Episodes of extreme heat are associated with increased morbidity and mortality in chronically-ill patients but there is a need to clearly establish the relationship between extreme heat and myocardial infarction. The aim of this study was to analyze the relationship between the incidence of ST-segment elevation myocardial infarction (STEMI) and maximum temperature, in particular during heat wave alert periods (HWAP).
MethodsThe population studied consisted of confirmed STEMI cases registered in the Infarction Code of the Community of Madrid between June 2013 and June 2017. Incidence rate ratios (IRR) adjusted for trend and seasonality and 95%CI were estimated using time series regression models.
ResultsA total of 6465 cases of STEMI were included; 212 cases occurred during the 66-day period of HWAP and 1816 cases during the nonalert summer period (IRR, 1.14; 95%CI, 0.96-1.35). The minimum incidence rate was observed at the maximum temperature of 18°C. Warmer temperatures were not associated with a higher incidence (IRR,1.03; 95%CI, 0.76-1.41), whereas colder temperatures were significantly associated with an increased risk (IRR, 1.25; 95%CI, 1.02-1.54). No effect modification was observed by age or sex.
ConclusionsWe did not find an increased risk of STEMI during the 66 days of HWAP in the Community of Madrid between June 2013 and June 2017. However, an increased risk was found during colder temperatures. No extra health resources for STEMI management are required during periods of extreme heat, but should be considered during periods of cold weather.
Keywords
There is growing concern regarding the risk of an increased frequency of extreme heat episodes related to climate change.1–3 Extreme temperatures stress the body, favoring destabilization in chronically ill patients. Numerous authors have reported increased mortality and hospitalizations with extreme temperatures in general4–6 and during episodes described as “heat waves” in particular,7–9 mainly in relation to chronic kidney, respiratory, and heart diseases. Meteorological factors can also trigger acute episodes. There is abundant evidence of an increased incidence of myocardial infarction during periods of cold weather.10–16 The association between extreme heat and acute coronary syndrome is less obvious and, therefore, controversial. Several studies have found an increase in infarction-related hospitalizations,8,11,13,17 whereas others have observed no increase in the incidence of infarction18,19 but have seen a rise in other cardiovascular problems. The aim of this study was to analyze the relationship between ambient temperature and the overall incidence of ST-segment elevation myocardial infarction (STEMI), but most particularly with episodes described as “heat waves.”
METHODSPopulation and Infarction Code registry of the Community of MadridThe study population included all STEMI cases confirmed after cardiac catheterization and included in the Infarction Code registry of the Community of Madrid between June 2013 and June 2017.
Infarction Code Madrid is a program designed to coordinate STEMI reperfusion therapy in the Community of Madrid20 and was implemented on 3 June 2013. All activations are initially recorded by the out-of-hospital emergency services. Data include basic demographic information, date/time of onset of symptoms, and date/time/place of care. The registry is completed at the referral hospitals and includes details on catheterization and primary angioplasty, if performed, and on survival at hospital discharge. The registry is audited regularly, most recently on 22 June 2017, the time point used to end this study. The registry does not include all STEMI cases in the Community of Madrid, as it does not encompass private health care or public hospitals without a 24-hour alert system for primary angioplasty.
An Infarction Code alert activates the system but does not presuppose a STEMI diagnosis, and STEMI is not the final diagnosis in a substantial percentage of patients. To eliminate those patients, individuals were only included after identification of a culprit plaque.
The study investigators obtained an anonymized version from the registry custodian. This version was then used to obtain the age, sex, date/time of symptom onset, health care measures taken, and survival at hospital discharge. For this study, the first date/time listed in the registry was taken. The project was approved by the Ethics Committee of Hospital Universitario Príncipe de Asturias (Alcalá de Henares) of the Infarction Code Madrid network.
Meteorological data and definition of heat waveMeteorological data were obtained from the AEMET (Spanish Agency of Meteorology), a government agency with a national network of weather stations.21 The Community of Madrid has a Mediterranean climate, with large temperature variations over the course of a year. Although there are slight differences in the climate of the flat plains and mountainous regions, the land area of the Community of Madrid (8030km2) is small, and most of the population (more than 90% of the Community's 6.5 million inhabitants) lives in the capital and the metropolitan area.22 Consequently, previous studies have taken only one of the weather stations in the network as a reference for temperatures in the Community of Madrid.23 For this study, we requested that the AEMET provide daily data on the maximum, minimum, and mean temperatures at the Getafe weather station, as a reference for the Community of Madrid within the metropolitan area.
