Although heart failure negatively affects the health-related quality of life of Spanish patients there is little information on the clinical factors associated with this issue.
MethodsCross-sectional multicenter study of health-related quality of life. A specific questionnaire (Kansas City Cardiomyopathy Questionnaire) and a generic questionnaire (EuroQoL-5D) were administered to 1037 consecutive outpatients with systolic heart failure.
ResultsMost patients with poor quality of life had a worse prognosis and increased severity of heart failure. Mobility was more limited and rates of pain/discomfort and anxiety/depression were higher in the study patients than in the general population and patients with other chronic conditions. The scores on both questionnaires were very highly correlated (Pearson r =0.815; P < .001). Multivariable linear regression showed that being older (standardized β=-0.2; P=.03), female (standardized β=-10.3; P < .001), having worse functional class (standardized β=-20.4; P < .001), a higher Charlson comorbidity index (standardized β=-1.2; P=.005), and recent hospitalization for heart failure (standardized β=6.28; P=.006) were independent predictors of worse health-related quality of life.
ConclusionsPatients with heart failure have worse quality of life than the general Spanish population and patients with other chronic diseases. Female sex, being older, comorbidity, advanced symptoms, and recent hospitalization are determinant factors in health-related quality of life in these patients.
Keywords
Patients with chronic heart failure (CHF) have far worse health-related quality of life (HRQoL) than the general population and patients with other chronic diseases.1 Improving HRQoL is one of the main objectives of the comprehensive management of CHF patients.2–4
In CHF patients, HRQoL is a multidimensional measure with good correlation with disease severity,5 provides independent prognostic information, and can assist in assessing the cost-effectiveness of implementing new therapeutic options.6,7
The deterioration of HRQoL in CHF patients is reflected in the dimensions that capture information on the functional limitations that have a particular impact on the mobility or daily activities domains.8
Several authors have addressed the extent to which the HRQoL of CHF patients differs from that of the general population or patients with other chronic diseases, which dimensions or domains of HRQoL are the most affected, and which clinical and demographic factors influence HRQoL. However, there is little information on HRQoL in heart failure (HF) patients in Spain, since publications to date in this field come from substudies of clinical trials or studies conducted in other geographical and cultural settings, and thus it remains unknown if the results are fully transferable to the Spanish setting.9,10
Thus, the aims of the prespecified analysis of the VIDA-IC study, whose first results were published in 2014,11 were: a) to determine the clinical-demographic factors associated with HRQoL in patients with CHF and left ventricular systolic dysfunction followed up in cardiology or internal medicine clinics; b) to assess which dimensions were most affected in these patients, and c) to explore if there was a gradient of total scores and by specific domains in HRQoL instruments between the study patients and the general population or in patients with other chronic conditions in Spain.
METHODSStudy DesignThe VIDA-IC observational descriptive study was conducted throughout Spain from October 2011 to January 2012 by 115 specialists (cardiologists and internal medicine specialists), who included consecutive CHF patients seen in an outpatient clinic.11 The objectives of the study were to assess the level of correlation between specific and generic HRQoL measures in CHF patients, study the factors determining the level of HRQoL, and contextualize the quality of life of HF patients measured with generic scales with the quality of life measured with the same scales in the general population or patients with other chronic diseases in Spain. The latter objective was fulfilled by comparing the general information available in the literature and in public national health surveys on quality of life in the general Spanish population and the population with chronic diseases in Spain. The study protocol was approved by the Ethics and Clinical Research Committee of the Instituto Hospital del Mar de Investigaciones Médicas (IMIM; Barcelona, Spain). All patients gave written informed consent before inclusion in the study.
Study Population and Inclusion and Exclusion CriteriaThe study consecutively included patients attending a specialized outpatient clinic (cardiology or internal medicine) who fulfilled the following inclusion criteria: clinically stable, older than 18 years, and a diagnosis of CHF with systolic dysfunction (left ventricular ejection fraction ≤ 40%) within the last 12 months. Exclusion criteria were: waiting for heart transplantation or correction of valvular lesions, inability to understand or complete the HRQoL questionnaires, noncardiac disease with a life expectancy of less than 1 year, noncardiovascular hospitalization in the month prior to inclusion, or hospitalization at the time of inclusion. Patient inclusion was stratified according to recent (less than 1 month) admission for HF and nonrecent (more than 6 months) admission for HF at a ratio of 1:1 for each of the recruiters. Baseline data were obtained from eligible patients or medical records after they had given informed consent, provided the patients were stable and had no signs of acute decompensation.
