|---|---|
| Younger-younger (n = 2684) | Younger-older (n = 290) | Older-older (n = 114) | Older-younger (n = 452) | ||
| Primary failure | 11.14 | 10.69 | 16.67 | 18.36 | 12.20 |
| Acute rejection | 5.89 | 4.14 | 6.14 | 6.19 | 5.79 |
| Chronic rejection | 7.15 | 4.14 | 1.75 | 4.65 | 6.41 |
| Infection | 16.17 | 19.66 | 20.18 | 19.91 | 17.06 |
| Cancer | 15.05 | 18.62 | 11.40 | 13.27 | 15.00 |
| Cardiac arrest | 7.56 | 4.48 | 6.14 | 4.87 | 6.92 |
| Multiorgan failure | 5.25 | 7.24 | 5.26 | 5.31 | 5.42 |
| Other | 31.78 | 31.03 | 32.46 | 27.43 | 31.19 |
| Total | 100 | 100 | 100 | 100 | 100 |
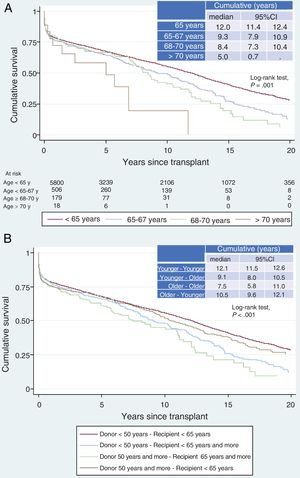
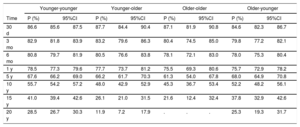
Table 6 shows the probability of short-, mid-, and long-term survival of recipients in 4 age groups (age <65 years, 65-67 years, 68-70 years, and> 70 years). Long-term survival decreased as the age of the recipients increased. Table 7 shows the probability of survival in the 4 study groups. The probability of survival was highest in the younger donor-younger recipient combination and lowest in the older donor-older recipient combination. Of the other 2 combinations, the probability of survival was highest in the older donor-younger recipient. Figure 4 compares actuarial survival between recipient age groups and between the 4 donor-recipient combinations (log-rank test).
Probability of survival (P) with 95% confidence interval by recipient age groups
| < 65 y | 65-67 y | 68-70 y | > 70 y | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time | P (%) | 95%CI | P (%) | 95%CI | P (%) | 95%CI | P (%) | 95%CI | ||||
| 30 d | 86.2 | 85.3 | 87.1 | 86.8 | 83.5 | 89.4 | 88.3 | 82.6 | 92.2 | 88.9 | 62.4 | 97.1 |
| 3 mo | 82.3 | 81.3 | 83.2 | 81.4 | 77.7 | 84.5 | 83.2 | 76.9 | 88.0 | 88.9 | 62.4 | 97.1 |
| 6 mo | 80.3 | 79.2 | 81.3 | 79.2 | 75.4 | 82.5 | 80.5 | 73.8 | 85.6 | 77.8 | 51.1 | 91.0 |
| 1 y | 77.9 | 76.8 | 79.0 | 76.3 | 72.3 | 79.7 | 78.8 | 72.0 | 84.1 | 72.2 | 45.6 | 87.4 |
| 5 y | 67.6 | 66.4 | 68.8 | 64.4 | 60.0 | 68.5 | 66.5 | 58.9 | 73.1 | 58.4 | 31.4 | 77.9 |
| 10 y | 55.4 | 54.0 | 56.8 | 49.4 | 44.4 | 54.1 | 41.1 | 31.8 | 50.2 | 19.5 | 1.5 | 53.0 |
| 15 y | 40.7 | 39.1 | 42.2 | 27.4 | 22.2 | 32.9 | 19.4 | 11.0 | 29.7 | . | . | . |
| 20 y | 28.2 | 26.5 | 29.9 | 12.2 | 7.1 | 18.9 | 5.8 | 1.2 | 16.0 | . | . | . |
95%CI, 95% confidence interval.
