Limited data are available on the clinical outcomes of optimal medical therapy (OMT) compared with revascularization by percutaneous coronary intervention (PCI) in patients with chronic total coronary occlusion (CTO) of the proximal or middle left anterior descending artery (pmLAD). Therefore, the objective of this study was to compare the long-term outcomes of patients with pmLAD CTO who were treated with a PCI strategy with those of patients treated with an OMT strategy.
MethodsBetween March 2003 and February 2012, 2024 patients with CTO were enrolled in a single-center registry. Among this patient group, we excluded CTO patients who underwent coronary artery bypass grafting. After the exclusion, a total of 1547 patients remained. They were stratified according to classification of coronary segments (pmLAD or non-pmLAD CTO) and the initial treatment strategy (OMT or PCI). Propensity score matching was performed. The primary outcome was cardiac death.
ResultsThe median follow-up was 45.9 (interquartile range, 22.9-71.1) months. After propensity score matching, the incidence of cardiac death (HR, 0.54; 95%C, 0.31-0.94, P=.029) was significantly lower in the PCI with pmLAD CTO group than in the OMT group. In contrast, no significant difference was found in the rate of cardiac death between the PCI and OMT groups with non-pmLAD CTO (HR, 0.62; 95%CI, 0.27–1.42, P=.26).
ConclusionsAs an initial treatment strategy, PCI of pmLAD CTO, but not PCI of non-pmLAD, is associated with improved long-term survival.
Keywords
Percutaneous coronary intervention (PCI) technology has made remarkable progress in the treatment of chronic total coronary occlusion (CTO) lesions.1,2 Successful PCI of CTO reduces the need for repeat revascularization and improves survival.3–5 However, only 1 in 10 patients with CTO will undergo PCI because the success rate of CTO PCI is only 70% or less and the complication rates and procedural costs are high.6,7 Furthermore, an initial PCI strategy in CTO may not reduce the risk of cardiac death, subsequent myocardial infarction (MI), or repeat revascularization compared with initial optimal medical therapy (OMT).8 Therefore, it is important to select patients who are likely to derive a survival benefit from revascularization by PCI.
The prognosis of patients with ischemic heart disease is related to the extent of myocardium at risk. Previous studies conducted in either acute MI9,10 or stable ischemic heart disease11 have shown that patients with occlusion of the left anterior descending artery (LAD) have a significantly worse prognosis, whereas patients with lesions in the left circumflex artery or right coronary artery have a better prognosis. This is because a large amount of myocardium is supplied by the diseased LAD, especially the proximal or middle left anterior descending artery (pmLAD). It has been reported that patients with larger amounts of myocardium have worse clinical outcomes than patients with non-pmLAD.9,12 Accordingly, a revascularization strategy by PCI might confer advantages in patients with pmLAD CTO lesions compared with an OMT only strategy. The objective of this study was to examine whether an initial PCI strategy could reduce adverse cardiac events in patients with pmLAD CTO compared with an initial OMT only strategy.
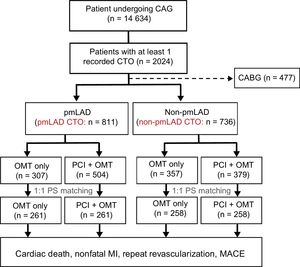
MethodsStudy PopulationBetween March 2003 and February 2012, a total of 2024 consecutive patients were enrolled in a single-center registry. Clinical, laboratory, and outcome data were collected by a trained study coordinator using a standardized case report form and protocol. If necessary, additional information was documented by contacting the principal investigators and/or by reviewing hospital records. The Institutional Review Board at Samsung Medical Center approved the study protocol and waived the requirement for informed consent. The inclusion criteria for the registries were: a) at least 1 CTO detected on a diagnostic coronary angiogram; and b) symptomatic angina and/or a positive functional ischemia study. Exclusion criteria were: a) previous coronary artery bypass graft (CABG); b) a history of cardiogenic shock or cardiopulmonary resuscitation; and c) ST-segment elevation acute MI during the preceding 48hours. CTO lesions were defined as the obstruction of a native coronary artery with a Thrombolysis In Myocardial Infarction (TIMI) flow grade 0 and an estimated duration longer than 3 months.13 Duration was estimated based on the interval from the last episode of acute coronary syndrome. For patients without a history of acute coronary syndrome, duration was estimated from the first episode of exertional angina consistent with the location of the occlusion or previous coronary angiogram. After application of the exclusion criteria, a total of 1547 patients remained. They were stratified according to the definition of coronary segments14 (pmLAD CTO or non-pmLAD CTO) and the initial treatment strategy used (OMT or PCI). A flowchart of patient selection is shown in Figure 1.