Evaluation of Results in Patient-centered Health: Quality of LifeAll patients in the study were asked to complete the self-administered Kansas City Cardiomyopathy Questionnaire (KCCQ)12 and the EuroQoL-5D overall quality of life questionnaire (EQ-5D).13 The KCCQ is specific to patients with HF. It comprises 23 items in 7 domains.
The score on each domain can, in theory, range from 0 to 100, with 100 corresponding to the best state. In addition, 3 summary scores are calculated: the symptoms summary score is derived by summing the scores on the frequency and severity of symptoms (excluding stability); the clinical summary score is derived by summing the scores on the physical limitations and symptoms domains; and the overall summary score is derived by summing the clinical summary score and the quality of life and social limitation scores. The EQ-5D is a generic instrument comprising a visual analogue scale (VAS) of self-rated general health and 5 dimensions (mobility, self-care, daily activities, pain/discomfort, and anxiety/depression). Scores on the VAS can range from 0 (worse state) to 100 (best state). Scores on the 5 dimensions can be expressed as an overall summary index (EQ-5D index) or as the percentage of patients who indicate some kind of problem on each of the dimensions. Both scales have been validated for the Spanish general population.13
The HRQoL of the study patients, the Spanish general population, and patients with other chronic diseases was compared using summary data of the VAS and the 5 dimensions of the EQ-5D. These data were obtained from the most recent Spanish National Health Survey of the general population14 and publications using the EQ-5D to assess HRQoL in Spanish patients with various chronic diseases.15–18
Statistical AnalysisContinuous variables are expressed as mean ± standard deviation and discrete variables as absolute and relative values. Groups with good and poor HRQoL were compared using the chi square test and Student t test (or Mann-Whitney U test as needed) for discrete and continuous variables, respectively. The level of correlation between the overall KCCQ and EQ-5D scores was assessed using correlation coefficients and Spearman's ρ and Pearson's r. Clinical and demographic factors associated with HRQoL were assessed using univariable logistic regression models and univariable linear regression models in which the dependent variables were the overall summary scores of the KCCQ, the EQ-5D index, and the VAS, and the independent variables were specific demographic and clinical factors included in this study. The independent variables were used to construct several exploratory multivariable linear regression models using the backward stepwise method to determine which factors remained independently associated with patient-centered health outcomes. A P value of < .05 was used as a cutoff for statistical significance. All analyses were performed using the SPSS statistical software package version 18 and the Stata statistical software package version 11.
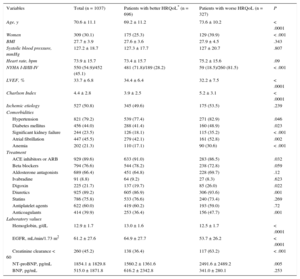
RESULTSA total of 1037 patients with HF and left ventricular systolic dysfunction were included in the study. Of these, 63.2% were recruited by cardiologists and the remaining 36.8% were recruited by internal medicine specialists. A total of 1037 KCCQ, 1020 VAS, and 1009 EQ-5D completed HRQoL questionnaires were available for analysis. Table 1 shows the characteristics of the study patients. Mean age was 72 (interquartile range: 64- 78) years and there was a predominance of men. About half of the patients had ischemic HF and were in New York Heart Association (NYHA) functional class III/IV. In general, patients with worse HRQoL scores on the KCCQ showed data associated with poor prognosis and increased severity of CHF.
