The aim was to determine whether secondary prevention involving the comprehensive and intensive treatment of cardiovascular risk factors reduces cardiovascular events and cardiovascular mortality at 3-year follow up.
MethodsThe study design comprised a randomized, controlled, open trial in a routine clinical practice setting. In total, 247 patients who presented with acute coronary syndrome or stroke were selected. They were randomized to comprehensive and intensive treatment of cardiovascular risk factors (n=121) or to follow-up based on usual care (n=126). The main study outcomes were the number of cardiovascular events and cardiovascular mortality at 3-year follow-up. The percentage of patients in whom each risk factor was successfully controlled was a secondary outcome.
ResultsOverall, 88.8% of patients assigned to the intensive treatment group had a low-density lipoprotein cholesterol level <100mg dl compared with 56 4 of the usual-care group relative risk rr 95 confidence interval ci 1 28-1 93 and 75 7 diabetics had a hemoglobin 1c <7 compared with 28 6 of the usual-care group rr="2.65;" 95 ci 1 13-6 19 there were four deaths due to cardiovascular causes and 26 nonfatal events in intensive treatment versus 17 54 cumulative survival rate at 3 years was 97 4 intervention 85 5 control P=.003).
ConclusionsSecondary prevention involving comprehensive and intensive treatment of cardiovascular risk factors reduced both morbidity and mortality at 3-year follow up.
Keywords
According to the World Health Organization, of the approximately 58 million deaths in the world that occurred in 2005, 30% were due to cardiovascular causes. A high proportion of these deaths (46%) was in patients < 70 years of age. Between 2006 and 2015 an increase of 17% is expected in deaths due to non-transmissible diseases (half of which are due to cardiovascular causes).1
Control of cardiovascular risk factors (CVRF) is the most effective measure known to decrease cardiovascular morbimortality, and many international guidelines establish targets to be achieved by patients with high cardiovascular risk.2,3,4,5,6,7,8 Nonetheless, in Spain, only between 6.9% and 16.9% of high-risk patients have all their factors under control.9,10
Two previous studies have shown a reduction in cardiovascular morbidity by means of a multifactorial intervention on CVRF. The Steno-2 study in diabetic patients with microalbuminuria showed a 50% reduction of cardiovascular events.11 More recently, our group showed a reduction of 64.3% in the incidence of cardiovascular events after a year of follow-up in patients in secondary prevention (MIRVAS project).12 Neither of these showed a short term reduction in mortality. However, a more prolonged follow-up of the patients included in Steno-2 has shown a reduction in cardiovascular mortality.13 This study shows the results of prolonging the MIRVAS patient follow-up for 3 years. Our aim is to demonstrate a reduction not only of cardiovascular morbidity but also mortality, by means of a complete and intensive control of CVRF in a group of patients in secondary prevention compared with a control group treated in the usual manner.
MethodsThe MIRVAS study is a randomized single-center clinical trial that assesses the effect of complete and intensive treatment of CVRF on cardiovascular morbimortality in patients in secondary prevention. Detailed information on the MIRVAS Study12 has been previously published. Briefly, we included in the study patients from 18 to 80 years of age admitted for acute coronary syndrome (with or without ST segment elevation) or for ischemic stroke between September 2002 and February 2004. From the care information available in our center, we assumed an incidence of cardiovascular events at 3 years of follow-up of 40%, we set an alpha risk of 5% and a power of 90% to find differences of 20% between both groups, and we estimated a sample size of 119 patients.
Exclusion criteria were the following: refusal or impossibility of participating in the follow-up (patients who moved or had reduced mobility), life expectancy of < 12 months and severe cognitive deterioration. Before hospital discharge, randomization by blocks (according to the disease: coronary or stroke) assigned each patient to either the intervention group or the control group using a computer generated list, with a different person in charge of this task than of the previous tasks.
InterventionThe patients assigned to the intervention group on the day of their hospital discharge received health education by a trained nurse, informing them of the meaning of their disease and the importance of carrying out correct treatment. Subsequently, visits were programmed at 2, 5, 12, 24, and 36 months after the acute episode, with the possibility of more visits if considered appropriate. Furthermore, the patients could consult with other specialists related to their cardiovascular disease. Each visit consisted of a nursing intervention (health education, lifestyle modifications, evaluation of adherence to treatment) and a medical assessment (clinical evaluation and modification of treatment, if appropriate).