Profile of patient enrollment. Analysis based on intention-to-treat. CABG, coronary artery bypass graft; CAG, coronary angiography; CTO, chronic total coronary occlusion; MACE, major adverse cardiac event; MI, myocardial infarction; OMT, optimal medical therapy; PCI, initial percutaneous coronary intervention strategy; PS, propensity score; pmLAD, proximal or middle left anterior descending artery.
The OMT strategy included antiplatelet medication, beta-blockers, renin angiotensin system blockade, nitrates, calcium channel blockers, and aggressive lipid lowering therapy. Medication regimens for all patients were considered as optimal, with doses allowed by heart rate, blood pressure, and symptoms in the absence of justifiable relative contraindications. Coronary interventions were performed using the standard technique. All patients received a 300mg loading dose of aspirin and a 300 to 600mg loading dose of clopidogrel before coronary intervention unless they had previously received these antiplatelet medications. Decisions on performing bilateral injection with the retrograde approach, the type of wire and microcatheter to be used, the use of intravascular ultrasound, and the use of glycoprotein IIb/IIIa receptor inhibitors were at the physician's discretion. Drug-eluting stents were used without restriction. The duration of dual antiplatelet therapy was determined by the treating physician.
Definitions and OutcomesA CTO lesion was defined as an obstruction of a native coronary artery with TIMI flow grade 0 for an estimated duration > 3 months. Duration was based on the interval from the last episode of acute coronary syndrome. For patients without a history of acute coronary syndrome, the duration was from the first episode of effort angina consistent with the location of the occlusion or previous coronary angiography.15–17 Successful revascularization was defined as final residual stenosis<20% and TIMI flow grade ≥ 2 after drug-eluting stent implantation based on visual estimation of the angiograms.15 Coronary angiograms were reviewed by experienced interventional cardiologists blinded to patient data. All deaths were considered to be of cardiac cause unless a definite noncardiac cause could be established.18 MI was defined as recurrent symptoms with new electrocardiogram changes compatible with MI or a cardiac marker level at least twice the normal upper limit.19–21 Repeat revascularization was a composite of target vessel revascularization and nontarget vessel revascularization treated with PCI or CABG.22 The primary outcome was cardiac death during follow-up. Secondary outcomes included MI, repeat revascularization, and major adverse cardiac event (MACE) defined as a composite of cardiac death, recurrent MI, and any revascularization with PCI or CABG during follow-up.
Statistical AnalysisPatients were divided into two subgroups: pmLAD and non-LAD CTO. Data are displayed separately for each group. Continuous variables are expressed as means±standard deviations while categorical variables are presented as absolute numbers and proportions (%). Overall comparisons between groups were performed with the Student t test for continuous variables and the chi-square test or Fisher exact test when the Cochran rule was not met for categorical variables. A Cox proportional hazards model was used to estimate the hazard ratio (HR) and 95% confidence interval (95%CI) for clinical outcomes between the 2 groups. Additionally, sensitivity analyses were performed to estimate hazard rates for other survival events with competing risks and we used the Fine and Gray's competing risk proportional hazard model23,24; a) cardiac death (competing risk=noncardiac death), b) MACE (which included cardiac death) (competing risk=noncardiac death), and c) each component of MACE (competing risk=all-cause death). To reduce selection bias for treatment and any other related potential confounding factor, we performed baseline characteristics adjustment for patients through propensity score matching using “psmatching” custom dialogue in conjunction with SPSS version 21 (IBM, Armonk, NY, United States). A full nonparsimonious model was developed that included all variables listed in Table 1. The “psmatching” program performs all analyses in R (R foundation for Statistical Computing, Vienna, Austria) through SPSS R-Plugin (version 2.14.2). The standard nearest-neighbor one-to-one technique was used with a caliper value of 0.05.25 Between the 2 groups, all confounding variables were compared before and after propensity score matching to ensure that a standardized mean difference of 0.1 or less was obtained and none of these baseline variables were significantly different. All tests were 2-tailed. Statistical significance was considered when P<.05.