Demographic and Clinical Characteristics of all Patients Included in the Study According to Health-related Quality of Life
| Variables | Total (n = 1037) | Patients with better HRQoL* (n = 696) | Patients with worse HRQoL (n = 327) | P |
|---|---|---|---|---|
| Age, y | 70.6 ± 11.1 | 69.2 ± 11.2 | 73.6 ± 10.2 | < .0001 |
| Women | 309 (30.1) | 175 (25.3) | 129 (39.9) | < .001 |
| BMI | 27.7 ± 3.9 | 27.6 ± 3.6 | 27.9 ± 4.5 | .343 |
| Systolic blood pressure, mmHg | 127.2 ± 18.7 | 127.3 ± 17.7 | 127 ± 20.7 | .807 |
| Heart rate, bpm | 73.9 ± 15.7 | 73.4 ± 15.7 | 75.2 ± 15.6 | .09 |
| NYHA I-II/III-IV | 550 (54.9)/452 (45.1) | 481 (71.8)/189 (28.2) | 59 (18.5)/260 (81.5) | < .001 |
| LVEF, % | 33.7 ± 6.8 | 34.4 ± 6.4 | 32.2 ± 7.5 | < .0001 |
| Charlson Index | 4.4 ± 2.8 | 3.9 ± 2.5 | 5.2 ± 3.1 | < .0001 |
| Ischemic etiology | 527 (50.8) | 345 (49.6) | 175 (53.5) | .239 |
| Comorbidities | ||||
| Hypertension | 821 (79.2) | 539 (77.4) | 271 (82.9) | .046 |
| Diabetes mellitus | 456 (44.0) | 288 (41.4) | 160 (48.9) | .023 |
| Significant kidney failure | 244 (23.5) | 126 (18.1) | 115 (35.2) | < .001 |
| Atrial fibrillation | 447 (45.5) | 279 (42.1) | 161 (52.8) | .002 |
| Anemia | 202 (21.3) | 110 (17.1) | 90 (30.6) | < .001 |
| Treatment | ||||
| ACE inhibitors or ARB | 929 (89.6) | 633 (91.0) | 283 (86.5) | .032 |
| Beta blockers | 794 (76.6) | 544 (78.2) | 238 (72.8) | .059 |
| Aldosterone antagonists | 689 (66.4) | 451 (64.8) | 228 (69.7) | .12 |
| Ivabradine | 91 (8.8) | 64 (9.2) | 27 (8.3) | .623 |
| Digoxin | 225 (21.7) | 137 (19.7) | 85 (26.0) | .022 |
| Diuretics | 925 (89.2) | 605 (86.9) | 306 (93.6) | .001 |
| Statins | 786 (75.8) | 533 (76.6) | 240 (73.4) | .269 |
| Antiplatelet agents | 622 (60.0) | 419 (60.2) | 193 (59.0) | .72 |
| Anticoagulants | 414 (39.9) | 253 (36.4) | 156 (47.7) | .001 |
| Laboratory values | ||||
| Hemoglobin, g/dL | 12.9 ± 1.7 | 13.0 ± 1.6 | 12.5 ± 1.7 | < .0001 |
| EGFR, mL/min/1.73 m2 | 61.2 ± 27.6 | 64.9 ± 27.7 | 53.7 ± 26.2 | < .0001 |
| Creatinine clearance < 60 | 260 (45.2) | 138 (36.4) | 117 (63.2) | < .001 |
| NT-proBNP, pg/mL | 1854.1 ± 1829.8 | 1560.2 ± 1361.6 | 2491.6 ± 2489.2 | .005 |
| BNP, pg/mL | 515.0 ± 1871.8 | 616.2 ± 2342.8 | 341.0 ± 280.1 | .253 |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blockers; BMI, body mass index; BNP, brain natriurectic peptide; EGFR, estimated glomerular filtration rate; HRQoL, health-related quality of life; LVEF, left ventricular ejection fraction; NT-proBNP, N-terminal pro-brain natriuretic peptide; NYHA, New York Heart Association.
Data are expressed as No. (%) or mean ± standard deviation.
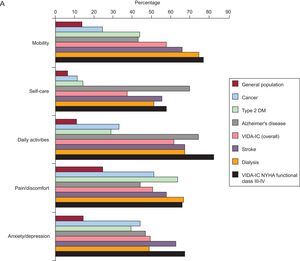
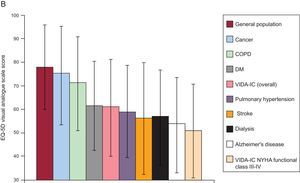
Compared with the general reference population (Figure 1),14–20 the study patients reported more limitations on all the dimensions of the EQ-5D. In some dimensions, such as mobility, pain/discomfort, and anxiety/depression, HF patients had more limitations than patients with chronic diseases, such as diabetes mellitus, cancer, or Alzheimer's disease. Patients with HF and NYHA III/IV comprised almost half the study population and reported similar or higher levels of limitations in the dimensions studied than patients with a history of stroke or those with chronic kidney failure on dialysis. Similar results were obtained when the mean scores of the VAS were analyzed. According to the VAS score, the perceived overall state of health of the study patients with CHF was worse than that of the general population, patients with chronic obstructive pulmonary disease or cancer, and similar to that of patients with diabetes or pulmonary hypertension. Patients with CHF in NYHA functional class III/IV had a lower mean VAS score, indicating a worse perceived overall health state even when compared with patients with a history of stroke or Alzheimer's disease or patients on dialysis.