Patients in the control group had the usual follow-up in cardiology or neurology and/or primary care consulting offices. Additionally, they were given annual appointments in our consulting offices to monitor lifestyle factors, drug treatment received, degree of CVRF control and the existence/non-existence of symptoms, visits to the Emergency Service and/or hospital admittance for any reason. There were no interventions.
The targets set for the different risk factors and the drug recommendations issued by different international guidelines are specified in Table 1, Table 2.1,2,3,4,5,6,7
Table 1. Control Targets for the Different Risk Factors.
| Risk factor | Target level |
| Blood pressure | BP < 140/90mmHg |
| BP <130/80mmHg (diabetes or kidney failure) | |
| Diabetes mellitus | Glycated hemoglobin <7% |
| LDLc | LDLc < 100mg/dl |
| Tobacco use | No consumption of any type of tobacco during the last 6 months |
| Alcohol consumption | Consumption of < 30g of alcohol/day |
| Weight | BMI < 25 kg/m2 |
| Physical exercise | Mild or moderate aerobic physical exercise during a minimum of 30min daily or 45min 3 days a week |
| Diet | Low in animal fats |
| Low in sodium in hypertensive patients | |
| Low in calories in cases of overweight |
BMI, body mass index; LDLc, low density lipoprotein cholesterol.
Table 2. Drug Interventions Recommended by International Guidelines for Secondary Prevention of Cardiovascular Risk.
| Angiotensin-renin-aldosterone system blockers for all patients, whatever their blood pressure 4 |
| Statins at appropriate doses for all patients, whatever their LDLc levels 7 |
| Platelet antiaggregants or oral anticoagulants if indicated, for all patients |
| Betablockers in cases with heart failure or ischemic cardiopathy |
LDLc: low density lipoprotein cholesterol.
The following final primary variables were defined: cardiovascular mortality and cardiovascular morbimortality, which included the following events: death due to cardiovascular causes, acute coronary syndrome with or without ST segment elevation, stroke (ischemic or hemorrhagic), transient ischemic attack, new diagnosis of peripheral arterial disease, peripheral territory revascularization, amputation as a consequence of peripheral ischemia, and admittance for heart failure; secondary variables consisted of the percentage of patients with each of the controlled risk factors at 3 years of follow-up. All episodes were considered as such if there was a clinical report supporting them. The evaluation was carried out by a nonblinded member of the research team.
Statistical AnalysisQuantitative variables were compared using the Student t test and qualitative variables using the χ2 and the Fisher exact tests. Survival curves were estimated for the time until the first event by means of the Kaplan-Meier method. A proportional risks regression model was adjusted to measure the effect of the intensive treatment, adjusted by age, sex, blood pressure values, diabetes, tobacco smoking, excessive alcohol consumption, history of cardiovascular disease at the beginning of the study, episode that led to the inclusion, and baseline low density and high density lipoprotein cholesterol (LDLc and HDLc) values. A step-by-step regression was used to construct the model, including the analysis of those variables that were statistically significant in the univariate analysis. Data analysis was carried out based on intention to treat. Calculation of the number of patients needed to treat (NNT) to prevent a cardiovascular event or a cardiovascular death was based on a rates ratio.
In all cases we considered that values < 0.05 were statistically significant. Statistical analysis was carried out with the SPSS program, version 13.0.