Baseline Characteristics of Patients With pmLAD and Non-pmLAD CTO
| pmLAD CTO | Total population | Propensity-matched population | ||||
|---|---|---|---|---|---|---|
| OMT (n=307) | PCI (n=504) | Standardized difference | OMT (n=261) | PCI (n=261) | Standardized difference | |
| Male sex | 230 (74.9) | 399 (79.2) | 0.104 | 199 (76.2) | 196 (75.1) | −0.028 |
| Age | 67.3±12.0 | 61.9±11.1 | −0.483 | 66.1±12.1 | 65.8±10.3 | −0.032 |
| Diabetes | 151 (49.2) | 217 (43.1) | −0.124 | 124 (47.5) | 125 (47.9) | 0.008 |
| HT | 199 (64.8) | 301 (59.7) | −0.104 | 168 (64.4) | 164 (62.8) | −0.031 |
| Smoking | 85 (27.7) | 152 (30.2) | 0.054 | 76 (29.1) | 72 (27.6) | −0.033 |
| CKD | 31 (10.1) | 42 (8.3) | −0.064 | 24 (9.2) | 30 (11.5) | 0.083 |
| Dyslipidemia | 71 (23.1) | 155 (30.8) | 0.165 | 66 (25.3) | 70 (26.8) | 0.033 |
| History of PCI | 74 (24.1) | 91 (18.1) | −0.157 | 64 (24.5) | 59 (22.6) | −0.050 |
| History of MI | 108 (35.2) | 104 (20.6) | −0.359 | 79 (30.3) | 75 (28.7) | −0.038 |
| History of stroke | 34 (11.1) | 43 (8.5) | −0.091 | 28 (10.7) | 30 (11.5) | 0.027 |
| Multiple CTOs | 71 (23.1) | 87 (17.3) | −0.155 | 52 (19.9) | 49 (18.8) | −0.030 |
| Multivessel disease | 275 (89.6) | 367 (72.8) | −0.376 | 229 (87.7) | 235 (90.0) | 0.052 |
| Abrupt stump | 153 (49.8) | 211 (41.9) | −0.161 | 142 (54.4) | 140 (53.6) | 0.016 |
| Bridge collaterals | 125 (40.7) | 156 (31.0) | −0.211 | 105 (40.2) | 101 (38.7) | −0.033 |
| Calcification | 78 (25.4) | 96 (19.0) | −0.162 | 61 (23.4) | 65 (24.9) | 0.039 |
| Rentrop grade 3 | 107 (34.9) | 178 (35.3) | 0.010 | 91 (34.9) | 90 (34.5) | −0.008 |
| SYNTAX score | 25.2±8.8 | 23.8±7.3 | −0.208 | 25.0±8.8 | 24.7±7.8 | −0.044 |
| Year of index procedure | 2007 (2005-2009) | 2008 (2006-2010) | 0.174 | 2007 (2005-2009) | 2008 (2005-2009) | 0.090 |
| non-pmLAD CTO | Total population | Propensity-matched population | ||||
|---|---|---|---|---|---|---|
| OMT (n=357) | PCI (n=379) | Standardized difference | OMT (n=258) | PCI (n=258) | Standardized difference | |
| Male sex | 279 (78.2) | 314 (82.8) | 0.124 | 208 (80.6) | 207 (80.2) | −0.010 |
| Age | 64.8±10.4 | 61.0±10.4 | −0.362 | 63.2±10.5 | 63.1±10.2 | −0.014 |
| Diabetes | 167 (46.8) | 167 (44.1) | −0.055 | 122 (47.3) | 118 (45.7) | −0.031 |
| HT | 240 (67.2) | 246 (64.9) | −0.049 | 176 (68.2) | 170 (65.9) | −0.049 |
| Smoking | 97 (27.2) | 133 (35.1) | 0.166 | 74 (28.7) | 75 (29.1) | 0.008 |
| CKD | 30 (8.4) | 26 (6.9) | −0.143 | 23 (8.9) | 17 (6.6) | −0.092 |
| Dyslipidemia | 87 (24.4) | 134 (35.4) | 0.230 | 76 (29.5) | 66 (25.6) | −0.081 |
| History of PCI | 134 (37.5) | 87 (23.0) | −0.346 | 75 (29.1) | 79 (30.6) | 0.037 |
| History of MI | 103 (28.9) | 76 (20.1) | −0.219 | 67 (26.0) | 57 (22.1) | −0.097 |
| History of stroke | 33 (9.2) | 23 (6.1) | −0.133 | 20 (7.8) | 17 (6.6) | −0.049 |
| Multiple CTOs | 23 (6.4) | 43 (11.3) | 0.154 | 19 (7.4) | 20 (7.8) | 0.012 |
| Multivessel disease | 242 (67.8) | 228 (60.2) | −0.156 | 133 (51.6) | 166 (64.3) | 0.008 |
| Abrupt stump | 182 (51.0) | 174 (45.9) | −0.102 | 140 (49.0) | 131 (50.8) | 0.016 |
| Bridge collaterals | 111 (31.1) | 109 (28.8) | −0.051 | 80 (31.0) | 76 (29.5) | −0.034 |
| Calcification | 38 (10.6) | 44 (11.6) | 0.030 | 31 (12.0) | 29 (11.2) | −0.024 |
| Rentrop 3 | 129 (36.1) | 154 (40.6) | 0.091 | 99 (38.4) | 99 (38.4) | <0.001 |
| SYNTAX score | 15.1±7.7 | 14.0±7.3 | −0.143 | 14.5±7.6 | 14.4±7.1 | −0.011 |
| Year of index procedure | 2007 (2005-2009) | 2008 (2006-2010) | 0.226 | 2008 (2005-2010) | 2008 (2006-2010) | 0.051 |
CKD, chronic kidney disease; CTO, chronic total coronary occlusion; HT, hypertension; MI, myocardial infarction; OMT, optimal medical therapy; PCI, percutaneous coronary intervention; pmLAD, proximal or middle left anterior descending coronary artery.