Comparison of the impact on health-related quality of life in study patients with heart failure compared with the Spanish general population and people with other chronic diseases in Spain. A: percentage of people and patients reporting any limitation in each dimension of the EuroQol-5D. B: comparative analysis of scores (mean ± standard deviation) on the EuroQol-5D visual analogue scale. COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; EuroQoL-5D, EuroQoL-5D overall quality of life questionnaire; HF, heart failure; NYHA, New York Heart Association functional class.
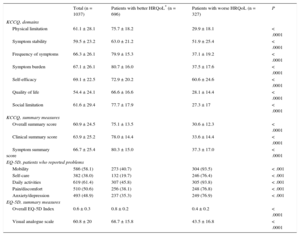
Table 2 shows the average scores of each subdomain of the KCCQ, the summary scores, the mean scores of the EQ-5D index and the VAS, and the percentage of patients with some degree of limitation on each of the EQ-5D. As expected, patients with worse HRQoL scored worse on all these items. Items such as self-efficacy or symptom stability, which are not included in the overall summary, were significantly worse in patients with worse HRQoL. Similarly, patients with an overall summary score on the KCCQ less than 50 points had more limitations on the 5 dimensions of EQ-5D and lower mean scores on this questionnaire and the VAS.
Distribution of the Summary Scores, Dimensions, and Various Domains of Quality-of-life Questionnaires Specific to Heart Failure (Kansas City Cardiomyopathy Questionnaire) and Generic Quality-of-life Questionnaires Used in the Total Study Population According to Health-related Quality of Life
| Total (n = 1037) | Patients with better HRQoL* (n = 696) | Patients with worse HRQoL (n = 327) | P | |
|---|---|---|---|---|
| KCCQ, domains | ||||
| Physical limitation | 61.1 ± 28.1 | 75.7 ± 18.2 | 29.9 ± 18.1 | < .0001 |
| Symptom stability | 59.5 ± 23.2 | 63.0 ± 21.2 | 51.9 ± 25.4 | < .0001 |
| Frequency of symptoms | 66.3 ± 26.1 | 79.9 ± 15.3 | 37.1 ± 19.2 | < .0001 |
| Symptom burden | 67.1 ± 26.1 | 80.7 ± 16.0 | 37.5 ± 17.6 | < .0001 |
| Self-efficacy | 69.1 ± 22.5 | 72.9 ± 20.2 | 60.6 ± 24.6 | < .0001 |
| Quality of life | 54.4 ± 24.1 | 66.6 ± 16.6 | 28.1 ± 14.4 | < .0001 |
| Social limitation | 61.6 ± 29.4 | 77.7 ± 17.9 | 27.3 ± 17 | < .0001 |
| KCCQ, summary measures | ||||
| Overall summary score | 60.9 ± 24.5 | 75.1 ± 13.5 | 30.6 ± 12.3 | < .0001 |
| Clinical summary score | 63.9 ± 25.2 | 78.0 ± 14.4 | 33.6 ± 14.4 | < .0001 |
| Symptom summary score | 66.7 ± 25.4 | 80.3 ± 15.0 | 37.3 ± 17.0 | < .0001 |
| EQ-5D, patients who reported problems | ||||
| Mobility | 586 (58.1) | 273 (40.7) | 304 (93.5) | < .001 |
| Self-care | 382 (38.0) | 132 (19.7) | 246 (76.4) | < .001 |
| Daily activities | 619 (61.4) | 307 (45.8) | 305 (93.8) | < .001 |
| Pain/discomfort | 510 (50.6) | 256 (38.1) | 248 (76.8) | < .001 |
| Anxiety/depression | 493 (48.9) | 237 (35.3) | 249 (76.9) | < .001 |
| EQ-5D, summary measures | ||||
| Overall EQ-5D Index | 0.6 ± 0.3 | 0.8 ± 0.2 | 0.4 ± 0.2 | < .0001 |
| Visual analogue scale | 60.8 ± 20 | 68.7 ± 15.8 | 43.5 ± 16.8 | < .0001 |
EQ-5D, EuroQoL-5D overall quality of life questionnaire; HRQoL, health-related quality of life; KCCQ, Kansas City Cardiomyopathy Questionnaire.
Values are expressed as no. (%) or mean ± standard deviation.