Ethical ConsiderationsThe study was approved by the Research and Ethics Committee of the Hospital Universitario de la Princesa. All patients gave their informed consent. The trial was registered with the reference ISRCTN93700442 at http://www.controlled-trials.com/
ResultsWe invited 260 patients to participate, of which 247 accepted and were included in the study; 121 (49%) were assigned to the intervention group and 126 (51%) to the control group. Eighteen patients (14.9%) of the intervention group dropped out of the follow-up, but not of the study. Their information was obtained by telephone or by means of consulting hospital databases at the time of study closure and all were included in the analysis based on intention to treat. The baseline characteristics of the 18 patients of the intervention group not followed up did not present any statistically significant differences in comparison with the followed-up group, although the first group had a greater frequency of stroke (11.1% vs. 5.3%) and diabetes (61.1% vs. 25.5%). The reasons for abandoning follow-up were the following: 2 patients due to change of place of residence, 1 due to health insurance other than the Spanish social security and 15 due to a personal decision. Of the control group, 71 (59.5%) patients did not come for their appointment; however, their information was obtained by means of telephone contact or hospital databases. The only missing data were morbimortality on 3 patients of the intervention group and 5 patients of the control group (Figure 1).
Figure 1. Patient flow diagram.
The episode that led to inclusion was ischemic cardiopathy in 162 patients (65.6%) and stroke in 85 (34.4%). Mean age at the time of inclusion was 64.9 years in the intervention group and 65.6 years in the control group. Of those patients included, 74.5% were men and 24.5% were women. The baseline characteristics of the patients in both groups were similar (Table 3). Mean follow-up (standard deviation) of the patients was 3.12 (0.82) years.
Table 3. Baseline Characteristics According to Assigned Group a
| Intervention group (n=121) | Control group (n=126) | P | |
| Sex | |||
| Male (%) | 79.3 | 69.8 | 0.108 |
| Female (%) | 20.7 | 30.2 | |
| Vascular history | |||
| Ischemic Cardiopathy (%) | 16.5 | 12.9 | 0.172 |
| Stroke (%) | 5.0 | 4.9 | |
| PAD (%) | 4.1 | 0 | |
| None (%) | 73.6 | 80.6 | |
| Various (%) | 0.8 | 1.6 | |
| Personal inclusion event | |||
| Ischemic Cardiopathy (%) | 64.5 | 66.7 | 0.789 |
| Stroke | 35.5 | 33.3 | |
| Acute treatment b | |||
| Primary angioplasty (%) | 66.67 | 71.25 | 0.27 |
| Fibrinolysis (%) | 33.33 | 28.75 | |
| Tobacco smoking (%) | 41.3 | 35.7 | 0.433 |
| Alcohol consumption (%) | 23.1 | 18.3 | 0.351 |
| HT (%) | 52.9 | 61.1 | 0.201 |
| High LDLc (%) | 62.8 | 54.8 | 0.245 |
| Diabetes mellitus (%) | 31.4 | 26.2 | 0.400 |
| Age (years) | 64.89 (11.53) | 65.60 (14.3) | 0.667 |
| LDLc (mg/dl) | 110.59 (32.31) | 106.98 (41.78) | 0.460 |
| HDLc (mg/dl) | 49.73 (25.87) | 45.89 (11.40) | 0.144 |
| Triglycerides (mg/dl) | 129.18 (58.61) | 130.06 (54.34) | 0.905 |
| Creatinine clearance (ml/min) | 77.93 (20.82) | 81.58 (50.37) | 0.484 |
HDLc, high density lipoprotein cholesterol; HT, hypertension; LDLc, low density lipoprotein cholesterol; PAD, peripheral arterial disease.
a Qualitative variables are expressed as %, and quantitative variables are expressed as mean (standard deviation).
b Treatment during the acute phase in patients with ischemic cardiopathy. Intervention group n=77; control group n=83.
Table 4 shows the degree of CVRF control in both groups at 3 years. A greater percentage of patients in the intervention group abstained from tobacco and alcohol, carried out physical exercise, and followed a low calorie diet; however, only the differences seen with reference to these last two were significant.