Probability of survival (P) with 95% confidence interval by donor-recipient age combinations
| Younger-younger | Younger-older | Older-older | Older-younger | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time | P (%) | 95%CI | P (%) | 95%CI | P (%) | 95%CI | P (%) | 95%CI | ||||
| 30 d | 86.6 | 85.6 | 87.5 | 87.7 | 84.4 | 90.4 | 87.1 | 81.9 | 90.8 | 84.6 | 82.3 | 86.7 |
| 3 mo | 82.9 | 81.8 | 83.9 | 83.2 | 79.6 | 86.3 | 80.4 | 74.5 | 85.0 | 79.8 | 77.2 | 82.1 |
| 6 mo | 80.8 | 79.7 | 81.9 | 80.5 | 76.6 | 83.8 | 78.1 | 72.1 | 83.0 | 78.0 | 75.3 | 80.4 |
| 1 y | 78.5 | 77.3 | 79.6 | 77.7 | 73.7 | 81.2 | 75.5 | 69.3 | 80.6 | 75.7 | 72.9 | 78.2 |
| 5 y | 67.6 | 66.2 | 69.0 | 66.2 | 61.7 | 70.3 | 61.3 | 54.0 | 67.8 | 68.0 | 64.9 | 70.8 |
| 10 y | 55.7 | 54.2 | 57.2 | 48.0 | 42.9 | 52.9 | 45.3 | 36.7 | 53.4 | 52.2 | 48.2 | 56.1 |
| 15 y | 41.0 | 39.4 | 42.6 | 26.1 | 21.0 | 31.5 | 21.6 | 12.4 | 32.4 | 37.8 | 32.9 | 42.6 |
| 20 y | 28.5 | 26.7 | 30.3 | 11.9 | 7.2 | 17.9 | . | . | . | 25.3 | 19.3 | 31.7 |
95%CI, 95% confidence interval.
Analysis of the influence of age and the recipient-donor combination on survival (in both figure parts death is the final outcome). A, comparison by recipient age. Log-rank test, P < .001. B, comparison of recipient-donor age combinations. Log-rank test, P < .001. 95%CI, 95% confidence interval.
Table 2 of the supplementary data shows Cox univariate analysis for the mortality outcome. Table 8 shows the final adjusted multivariate model of mortality outcome. In HTX patients, many variables are associated with mortality. In both the donor and recipients, increased age was linearly related to increased mortality. Furthermore, after adjustment for other significant variables, all donor-recipient age combinations were independent predictors of mortality in relation to the best combination (ie, younger donor-younger recipient).
Multivariate analyses effect of donor and recipient age on mortality
| Variablea | HRb | 95%CI | P | |
|---|---|---|---|---|
| Younger donor-older recipient (young-older vs young-younger) | 1.38 | 1.16 | 1.64 | <.001 |
| Older donor-older recipient | 1.62 | 1.23 | 2.13 | .001 |
| Older donor-younger recipient | 0.98 | 0.81 | 1.18 | .845 |
95%CI, 95% confidence interval; HR, hazard ratio.
Final multivariate model adjusted for diabetes mellitus, kidney failure, previous sternotomy, mechanical ventilation, extracorporeal circulation time, induction, primary graft failure, dialysis, infection in the first year, cancer (skin cancer vs none and nonskin cancer vs none), and year of transplant.