Episodes of extreme heat were considered to be alert periods of risk level 2 (high risk) issued by the Directorate General for Public Health of the Community of Madrid during the study period.24 High risk is assumed to exist when the maximum temperature forecast for that day or any of the next 4 days is above 38.5°C or when there are more than 3 consecutive days with a temperature above 36.5°C.
Statistical analysisThe incidence rate (IR) for STEMI in the population older than 14 years in the Community of Madrid was calculated, using as numerator the number of valid cases in the Infarction Code Madrid registry and as denominator, the population older than 14 years in the Community of Madrid according to the census for the respective year (measured on 1 January, official data from the National Institute of Statistics),25 multiplied by the number of days in the period analyzed. The IRs for days with a heat wave alert were estimated, and the alert-free days were divided into 2 periods (June-September and October-May). IR values are expressed as the total in million person-days and stratified by sex and age bracket (age < 65 years and ≥ 65 years). STEMI incidence rate ratios (IRRs) were calculated for heat wave alert periods (HWAP) vs alert-free periods.
To control for confounding by trend and seasonality in the STEMI IR, IRRs were estimated by time series regression models, with quasi-Poisson regression using a generalized linear model,26 such that:
Yt ∼ quasi-Poisson (nt×μt)
log (μt)=b0+log (nt)+s (t, 8 df/year)+b1 dayst+b2 holidayst+b3 summerpopt+b4hwapt
wherein t is the observation day, n is the exposed population, and s is a natural cubic smoothing spline function with 8 degrees of freedom (df) per year, to adjust for trend and seasonality. The variable designated days corresponds to the days of the week, to control for short-term variations; the variable holidays identifies holidays in the Community of Madrid, and summerpop refers to the summer holidays between 15 July and 31 August, in order to control for the large decline in population at this time of year.27 The variable hwap identifies HWAPs, taking as a reference alert-free days in the summer (June-September). Because temperature-related effects on health are not always immediate and some authors report delays of several days or even weeks,28 the IRRs were evaluated on the actual alert day (lag0) as well as up to 4 days afterward to evaluate lag effects (lag1 to lag4).
Last, the effect of maximum temperature (in °C) was assessed, using the following regression model:
Yt ∼ quasi-Poisson (nt×μt)
log (μt)=b0+log (nt)+s (t, 8 df/year)+b1 dayst+b2 holidayst+b3 summerpopt+cb (tempt)
wherein temp is now the maximum temperature modeled by a distributed lag nonlinear model.29 This type of model is suitable for describing the complex nonlinear time-lag dependencies usually found in the case of temperature effects in health, using a combination of 2 functions defining the exposure-response and lag-response relationships. More specifically, the temperature-STEMI IR relationship was modeled using a natural cubic smoothing spline function with 3 nodes at the 10th, 75th, and 90th percentiles for the maximum temperature distribution.30 The lag-STEMI IR relationship was modeled with a cubic smoothing spline function, using 3 equally spaced internal nodes, with cumulative lags of 14 days to capture the most delayed effects for the cold period as well.15,30 These modeling options were checked using various sensitivity analyses.
All statistical analyses were performed using Stata, version 15 (StataCorp; College Station, Texas, United States).
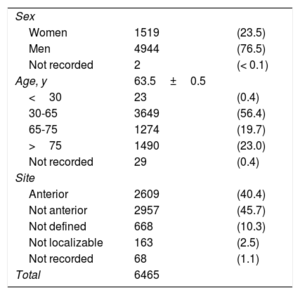
RESULTSDuring the study period (June 2013 to June 2017), 8814 alerts were recorded. The STEMI diagnosis was confirmed following a cardiac catheterization procedure in 6465 patients. Men accounted for 76.5%, and the mean age was 63 (range, 15-101) years. Among the alerts recorded, 358 patients died, with an inpatient mortality of 5.6% (table 1).
Characteristics of STEMI cases
| Sex | ||
| Women | 1519 | (23.5) |
| Men | 4944 | (76.5) |
| Not recorded | 2 | (< 0.1) |
| Age, y | 63.5±0.5 | |
| <30 | 23 | (0.4) |
| 30-65 | 3649 | (56.4) |
| 65-75 | 1274 | (19.7) |
| >75 | 1490 | (23.0) |
| Not recorded | 29 | (0.4) |
| Site | ||
| Anterior | 2609 | (40.4) |
| Not anterior | 2957 | (45.7) |
| Not defined | 668 | (10.3) |
| Not localizable | 163 | (2.5) |
| Not recorded | 68 | (1.1) |
| Total | 6465 | |
STEMI, ST-segment elevation myocardial infarction.