A correlation matrix was used to study the associations between the HRQoL questionnaire variables used in this study (Table 3). The table shows a horizontal and vertical list of the same variables with their correlation coefficients (R) expressed as a number ranging from 0 to 1 and their confidence intervals. Table 3 shows the correlations between the scores on the KCCQ domains and the summary scores of the KCCQ, the EQ-5D index, and the VAS. The correlations between the overall scores of the EQ-5D and KCCQ were very high (Pearson's r=0.815; Spearman's ρ = 0.811; P < .001 for both coefficients). Significantly high correlations (> 0.6) were found between the KCCQ domains and between these domains and the KCCQ and EQ-5D summary scores in all cases where convergent correlation would be expected. Regarding the overall KCCQ scores, the physical limitation domain and total symptoms summary score had very high convergence (coefficients > 0.8). These correlations were relatively lower in relation to the VAS and EQ-5D index. The correlations that, although significant, were more divergent regarding the other dimensions and the KCCQ or the EQ-5D summary scores were those obtained from symptom stability and the self-efficacy domain of the KCCQ (ranges between 0.1 and 0.2 in most cases).
Correlation Matrix (R-values and Confidence Intervals) of the Different Items, Dimensions, Domains, and Summary Scores of the Questionnaires Used to Assess Health-related Quality of Life
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. EuroQoL-5 dimensions score | 1 | |||||||||||
| 2. Visual analogue scale | 0.682 | 1 | ||||||||||
| (0.647-0.714) | ||||||||||||
| 3. Physical limitations | 0.785 | 0.634 | 1 | |||||||||
| (0.759-0.807) | (0.596-0.669) | |||||||||||
| 4. Symptom stability | 0.207 | 0.229 | 0.176 | 1 | ||||||||
| (0.147-0.266) | (0.170-0.286) | (0.116-0.235) | ||||||||||
| 5. Frequency of symptoms | 0.717 | 0.601 | 0.756 | 0.203 | 1 | |||||||
| (0.685-0.745) | (0.560-0.639) | (0.729-0.781) | (0.144-0.261) | |||||||||
| 6. Symptom burden | 0.721 | 0.633 | 0.756 | 0.240 | 0.903 | 1 | ||||||
| (0.689-0.749) | (0.595-0.669) | (0.729-0.781) | (0.182-0.297) | (0.891-0.914) | ||||||||
| 7. Overall symptom score | 0.736 | 0.633 | 0.775 | 0.227 | 0.976 | 0.976 | 1 | |||||
| (0.706-0.763) | (0.594-0.668) | (0.749-0.798) | (0.168-0.284) | (0.972-0.978) | (0.972-0.978) | |||||||
| 8. Self-efficacy | 0.349 | 0.301 | 0.322 | 0.0909* | 0.340 | 0.345 | 0.351 | 1 | ||||
| (0.293-0.402) | (0.244-0.356) | (0.266-0.375) | (0.030-0.151) | (0.284-0.392) | (0.290-0.398) | (0.296-0.403) | ||||||
| 9. Quality of life | 0.701 | 0.629 | 0.695 | 0.210 | 0.779 | 0.788 | 0.802 | 0.318 | 1 | |||
| (0.668-0.731) | (0.591-0.665) | (0.662-0.726) | (0.151-0.268) | (0.754-0.802) | (0.763-0.810) | (0.780-0.823) | (0.262-0.372) | |||||
| 10. Social limitations | 0.751 | 0.645 | 0.822 | 0.208 | 0.790 | 0.795 | 0.812 | 0.300 | 0.815 | 1 | ||
| (0.723-0.777) | (0.607-0.679) | (0.801-0.841) | (0.149-0.266) | (0.766-0.812) | (0.772-0.817) | (0.790-0.832) | (0.243-0.354) | (0.793-0.834) | ||||
| 11. Overall summary score | 0.815 | 0.698 | 0.905 | 0.224 | 0.897 | 0.903 | 0.921 | 0.352 | 0.898 | 0.944 | 1 | |
| (0.792-0.834) | (0.665-0.729) | (0.893-0.916) | (0.165-0.281) | (0.884-0.908) | (0.891-0.914) | (0.912-0.930) | (0.297-0.404) | (0.885-0.909) | (0.937-0.951) | |||
| 12. Clinical summary score | 0.807 | 0.672 | 0.948 | 0.211 | 0.913 | 0.913 | 0.936 | 0.358 | 0.792 | 0.866 | 0.968 | 1 |