In the first decades of HTX, only people younger than 35 years were accepted as donors.11–13 However, as waiting lists grew and there was an urgent need for more hearts as soon as possible,14 transplant teams began to accept hearts from more donors.3,15,16 In addition, until relatively few years ago, HTX was exclusively restricted to recipients aged up to 50 years. However, in recent decades, the age of recipients has increased and the selection criteria have been expanded.1,17–19 These changes have been due to advances in surgical techniques, major improvements in postoperative treatment, and above all, new treatments and devices for HF that improve the quality and quantity of life, thus allowing these patients to reach older ages in good health.20,21 In addition, in recent decades, there has been progressive improvement in the treatment of diseases that may ultimately lead to ischemic HF (ie, the generalized use of primary angioplasty programs), valvular HF, cardiotoxicity, and so on. These improvements delay the onset and development of HF, thus shifting upward the age at which HTX is indicated. Therefore, since the beginning of HTX, donor and recipient age has also progressively increased. This trend may also be related to greater experience in THX. However, as of 2007, the progression curves separated and the proportion of donors older than 50 years increased annually much more than that of recipients older than 65 years. Thus, the annual proportion of donors older than 50 years old exceeded 50%. It is not clear what could have happened in that year, but it may have been the case that the greater demand due to longer waiting lists, the increase in urgent transplants, and more experience in donor selection led to the view that the older age of these donors was no longer considered to be an excessive risk to survival. Currently, all transplant teams accept donors above this age. The latest HTX register from the International Society for Heart and Lung Transplantation (ISHLT) also shows that from 2009 to 2017 there was a progressive increase in the age of donors.22
There are few scientific studies on the impact of this trend. Although the ISHLT guidelines recommended increasing the age of potential recipients to 70 years in 2006,23 many hospitals still consider age to be a limiting factor for HTX in patients with advanced HF. Data from the Spanish Heart Transplant Registry3 may clarify the relationship between donor-recipient age and survival. For all these reasons, this study analyzed the impact of 4 donor-recipient age combinations on HTX survival. The 4 groups comprised younger donor to younger/older recipient and older donor to a younger/older recipient. The results showed that there was a difference in survival between the 4 groups. The best combination was younger donor-younger recipient and the worst combination was older donor-older recipient. However, the results from other 2 groups are those with the greatest interest from the point of view of clinical practice.
We followed the previous literature to determine the cutoff point to consider a donor as older, because several studies have shown that a donor age of more than 50 years is associated with an increased risk of posttransplant mortality.7,24 Other studies have used cutoff points of 50 years or more and less than 40 years to consider donors as older and younger, respectively. Donors aged 40 to 49 years were excluded from the analyses to obtain a clearer distinction between the 2 groups.25 However, given the significant percentage of donors in this interval, we used a cutoff point of 50 years to include the entire spectrum of donors. Thus, the results of the analysis are more relevant from a clinical perspective and may assist in decision-making in real-world settings.
In Spain, 11% of patients who undergo HTX are older than 65 years. In these recipients, the most frequent cause of heart disease is of ischemic origin and the prevalence of comorbidities is higher; however, the proportion of urgent transplants and mechanical ventilation is lower. This profile is similar to that reported in previous studies, especially in relation to the higher prevalence of comorbidities and ischemic heart disease in this group of recipients. A steady trend (typically nonsignificant) has been observed toward a lower percentage of these patients undergoing urgent HTX.26
In the present study, 20% of the donors were older than 50 years and a higher percentage of women died from nontraumatic cerebrovascular causes. However, the recipient/donor weight ratio was better in the previous study.26 The aforementioned profile is similar to that reported in some registries,15,25 in which stroke was the most frequent cause of death in donors more than or equal to 50 years; however, the percentage of female donors in this group was not high.
The distribution of donor-recipient age groups shows that the number of patients differed in each group. The most frequent group was younger donor for younger recipient (73%) followed by older donor for younger recipient (16.2%). The Spanish Heart Transplant Registry3 database was used to obtain a sufficient number of patients in the less frequent groups (younger donor for older recipient [7.3%] and older donor for older recipient [3.5%]). This registry includes all the HTXs performed in Spain from the first one in May 1984 to the present and is completed by all the Spanish HTX teams.
Significant differences were found between transplants in older and younger recipients, with a difference of almost 3.5 years in median survival (12 years vs 8.7 years, respectively). An association was also found between an increase in the age of the recipients and a decrease in their probability of survival. In fact, in recipients older than 70 years, the probability of post-HTX 10-year survival was only 19.5%. However, there were no differences between recipient groups in early mortality. Thus, the survival curves were identical at the beginning and then began to gradually separate. This finding could be explained by expected survival time based on the age of the recipients independently of the transplant. It could also lead to the age of the recipient not being considered as the only criterion by which HTX could be contraindicated.