Table 4. Control of Cardiovascular Risk Factors After 3 Years of Follow-Up.
| Variable | Intervention group n a (%) b | Control group n a (%) b | P | RR (95% CI) |
| Tobacco smoking | 106 (90.6) | 51 (86.3) | 0.422 | 1.05 (0.93-1.19) |
| Alcohol | 106 (93.4) | 51 (84.3) | 0.085 | 1.13 (1-1.28) |
| Diet | 106 (95.2) | 50 (70) | < 0.001 | 1.36 (1.13-1.64) |
| Physical exercise | 105 (84.8) | 50 (60) | < 0.001 | 1.41 (1.11-1.80) |
| Global BP Target | 106 (82.1) | 56 (71.4) | 0.159 | 1.15 (0.95-1.39) |
| BP target with history of HT | 59 (72.9) | 35 (65.7) | 0.463 | 1.11 (0.83-1.48) |
| BMI < 25 kg/m2 | 99 (19.2) | 48 (18.8) | 0.949 | 1.02 (0.50-2.09) |
| LDLc < 100 mg/dl | 107 (88.8) | 78 (56.4) | < 0.001 | 1.57 (1.28-1.93) |
| HBA1C < 7% | 37 (75.7) | 14 (28.6) | 0.004 | 2.65 (1.13-6.19) |
| Intervention group c | Control group c | Diference c | P of the difference | |
| Systolic BP (mmHg) | 123.22 (15.05) | 128.47 (20,42) | −5.26 (2,81) | 0.63 |
| Diastolic BP (mmHg) | 70.45 (11.29) | 71.75 (11,24) | −1.30 (1,85) | 0.48 |
| BMI (kg/m2) | 28.82 (4,26) | 29.39 (5.31) | −0.57 (0,81) | 0.49 |
| LDLc (mg/dl) | 79.45 (22.07) | 93.63 (29.31) | −14.18 (3,93) | < 0.005 |
| HDLc (mg/dl) | 53.59 (14,61) | 50.38 (14.42) | 3.20 (2,16) | 0.14 |
| HbA1c (%) | 6.55 (0,84) | 8.30 (1,62) | −1.75 (0,45) | 0.001 |
| Triglycerides (mg/dl) | 110.87 (53,71) | 116.49 (59) | −5.62 (8,43) | 0.51 |
BMI, body mass index; BP, blood pressure; HbA1c: glycated hemoglobin; HDLc, high density lipoprotein cholesterol; HT, hypertension; LDLc, low density lipoprotein cholesterol; RR, relative risk.
a Number of patients included in the analysis.
b Percentage of patients with controlled risk factors.
c Data are expressed as mean (standard deviation).
The intervention group achieved better control of blood pressure, LDLc and glycated hemoglobin, although the difference related to blood pressure was not significant.
TreatmentsTable 5 shows the treatments prescribed for each group. An angiotensin-converting enzyme inhibitor or angiotensin receptor antagonist and a statin were prescribed with greater frequency for patients in the intervention group. Prescription of anticoagulants and antiaggregants was similar for both groups.
Table 5. Prescribed Drug Groups According to Assignation.
| Drug | Intervention group (n=111)(%) | Control group (n=55) (%) | P | RR [95% CI] |
| ACEI/ARB | 93.7 | 72.7 | < 0.001 | 5.57 [2.12-14.67] |
| Betablocker | 50.9 | 58.2 | 0.378 | 0.75 [0.40-1.43] |
| Statin | 94.5 | 83.6 | 0.040 | 3.39 [1.14-10.08] |
| AA/OAC | 99.1 | 100.0 | 1 | 1 |
AA, antiaggregant; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CI, confidence interval; OAC, oral anticoagulation; RR, relative risk.
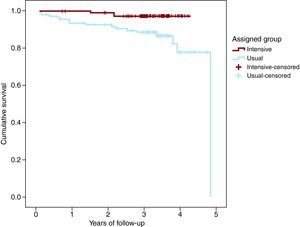
There were 4 cardiovascular deaths in the intervention group and 17 in the control group. Survival rate at 3 years (Kaplan-Meier) was 97.4% (SD 1.5) in the intervention group and 85.5% (SD 3.1) in the control group (p=0.003) (Figure 2).
Figure 2. Survival curve.
Nineteen of 118 (16.1%) patients in the intervention group and 54 of 121 (44.6%) in the control group had suffered at least 1 cardiovascular event, a reduction of absolute risk of 28.5%. The crude risk of suffering a cardiovascular event was 4.2 times greater in the control group (95% confidence interval [CI], 2.29-7.71) (Mantel-Haenszel). The total number of cumulative events was 31 in the intervention group and 74 in the control group (Table 6).