Data are expressed as No. (%) or as mean±standard deviation.
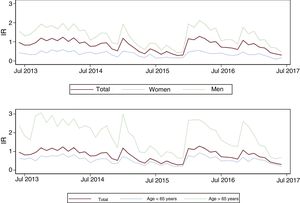
figure 1 shows the monthly trend of STEMI IR during the study period, overall and stratified by sex and age bracket. The IR was higher in men and in people older than 65 years. No long-term upward or downward trend was observed, but there were some cyclical fluctuations, with maximum IR values seen in winter months and minimum values observed in the summer.
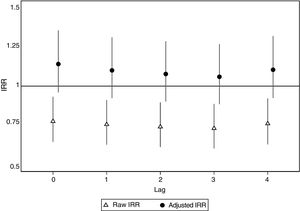
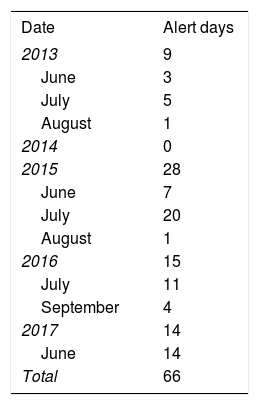
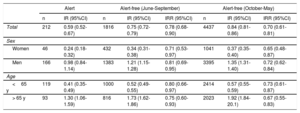
Table 2 lists the days when the Community of Madrid activated heat alert level 2. Detailed information on the days and the maximum and minimum temperatures are provided in table 1 of the supplementary data. A total of 212 STEMI cases were recorded during the 66 days identified as HWAP, compared with 1816 cases on alert-free days between June and September (IRR=0.78; 95% confidence interval [95%CI], 0.68-0.90) and 4437 cases between October and May (IRR=0.70; 95%CI, 0.61-0.81) (table 3). The IRR was not substantially modified after stratification by sex and age bracket (table 3). In contrast, IRR adjusted by trend and seasonality showed an increase during HWAPs compared with alert-free days (IRR=1.14; 95%CI, 0.96-1.35), although this was not statistically significant (figure 2). Likewise, no statistically significant increase was observed during the following 4 days (lag1 to lag4) after the heat wave alert (figure 2). The adjusted IRR showed practically no change by sex or age bracket (figure 1 of the supplementary data).
Incidence rates of ST-segment elevation myocardial infarction on level 2 (high risk) heat alert days in the Community of Madrid and on alert-free days, grouped into 2 periods (June-September and October-May)
| Alert | Alert-free (June-September) | Alert-free (October-May) | ||||||
|---|---|---|---|---|---|---|---|---|
| n | IR (95%CI) | n | IR (95%CI) | IRR (95%CI) | n | IR (95%CI) | IRR (95%CI) | |
| Total | 212 | 0.59 (0.52-0.67) | 1816 | 0.75 (0.72-0.79) | 0.78 (0.68-0.90) | 4437 | 0.84 (0.81-0.86) | 0.70 (0.61-0.81) |
| Sex | ||||||||
| Women | 46 | 0.24 (0.18-0.32) | 432 | 0.34 (0.31-0.38) | 0.71 (0.53-0.97) | 1041 | 0.37 (0.35-0.40) | 0.65 (0.48-0.87) |
| Men | 166 | 0.98 (0.84-1.14) | 1383 | 1.21 (1.15-1.28) | 0.81 (0.69-0.95) | 3395 | 1.35 (1.31-1.40) | 0.72 (0.62-0.84) |
| Age | ||||||||
| <65 y | 119 | 0.41 (0.35-0.49) | 1000 | 0.52 (0.49-0.55) | 0.80 (0.66-0.97) | 2414 | 0.57 (0.55-0.59) | 0.73 (0.61-0.87) |
| > 65 y | 93 | 1.30 (1.06-1.59) | 816 | 1.73 (1.62-1.86) | 0.75 (0.60-0.93) | 2023 | 1.92 (1.84-20.1) | 0.67 (0.55-0.83) |
95%CI, 95% confidence interval; IR, incidence rate; IRR, incidence rate ratio.