Differences were also found in median survival between donors and recipients older and younger than 50 years (11.8 years vs 10.3 years, respectively). In this case, however, the difference was 1.5 years. It therefore appears that donor age is not as relevant as recipient age as a cause of long-term mortality. The survival curve shows that the initial fall, which is related to the perioperative process, was greater when the donors were older. Subsequently, the curves tended to separate slightly, then from 5 years onward the separation clearly widened consistently over time. The scientific literature typically considers donor age to be an independent risk factor for mortality in HTX,27,28 although there are conflicting data. Data from the most recently published ISHLT registry11 and the United Network for Organ Sharing29 database show that advanced donor age increases the risk of mortality for all recipients. However, a Spanish study published in 2015 found no difference in mortality in older donors after adjusting for confounding factors, although it found a mid-term increase in the risk of vascular graft disease in older donors.
The present study found differences between donor-recipient age combinations. The worst mean survival time was found in the older donor-older recipient age combination (7.5 years). The other 3 combinations initially showed similar survival curves; however, from the fifth year onward the gap between curves began to widen. Thus, mean survival time was 12.1 years in the younger-younger combination, 10.5 years in the older-younger combination, and 9.1 years in the younger-older combination. The results show survival would be reduced in each risk combination by approximately 1.5 years in relation to the best combination (younger-younger, 12 years). A study published in 2020 assessed the relationship between donor and recipient age by dividing recipients into those younger than 60 years vs those older than or equal to 60 years and donors younger than 50 years vs those older than or equal to 50 years. Five-year survival was significantly lower among recipients who received an older heart than among those who received a younger heart (67% vs 73% respectively; log-rank test, P <.001).23
Multivariate analysis confirmed the relevance of donor-recipient age to survival. Thus, the risk of mortality was 32% higher in recipients older than 65 years than in recipients younger than 65 years. Furthermore, there were significant differences in survival between the best age combination (younger donor-younger recipient) and all the other combinations, except for one: there were no significant differences in survival between the older donor-younger recipient combination and the younger donor-younger recipient combination. This may make individuals older than or equal to 55 years suitable donors even for younger recipients without it being a predictor of worse survival. Furthermore, significance was maintained after adjustnebt if the variables with those that reached significance in the univariate analysis and that are known to be associated with posttransplant mortality.30,31 However, the option of transplanting older hearts into older patients (worst combination) should not be rejected, because in these patients survival times are much longer than those in patients older than 65 years with advanced HF.32,33
LimitationsThis study has the limitations associated with the use of databases; although main variables are entered prospectively, the analysis and inclusion of secondary variables can be retrospective. However, in the present study, the main variables were fixed, were not subject to defining criteria, were 100% complete, and could not give rise to confusion. Therefore, the results of this study have a high level of reliability and show real trends. Moreover, the present study was a multicenter study of all HTXs performed in the inclusion period in which all Spanish HTX teams participated. These characteristics also ensure that the results have a high level of reliability and are representative of the real situation in Spain, where there is a highly developed HTX organization system. This study also shows that although few older hearts are implanted, they do not reduce survival time by very much, particularly when they are implanted in younger recipients. Further research could investigate whether the donor pool could be increased and determine the research strategies to be conducted by the HTX groups and the Spanish National Transplant Organization.
CONCLUSIONSThe results of the present study suggest that the age of the donor and recipient is a relevant prognostic factor in HTX. The donor-recipient age combination has prognostic implications that must be known and weighed up when accepting an organ for transplant.
CONFLICTS OF INTERESTNone declared.
- –
In recent decades, the age of heart transplant donors and recipients has been increasing.
- –
Some studies have shown donor age to be a predictor of poor prognosis.
- –
Some studies have shown that survival times in older recipients can be similar to those in younger recipients.
- –
This study provides information on comparisons between different donor-recipient age combinations (younger donor-younger recipient, younger donor-older recipient, older donor-older recipient, and older donor-younger recipient) and confirms that there are significant differences in survival times between them.
- –
The best combination is younger donor-younger recipient and the worst is older donor-older recipient. All the age combinations had worse survival than the best combination, except for one: there were no significant differences in survival between the older donor-younger recipient combination and the younger donor-younger recipient combination.
- –
This finding may change the current paradigm, given that it has been shown that an older heart does not worsen survival in a younger recipient. Thus, it should be possible to increase the number of donors.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2020.02.016