Table 6. Cardiovascular Episodes During the 3 Years of Follow-Up.
| Intervention group, n | Control group, n | |
| Cardiovascular death | 4 | 17 |
| STACS | 2 | 5 |
| NSTACS | 14 | 25 |
| Established stroke | 0 | 6 |
| TIA | 2 | 1 |
| Admittance due to heart failure | 6 | 13 |
| New diagnosis of PAD | 2 | 4 |
| Peripheral revascularization | 0 | 0 |
| Amputation | 0 | 0 |
| Cardiovascular death | 1 | 3 |
NSTACS, non-ST elevation acute coronary syndrome; PAD, peripheral artery disease; STACS, ST elevation acute coronary syndrome; TIA, transient ischemic attack.
The cardiovascular mortality rate (hazard ratio [HR]), estimated by means of an adjusted Cox model, was significantly greater in older patients assigned to the control group than in those with a history of cardiovascular disease, low baseline levels of high density cholesterol (HDLc), and lower levels of estimated creatinine clearance (Table 7). The patients assigned to the control group had a greater risk of cardiovascular death than those in the intervention group (HR=5.42 95% CI, 1.22 to 21.64); history of cardiovascular disease and low levels of HDLc (taken as a continuous variable, without a defined cut-off point) also supposed greater risk (Table 8).
Table 7. Cardiovascular Mortality Rates for Different Risk Factors. Univariate Analysis.
| HR [95% CI] | P | |
| Control group | 5.142 [1.550-18.593] | 0.008 |
| Vascular disease prior to the episode that caused inclusion in the study | 4.847 [1.878-12.512] | 0.010 |
| HDLc | 0.986 [0.975-0.999] | 0.030 |
| Age | 1.093 [1.033-1.157] | 0.002 |
| Baseline creatinine clearance | 0.960 [0.935-0.986] | 0.003 |
| Type of event at inclusion | 1.216 [0.471-3.144] | 0.686 |
| Smoking | 0.827 [0.310-2.206] | 0.705 |
| Alcohol consumption | 0.032 [0.0-3.429] | 0.149 |
| Hypertension | 1.902 [0.678-5.335] | 0.222 |
| LDLc at baseline | 0.811 [0.319-2.059] | 0.659 |
| Diabetes | 0.883 [0.314-2.487] | 0.814 |
CI, confidence interval; HDLc, high density lipoprotein cholesterol; HR, hazard ratio; LDLc, low density lipoprotein cholesterol.
Table 8. Mortality Rates Adjusted for Different Risk Factors. Multivariate Analysis.
| HR [95% CI] | P | |
| Control group | 5.142 [1.222-21.641] | 0.026 |
| Previous vascular disease | 1.952 [1.387-2.747] | < 0.001 |
| Low levels of HDLc | 1.019 [1.003-1.035] | 0.021 |
CI, confidence interval; HDLc, high density lipoprotein cholesterol; HR, hazard ratio.
The NNT during 3 years to prevent a cardiovascular event was 2.90 (95% CI, 1.52 to 23.51), and the NNT to prevent cardiovascular death was 4.73 (95% CI, 2.6 to 11.89).
DiscussionAfter 3 years of follow-up involving complete and intensive control of cardiovascular risk factors, it was possible to reduce the absolute risk of cardiovascular morbidity by 28.5% and total mortality by 11.9%. These results are comparable with those found in other cardiovascular high risk populations such as those of the Steno-2 Study in diabetic patients, which achieved a 29% reduction in a combination of cardiovascular events and a reduction of 20% in total mortality after 13.3 years of follow-up,13 confirming the efficacy of complete and intensive control in patients in a secondary prevention environment, and not only in diabetes. In our study, 44.6% of the control group patients suffered a cardiovascular event during the 3 years of follow-up, compared to 40 of 80 patients (60%) in Steno-2 with a more prolonged follow-up. The fact that in our study we also included patients admitted for heart failure may have increased the number of events observed.