| (0.784-0.828) | (0.637-0.705) | (0.941-0.954) | (0.152-0.269) | (0.903-0.923) | (0.903-0.923) | (0.928-0.943) | (0.303-0.410) | (0.768-0.814) | (0.850-0.881) | (0.964-0.972) |
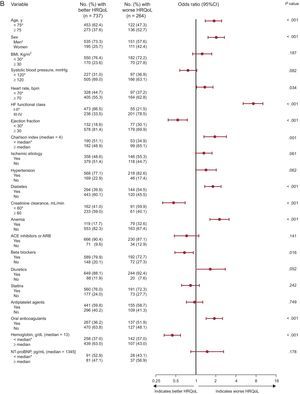
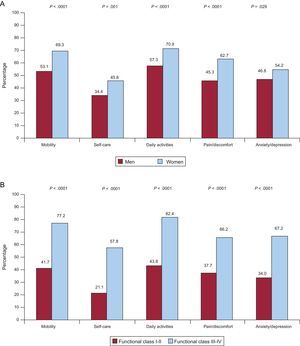
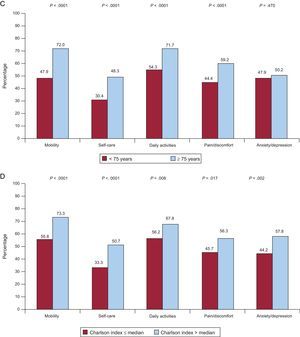
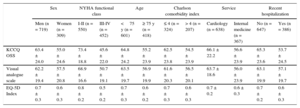
Figure 2 and Table 4 show the clinical factors associated with worse HRQoL. The multiple linear regression analysis (Table 4) showed that advanced age, female sex, worse functional class, and greater comorbidity were independent predictors of worse quality of life. The treatment of patients in cardiology services was independently associated with better quality of life, which is probably associated with a better clinical profile. These clinical features had an effect on the statistical significance of the differences in the raw summary scores of the instruments (Table 5) and the percentage of problems identified in each dimension of the EQ-5D (Figure 3).
Demographic and clinical factors associated with the health-related quality of life perceived by patients assessed using the Kansas City Cardiomyopathy Questionnaire (A), the EuroQoL-5 dimensions (B), and the EuroQoL-5D visual analogue scale (C). Quality of life related to poor health: overall Kansas City Cardiomyopathy Questionnaire summary score < 50; EuroQoL-5D index < 0.5; visual analogue scale < 50. Analyses were performed using univariable binary logistic regression models. 95%CI, 95% confidence interval; ACE, angiotensin converting enzyme; ARB, angiotensin receptor blockers; BMI: body mass index; HF, heart failure; HRQoL: health-related quality of life; NT-proBNP: N-terminal pro-brain natriuretic peptide. *Reference category.
Univariable and Multivariable Linear Regression Models used to Assess Demographic and Clinical Factors Associated with the Health-related Quality of Life as Measured by the Kansas City Cardiomyopathy Questionnaire Summary Score, the EuroQoL-5 Dimensions Overall Index, and the Visual Analogue Scale
| Univariable | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| KCCQ OSS | EQ-5D Index | VAS | |||||||
| β* | R2 | P | β* | R2 | P | β* | R2 | P | |
| Age, 1 y | –0.275 | 0.076 | <.001 | –0.287 | 0.082 | <.001 | –0.223 | 0.050 | <.001 |
| Sex, male/female | –0.157 | 0.025 | <.001 | –0.169 | 0.029 | <.001 | –0.108 | 0.012 | .001 |
| BMI, 1 | –0.056 | 0.003 | .077 | –0.082 | 0.007 | .010 | –0.016 | <0.001 | .610 |
| Systolic blood pressure, 1 mmHg | –0.010 | <0.001 | .743 | 0.001 | <0.001 | .965 | 0.041 | 0.002 | .194 |
| Heart rate, 1 bpm | –0.103 | 0.011 | .001 | –0.093 | 0.009 | .003 | –0.059 | 0.004 | .059 |
| NYHA functional class I-II/III-IV | –0.562 | 0.316 | <.001 | –0.465 | 0.216 | <.001 | –0.453 | 0.206 | <.001 |
| LVEF, 1% | 0.156 | 0.024 | <.001 | 0.129 | 0.017 | <.001 | 0.165 | 0.027 | <.001 |
| Charlson index, 1 point | –0.285 | 0.081 | <.001 | –0.318 | 0.101 | <.001 | –0.240 | 0.058 | <.001 |
| Ischemic etiology, no/yes | –0.068 | 0.005 | .030 | –0.086 | 0.007 | .006 | –0.050 | 0.003 | .114 |
| EGFR, 1 mL/min/ 1.73 m2 | 0.193 | 0.037 | <.001 | 0.187 | 0.035 | <.001 | 0.173 | 0.030 | <.001 |
| Hypertension, no/yes | –0.097 | 0.010 | .002 | –0.126 | 0.016 | <.001 | –0.040 | 0.002 | .202 |
| Atrial fibrillation, no/yes | –0.152 | 0.023 | <.001 | –0.172 | 0.030 | <.001 | –0.145 | 0.021 | <.001 |
| DM, no/yes | –0.149 | 0.022 | <.001 | –0.164 | 0.027 | <.001 | –0.106 | 0.011 | .001 |
| Hemoglobin, 1 g/dL | 0.227 | 0.051 | <.001 | 0.245 | 0.060 | <.001 | 0.214 | 0.046 | <.001 |
| Optimal treatment, no/yes | 0.028 | 0.001 | .366 | 0.042 | 0.002 | .188 | 0.038 | 0.001 | .230 |