Values are expressed as mean±standard deviation or No. (%)
Between March 2003 and February 2012, total 14 634 patients underwent coronary angiography. Among them, 2024 (13.8%) patients had at least 1 CTO. Among the 2024 registered patients, 477 patients who underwent CABG were excluded. The remaining 1547 patients were divided into the pmLAD CTO group (n=811) and the non-pmLAD CTO group (n=736) according to angiographic classification of the CTO segment (Figure 1). On univariate and multivariate analyses, the pmLAD CTO group was found to have a significantly higher risk of cardiac death than the non-pmLAD CTO group (Table 1 of the supplementary data).
Among patients who underwent the initial PCI strategy, complete revascularization was performed in more than 50% (n=471, 53.4%). There were no significant differences in the rate of complete revascularization between the pmLAD CTO (n=258, 51.2%) and non-pmLAD CTO (n=213, 56.4%) groups (P=.14). There were no significant differences in the incidence of left, right, and balanced coronary dominance between the pmLAD CTO and non-pmLAD CTO groups. Almost all patients had right coronary dominance in the pmLAD CTO (n=744, 91.7%) and non-pmLAD CTO (n=674, 91.6%) groups (P=.96). The completeness of follow-up was 92.9% and the median duration was 45.9 (interquartile range, 22.9 to 71.1) months. During follow-up, 97 cardiac deaths occurred (61 [7.5%] in the pmLAD CTO group vs 36 [4.9%] in the non-pmLAD CTO group, P=.012), and 114 noncardiac deaths occurred (61 [7.5%] in the pmLAD CTO group vs 53 [7.2%] in the non-pmLAD CTO group, P=.81).
Patients With Chronic Total Coronary Occlusion of the Proximal or Middle Left Anterior Descending ArteryTotal PopulationOf the pmLAD CTO group, 504 (61.2%) patients were classified into the PCI group and 307 (38.8%) patients were classified into the OMT group according to the initial treatment strategy. In the pmLAD CTO group, more patients with old age, previous MI or PCI, multivessel disease, and difficult lesion subsets (such as the presence of abrupt stump, bridge collateral, or calcification) were treated with OMT only. A total of 61 cardiac deaths occurred during follow-up in the pmLAD CTO group. The median length of follow-up was 46.4 months (interquartile range, 21.8-74.4 months).
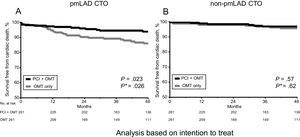
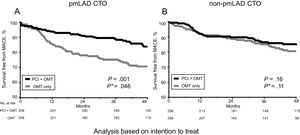
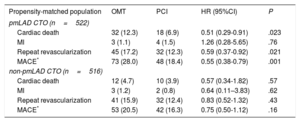
Propensity Score-matched PopulationAfter propensity score matching, 261 pairs were generated. There was no significant difference in baseline clinical or angiographic characteristics in these propensity score-matched participants (Table 1). A total of 50 cardiac deaths occurred during follow-up in the matched patients. The PCI strategy was associated with a lower incidence of cardiac death (PCI vs OMT: 6.9% vs 12.3%; HR, 0.51, 95%CI, 0.29–0.91, P=.023) and less MACE (PCI vs OMT: 18.4% vs 28.0%; HR, 0.55, 95%CI, 0.38–0.79, P=.001) (Figure 2A, Figure 3A, Table 2). This result was consistent after the performance of Fine and Gray competing risks proportional hazards model (Table 2 of the supplementary data).24,25
Kaplan-Meier curves for cardiac death by PCI vs OMT in the pmLAD group (A) and non-pmLAD group (B) after propensity score matching. CTO, chronic total coronary occlusion; OMT, optimal medical therapy; PCI, initial percutaneous coronary intervention strategy; pmLAD, proximal or middle left anterior descending artery. *P values were estimated with the use of a Fine-Grey subdistribution hazards model.