Although previous studies have demonstrated that intensive multifactorial treatment achieves better control of risk factors, our study is the first to demonstrate that this translates into a reduction of cardiovascular mortality with only 3 years of intervention. Therefore, in our environment, a study published by Muñoz et al14 did not find any differences between intensive treatment and usual treatment in spite of the fact that better blood pressure and LDLc control were achieved. Their multicenter study was carried out in a primary care environment, and did not recruit patients after an acute event. The fact that our study was carried out in a specialized care environment, by only one center, with more homogeneous care and provided immediately after an event may have influenced our results.
Strandberg et al15, in the DEBATE Study of patients > 75 years of age with cardiovascular disease, which compared multifactorial treatment with usual treatment, found that there was better control of blood pressure (72.7% vs. 56.8%) and of LDLc (81.3% vs. 35.9%) and better compliance with therapeutic guidelines. However, no reduction of total mortality or number of cardiovascular events was achieved. In contrast to our study, they included elderly patients and the blood pressure and cholesterol levels achieved are not as low.
This reduction in cardiovascular mortality is based on greater treatment compliance with international guidelines and, consequently, better control of cardiovascular risk factors. This is in line with previous studies published by Yan et al,16 in which an optimum treatment was associated with a lower risk of cardiovascular mortality at 1 year (ratio=0.54; 95% CI, 0.36 to 0.81, p=0.001). Furthermore, Salomma et al17 found a lower risk of mortality in patients treated with betablockers (HR=0.47; 95% CI, 0.41 to 0.53) or with lipid lowering drugs (HR=0.54; 95% CI, 0.49 to 9.60). Both studies highlighted underutilization of treatments with currently accepted evidence-based effectiveness. The percentage of patients that were correctly treated is similar to that found in the control group in our study.
This study has certain limitations. One of them is the heterogeneity of patient follow-up, since patients had no limitation on consultations with different specialists. However, we believe that any additional follow-up is not more frequent in one group than in another, i.e., is equal for both groups, and does not affect the results.
The number of patients included in our study is not very large, but has been sufficient to show decreased mortality and morbidity. It was not powerful enough, however, to find significant differences in smoking or excessive alcohol consumption, since the number of included patients with these risk factors was low in both groups.
The number of patients who dropped out of intensive follow-up is relatively high (18). The reason for this dropout rate was mainly duplication of consultations, in many cases due to recommendation of the different specialists involved in the follow-up. In spite of the fact that a single follow-up in internal medicine consulting offices would have improved adherence, for ethical reasons we did not consider the possibility of limiting visits to other specialists.
In the control group, 59% of the patients did not attend the consultation, which meant that there was a lack of intermediate variables (blood pressure, cholesterol, treatment received, etc.). We attempted to complete the missing information by means of hospital database consultation or telephone interviews. Although we did not have intermediate data for all patients, we did have morbimortality data for most of them. Therefore, the primary study objective was not affected. As to the secondary objectives, it was to be expected that the patients in the control group who attended consultation would cooperate more and would possibly be better controlled. The degree of control of risk factors such as hypertension and LDLc in recently published studies10,18 is worse than in our control group, between 25%-60% for hypertension and 13.3%-26.3% for LDLc. This fact, if it had influenced our results, would have made it difficult to achieve significant results in our study.
We believe that the high rate of events in the control group, compared with the intervention group, can be attributed to the difference in the intervention carried out. In the case of the control group, the usual intervention in the Spanish health system was applied in the health care area where the study was performed. Our study collected a quite large number of patients admitted for heart failure, and this may have contributed to a greater rate of events. We find no other reason other than the type of intervention received (control of CVRF, health education, nursing consultation) that can explain the different rate of events between both groups.
ConclusionsOur work underlines the need for complete and intensive control of cardiovascular risk factors in patients in secondary prevention to decrease mortality due to cardiovascular causes. On this subject, a consultation by an internal medicine physician with specialized nursing support has been shown to be useful to improve prognosis in these patients in the short term.
Conflicts of interestNone declared.
Received 25 October 2009
Accepted 9 July 2010
Corresponding author: C/ Pirra 18, Portal Q, Ático D. 28022 Madrid, Spain. miguel.m.palanco@gmail.com