For alert-free periods, the IR and the raw IRRs comparing the incidence between alert and alert-free periods are included, not adjusted for trend and seasonality.
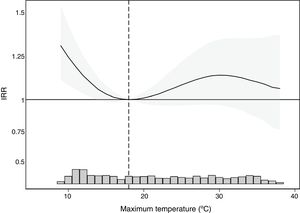
The lowest STEMI IR was recorded when the maximum temperature was 18°C. figure 3 shows the STEMI IRR associated with various maximum temperature values compared with this reference value, indicating a statistically significant increase in IR associated with colder temperatures (lowest maximums). Conversely, no increase was observed in the IR associated with warm temperatures. When we used the temperatures of 10°C and 35°C corresponding to the 5th and 95th percentiles of the maximum temperature distribution as the arbitrary indicators of cold and heat, the IRR was significantly higher at cold (IRR=1.25; 95%CI, 1.02-1.54) but not warm (IRR=1.03; 95% CI, 0.76-1.41) temperatures than at the temperature with the lowest IR. The relationship between maximum temperature and STEMI IRR was unchanged by sex or age bracket (figure 2 of the supplementary data).
DISCUSSIONThis study was carried out with a large series of STEMI cases seen over a 4-year period by a public health care network in a single geographical region with large temperature variations and numerous heat waves of differing duration and intensity during this period. The results do not support the hypothesis that high temperatures raise the incidence of STEMI on the days of a heat wave or on the following 4 days. Nevertheless, it does confirm that the risk of STEMI rises during periods with colder temperatures.
Previous studies have clearly shown that mortality and hospitalizations increase during periods of extreme heat.4–9 A large part of this increase is attributed to decompensation of chronic diseases, particularly kidney and respiratory diseases and, to a lesser extent, to cardiovascular diseases.7–9 Elderly individuals would be those most vulnerable to heat-related injury.23
Extreme heat could also act as a trigger of acute cardiovascular events, which is why tachycardia, endothelial dysfunction, and hypercoagulability are considered potential causal mechanisms.31 It has been reported that heat stroke may resemble STEMI.32 Nevertheless, the relationship between extreme heat and myocardial infarction is not clearly established. In Ontario, Canada, a population registry collected 443447 cases of myocardial infarction between 1996 and 2013, but found no increase in risk at temperatures above the 99th percentile, although there was an increase in hospitalizations due to cardiovascular disease.4 In Japan, a nationwide coronary interventional registry collected 56863 STEMIs treated by primary angioplasty over a 1-year period,11 observing, as in our study and others,4,15 a negative correlation between temperature and STEMI incidence, with no increase in risk associated with maximum summer temperatures. Nevertheless, this study did find that an increase in temperature on the previous day was associated with an increased risk of infarction at all times of year. In England and Wales, the MINAP database17 included 24861 hospitalizations due to myocardial infarction during the months of June to August between 2003 and 2009. For each 1°C increase in maximum temperature above an optimal threshold of 20°C, the risk of infarction increased by 1.9% within 1 to 6hours after exposure. In Michigan, between 2000 and 2009, an increase was reported in infarction-related hospitalizations only when the temperature was above the 99th percentile of usual temperatures.8 A comparison between the Paris heat wave in August 2003 and the same period in other years with no heat waves found an increase in out-of-hospital cardiac arrests in persons older than 60 years, but not in infarctions.18 An increase in infarctions was also not observed during the heat wave affecting Apulia (southern Italy) in July 2011, although there was an increase in atrial fibrillation episodes.19 The SWEDEHEART database16 showed an almost linear decrease in the risk of infarction as minimum temperatures rose from 0°C to 20°C. Previous studies report somewhat contradictory data and, therefore, do not seem to clearly show that myocardial infarctions increase during periods of extreme heat, although there is some evidence of an optimal temperature threshold after which, particularly in the case of cold temperatures, or to a lesser extent, hot temperatures, there may be an increased risk of infarction.4,5,10–13,17 This is consistent with our results, which show that the maximum temperature with the lowest IR recorded was 18°C.