Kaplan-Meier curves for MACE by PCI vs OMT in pmLAD group (A) and non-pmLAD group (B) after propensity score matching. CTO, chronic total coronary occlusion; MACE, major adverse cardiac event; OMT, optimal medical therapy; PCI, initial percutaneous coronary intervention strategy; pmLAD, proximal or middle left anterior descending artery. *P values were estimated with the use of a Fine-Grey subdistribution hazards model.
Clinical Outcomes With OMT Versus PCI in the Propensity-matched Population
| Propensity-matched population | OMT | PCI | HR (95%CI) | P |
|---|---|---|---|---|
| pmLAD CTO (n=522) | ||||
| Cardiac death | 32 (12.3) | 18 (6.9) | 0.51 (0.29-0.91) | .023 |
| MI | 3 (1.1) | 4 (1.5) | 1.26 (0.28-5.65) | .76 |
| Repeat revascularization | 45 (17.2) | 32 (12.3) | 0.59 (0.37-0.92) | .021 |
| MACE* | 73 (28.0) | 48 (18.4) | 0.55 (0.38-0.79) | .001 |
| non-pmLAD CTO (n=516) | ||||
| Cardiac death | 12 (4.7) | 10 (3.9) | 0.57 (0.34-1.82) | .57 |
| MI | 3 (1.2) | 2 (0.8) | 0.64 (0.11–3.83) | .62 |
| Repeat revascularization | 41 (15.9) | 32 (12.4) | 0.83 (0.52-1.32) | .43 |
| MACE* | 53 (20.5) | 42 (16.3) | 0.75 (0.50-1.12) | .16 |
95%CI, 95% confidence interval; CTO, chronic total coronary occlusion; HR, hazard ratio; MACE, major adverse cardiac events; MI, myocardial infarction; OMT, optimal medical therapy; PCI, percutaneous coronary intervention; pmLAD, proximal or middle left anterior descending artery.
Unless otherwise indicated, values are expressed as No. (%).
In patients with non-pmLAD CTO, 357 (48.5%) were classified into the PCI group and 379 (51.5%) were classified into the OMT group according to the initial treatment strategy. More patients with old age, previous MI or PCI, and multiple vessel disease were treated with OMT only. A total of 36 cardiac deaths occurred during the follow-up of these non-pmLAD CTO patients. The median length of follow-up was 44.9 (interquartile range, 23.4–67.7) months.
Propensity Score-matched PopulationAfter propensity score matching, 258 pairs were generated. There was no significant difference in baseline clinical or angiographic characteristics in these propensity score-matched patients (Table 1). A total of 22 cardiac deaths occurred during follow-up of these matched patients. Cardiac death during follow-up was not significantly different between the PCI and OMT groups (PCI vs OMT: 3.9% vs 4.7%, HR, 0.57, 95%CI, 0.34–1.82, P=.57). The rates of MI, repeat revascularization, and MACE were not significantly (P >.05) different between the 2 groups (Figure 2B, Figure 3B, Table 2). After we accounted for noncardiac death as a competing risk, the probability of cardiac death and MACE also showed no difference between the groups (Table 2 of the supplementary data).
Per-protocol Analysis (Successful Percutaneous Coronary Intervention, or Optimal Medical Therapy/Failed Percutaneous Coronary Intervention)The overall CTO PCI success rate was 79.2% (699 of 883 cases). In the pmLAD CTO group, the CTO PCI success rate was 81.2% (409 of 504 cases). In the non-pmLAD CTO group, the CTO PCI success rate was 76.5% (290 of 379 cases). There was no significant difference in the success rate of CTO PCI (P=.44). The results of per-protocol analysis showed a significantly lower incidence of cardiac death (HR, 0.35; 95%CI, 0.18–0.71, P=.003) in successful PCI in patients with pmLAD CTO compared with those with OMT/failed PCI. In contrast, there was no significant difference in the rate of cardiac death between the successful PCI and OMT/failed PCI groups of patients with non-pmLAD CTO (HR, 0.57; 95%CI, 0.22–1.45, P=.57). The results were consistent with the intention-to-treat analysis (initial PCI or initial OMT only strategy) (Table 3 of the supplementary data).