| Inclusion service, CAR/IM | –0.186 | 0.035 | <.001 | –0.197 | 0.039 | <.001 | –0.185 | 0.034 | <.001 |
| Recent admission, yes/no | 0.259 | 0.067 | <.001 | 0.201 | 0.041 | <.001 | 0.195 | 0.038 | <.001 |
| Time since diagnosis <1 y, no/yes | –0.070 | 0.005 | .034 | –0.067 | 0.004 | .046 | –0.072 | 0.005 | .029 |
| Multivariable (stepwise backward method) | ||||||
|---|---|---|---|---|---|---|
| KCCQ OSS | EQ-5D index | VAS | ||||
| β* | P | β* | P | β* | P | |
| Age, 1 y | –0.230 | .030 | –0.004 | .002 | –0.178 | .072 |
| Sex, male/female | –10.258 | <.001 | –0.105 | <.001 | –3.683 | .095 |
| BMI, 1 | ||||||
| Systolic blood pressure, 1 mmHg | ||||||
| Heart rate, 1 bpm | ||||||
| NYHA functional class I-II/III-IV | –20.373 | <.001 | –0.180 | <.001 | –12.586 | <.001 |
| LVEF, 1% | 0.254 | .135 | 0.263 | .086 | ||
| Charlson index, 1 point | –1.258 | .005 | –0.008 | .136 | –1.029 | .009 |
| Ischemic etiology, no/yes | –0.053 | .055 | ||||
| EGFR, 1 mL/min/ 1.73 m2 | ||||||
| Hypertension, no/yes | –0.060 | .085 | ||||
| Atrial fibrillation, no/yes | ||||||
| DM, no/yes | –0.041 | .140 | ||||
| Hemoglobin, 1 g/dL | 1.023 | 0.087 | ||||
| Optimal treatment, no/yes | ||||||
| Inclusion service, CAR/IM | –4.595 | .049 | –0.035 | .185 | –4.761 | .022 |
| Recent admission, yes/no | 6.286 | .006 | 0.046 | .075 | ||
| Time since diagnosis <1 y, no/yes | ||||||
| R2 adjusted for each model | 0.3690 | 0.3151 | 0.2534 | |||
β, standardized beta coefficient; BMI, body mass index; CAR/IM, cardiology/internal medicine; DM, diabetes mellitus; EGFR, estimated glomerular filtration rate; EQ-5D, EuroQoL-5D overall quality of life questionnaire; KCCQ OSS, Kansas City Cardiomyopathy Questionnaire overall summary score; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
Unadjusted Analysis of the Mean Scores of the Overall Kansas City Cardiomyopathy Questionnaire Summary Score, Visual Analogue Scale, and the Overall EuroQol-5D Index Quality of Life Questionnaire in the Patient Subgroups With an Independent Association With The Kansas City Cardiomyopathy Questionnaire Summary Score in the Multivariable Linear Regression Analysis
| Sex | NYHA functional class | Age | Charlson comorbidity index | Service | Recent hospitalization | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men (n = 719) | Women (n = 309) | I-II (n = 550) | III-IV (n = 452) | <75 y (n = 601) | ≥ 75 y (n = 418) | ≤ 4 (n = 324) | > 4 (n = 207) | Cardiology (n = 638) | Internal medicine (n = 367) | No (n = 647) | Yes (n = 386) | |
| KCCQ OSS | 63.4 ± 24.0 | 55.0 ± 24.6 | 73.4 ± 18.8 | 45.6 ± 22.0 | 64.8 ± 24.2 | 55.2 ± 23.9 | 62.5 ± 23.8 | 54.5 ± 23.9 | 66.1 ± 22.2 | 56.6 ± 23.9 | 65.3 ± 23.6 | 53.7 ± 24.5 |
| Visual analogue scale | 62.2 ± 19.4 | 57.5 ± 20.8 | 68.9 ± 16.6 | 50.7 ± 19.1 | 63.5 ± 19.7 | 56.9 ± 19.9 | 61.6 ± 20.3 | 56.5 ± 20.1 | 63.7 ± 18.6 | 56.0 ± 23.9 | 63.1 ± 19.9 | 57.1 ± 19.7 |
| EQ-5D Index | 0.7 ± 0.3 | 0.6 ± 0.3 | 0.8 ± 0.2 | 0.5 ± 0.2 | 0.7 ± 0.3 | 0.6 ± 0.2 | 0.7 ± 0.3 | 0.6 ± 0.3 | 0.7 ± 0.2 | 0.6 ± 0.3 | 0.7 ± 0.2 | 0.6 ± 0.3 |
EQ-5D, EuroQoL-5D overall quality of life questionnaire; KCCQ, Kansas City Cardiomyopathy Questionnaire; NYHA, New York Heart Association functional class.
All differences between groups: P < .05.
Mean ± standard deviation according to sex (male vs female), NYHA functional class (I-II vs IV-III), age (< 75 years vs ≥ 75 years), Charlson comorbidity index (≤ 4 [median] vs > 4), time since last admission (< 30 days vs ≥ 30 days), and clinical service (cardiology vs internal medicine).