The definition of heat wave is arbitrary, both in terms of the thresholds selected24 and the actual temperatures involved: in Stockholm a heat wave is declared when temperatures rise above 26°C, whereas in Rome the threshold is above 35.9°C. A pleasant springtime temperature for a Roman would mean an increased likelihood of mortality in Stockholm, including among myocardial infarction survivors.9 Heat-related deaths are similar in areas of extreme heat, such as Athens, and Finland, with completely different temperatures with minimal mortality.33 Although the above data could be partly explained by the effects of humidity, recent data indicate that populations learn to protect themselves from the effects of heat. A reduction has been reported in the lethal effect of heat in the Spanish population, dropping from a relative risk of 1.14 between 1983 and 2003, to a risk of 1.01 between 2004 and 2013.34 This reduction in the risk of heat-related mortality is observed worldwide35 and could be attributed to economic development, which would allow better measures to be taken to handle heat, as well as to the effects of prevention campaigns, among them, heat alerts.34,35 Our study observed a statistically significant decrease in raw IR during HWAPs, compared with alert-free periods, but this decrease disappeared after adjustment for trend and seasonality; hence, we conclude that there was no increase or decrease in the risk of STEMI during HWAPs in the overall population or in the groups analyzed by sex and age.
LimitationsThe Infarction Code Madrid registry does not include all STEMI cases and, therefore, the calculated rates underestimate the actual rates. This underestimation may be somewhat larger because STEMIs were included only if confirmed after catheterization. In certain clinical situations, a few patients with STEMI may have been treated conservatively. However, we believe that the underestimation due to these 2 causes is small and would have little effect on the results of a sample as large as that described.
Only STEMIs with confirmed atherothrombosis were included, thus allowing the study to assess a fairly homogeneous pathophysiological process and to detect variations that help predict incidence peaks from STEMI alerts. This could explain why the population is younger than in studies that include all types of infarction, such as that based on the MINAP database.17 In our study, 42% of patients were older than 65 years (23% older than 75 years) and were exposed to higher temperatures than those described in the British study. Therefore, we do not believe that the age difference (65 years in our study vs 69 years in MINAP) alone explains the differing results.
The study could have used temperatures from the 8 weather stations of the Community of Madrid and have created patient clusters around each one. These clusters would have to be assigned according to isotherms, which were not available, rather than according to distance, which does not necessarily reflect temperature variations. Because most of the population lives within the metropolitan area, which is geographically homogeneous, and because one of the weather stations is reported to be representative of the temperature in the Community of Madrid, the study was simplified by using those values. The interaction of multiple weather and environmental pollution variables could also have been considered, as these variables could affect the incidence of multiple diseases.2,11 This is a research line to be undertaken in the future.
The definitions of heat wave and alert issuance are necessarily arbitrary. For that reason, the analysis was carried out using heat wave alerts based on forecasts, but also using actual maximum temperatures. The results are consistent between both, which enhances their validity.
Last, the type of study makes it impossible to discern whether no heat-wave effect was observed because extreme heat does not affect the incidence of STEMI or because alerts and prevention measures are effective.
StrengthsThe main strengths of the study are: a) the definition of STEMI validated by cardiac catheterization, which focuses the study on a specific pathophysiological process and makes the presence of false positives highly unlikely, and b) analysis of a time series that controls for trend and seasonality and permits adjustment for variables such as day of the week, holidays, and declines in population due to summer holidays. The impact of these variables is observed on comparison of the raw and adjusted IRR for HWAP days to alert-free days. In fact, the raw IRR indicates a protective effect during heat waves, but this disappears in the adjusted model.
CONCLUSIONSIn the Community of Madrid, HWAPs officially defined between June 2013 and June 2017 were not accompanied by an increase in the incidence of STEMI. This finding could be explained in part by the effectiveness of prevention measures targeting the population and, therefore, it seems unadvisable to relax these measures. Regarding STEMI treatment strategies, additional resources are needed in cold weather periods, as opposed to extreme heat. A strategy to protect the population during cold weather appears to be necessary.
FUNDINGA. Tobías received support from the Japanese Society for the Promotion of the Science (JSPS) in its grant invitation program for research in Japan (S18149).
CONFLICTS OF INTERESTNone declared.
- –
Extreme heat is associated with increased morbidity and mortality due to chronic diseases. Cold temperatures raise the incidence of acute coronary syndromes, including STEMI. However, the relationship between extreme heat and acute coronary syndrome is unclear.
- –
No increase was found in the incidence of STEMI associated with hot weather, including extreme heat. Conversely, the incidence of STEMI rose with cold temperatures, even when not necessarily extreme.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2019.05.016