DiscussionThe principal findings of this study are as follows: a) patients with pmLAD CTO had worse clinical outcomes than patients with non-pmLAD CTO; b) patients with pmLAD CTO who underwent PCI had a significantly lower risk of cardiac death and less MACE than those treated with OMT alone; c) in patients with non-pmLAD CTO, PCI failed to reduce cardiac death, repeat revascularization, or MACE compared with OMT during the follow-up period in the propensity-matched population.
Our hypothesis was that a revascularization strategy by PCI could confer advantages to patients with pmLAD CTO lesions compared with an OMT only strategy. For patients with acute MI treated with thrombolysis9 or PCI,10 patients with a pmLAD culprit lesion have a worse survival rate than those with non-pmLAD. For patients with stable ischemic heart disease,11,26 those with an occluded LAD lesion have a worse survival rate than those with non-LAD lesions. These results might be because a larger myocardial territory is supplied by the pmLAD. A larger area of myocardium is known to be associated with pmLAD-related infarcts. Our findings revealed that, consistent with previous studies, worse clinical outcomes depended on the occluded CTO lesion.
Since the inception of revascularization by PCI, there has been no convincing evidence to show that it can improve survival compared with an OMT only strategy in patients with stable ischemic heart disease.27,28 Nonetheless, survival has been improved by revascularization in some selected patients with severe coronary artery disease who are at high risk of an adverse cardiovascular event due to a large amount of myocardium supplied by the diseased vessel.29,30 These patients include the following: a) those with left main equivalent disease; b) those with 3-vessel coronary artery disease; and c) those with 2 vessel disease with more than 75 percent stenosis in the pLAD. A meta-analysis has also shown that revascularization by CABG or PCI is associated with fewer adverse cardiovascular events than OMT in patients with high-risk coronary artery disease30,31 or those with documented myocardial ischemia.32,33 Although some of these studies have included patients with CTO lesions, few such analyses have been carried out. Therefore, we investigated the clinical outcomes of an OMT strategy in patients with CTO compared with those receiving a PCI strategy in high risk coronary artery disease with pmLAD CTO.
A growing body of evidence has shown that successful PCI of CTO is associated with better symptom relief and long-term survival compared with failed PCI.4,34 However, other studies have reported inconsistent benefits, particularly in patients with total occlusion of the infarct-related artery after MI.7,35,36 Furthermore, previous studies have focused on the association of successful PCI of CTO with clinical outcomes compared with failed PCI of CTO among patients. Our previous study has shown that PCI as an initial treatment strategy of CTO is not superior to OMT alone.8 In contrast, this study revealed that, for a subpopulation of high risk CTO patients, an initial revascularization strategy by PCI of pmLAD CTO was associated with a reduction in cardiac death and MACE. However, this reduction was not evident in patients with non-pmLAD CTO.
Study LimitationsThis study has several limitations. First, the study design was nonrandomized due to the nature of the registry data. Therefore, the results could have been affected by residual confounding. Second, we lacked comprehensive data on possible alterations of medical therapies over the follow-up period. Finally, the present analysis included patients who were treated over a long period. During such a long time, changes in PCI strategies might have impacted the clinical outcomes.
ConclusionsOur results suggest that patients with pmLAD CTO have better long-term survival when PCI is used as the initial treatment strategy compared with an OMT strategy only. This survival benefit was not evident among patients with non-pmLAD CTO. This information might be used for selecting patients for CTO PCI.
CONFLICTS OF INTERESTNone declared.
- –
An initial PCI strategy in CTO may not reduce the risk of adverse cardiac events compared with an OMT strategy. Therefore, it is important to select patients who are likely to have a survival benefit from revascularization by PCI.
- –
Patients with pmLAD CTO have better long-term survival when PCI is used as an initial treatment strategy compared with those receiving an OMT strategy only. This survival benefit is not evident among patients with non-pmLAD CTO. Further studies are needed to verify whether the subgroup of patients with pmLAD CTO benefit from PCI of this lesion, as reflected in a reduction in subsequent MI and repeat revascularization and longer survival.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2018.07.011.