Unadjusted analysis of each dimension of the EuroQol-5D in patient subgroups with an independent association with health-related quality of life in the multivariable analysis. Percentage of patients who had some type of limitation in each of the 5 dimensions of EuroQol-5 dimensions according to sex (A); New York Heart Association functional class (B); age (C); Charlson comorbidity index (D); recent hospitalization (E), and clinical service (F).
This multicenter Spanish study showed that patients with HF and systolic dysfunction experience marked changes in HRQoL. Specifically, in patients with HF and advanced functional class, the level of HRQoL is similar to or even worse than that seen in patients with chronic obstructive pulmonary disease, pulmonary hypertension, Alzheimer's disease, or a history of stroke or in patients on dialysis.14–20 The average overall KCCQ summary score, particularly that of the subgroup of patients in NYHA functional class III-IV, was lower than that described in patients in international clinical trials on CHF.9,21,22 This finding highlights not only the worse HRQoL of patients with HF in the real world, but also the differences between populations included in trials and those treated in clinical practice.23
This study found high correlations between specific and generic HRQoL measures. Higher correlations were found between the overall scores of quality of life measured with the KCCQ and the dimensions or items that measured physical limitation imposed by the disease. These results suggest that physical limitations and symptoms related to HF (physical component) determine the decreased HRQoL of these patients.8,24–26 Notably, although high correlations were found between the items related to physical limitations or symptoms on the KCCQ and the generic overall measures of the EQ-5D, they were slightly lower than those associated with the overall scores on the KCCQ for HF. This result suggests that the HRQoL of patients with HF could also be affected by other factors beyond the physical limitations imposed by the disease and other aspects unaddressed by specific instruments for HF. These aspects include impaired ability to maintain self-care, pain, anxiety or mood symptoms, all of which are equally relevant in the perceived state of health of patients with HF.6,8,9,24 This aspect highlights the relevance of assessing HRQoL in these patients using specific and generic instruments and underlines the multidimensional character of HRQoL.8
A prominent aspect of our study was to assess the clinical determinants of HRQoL in these patients. Thus, we draw attention to the originality of this study, given the current lack of Spanish multicenter studies that have assessed the factors that determine HRQoL in such a large number of patients with systolic HF. The factors associated with worse disease progression, such as advanced age, comorbidity, recent hospitalization, or poor functional class, were independently associated with poor HRQoL. Many of these factors are not only associated with poor HRQOL,5,6,24–26 but are also associated with an increased risk of death or hospitalization.23 In this sense, previous studies have shown that HRQoL is an independent predictor of these clinical events.27,28
The association between sex and HRQoL found in this study may be related to the loss of the social role of women due to the limitations imposed by HF or to the possibility that the instruments that are designed to measure HRQoL better capture this information in women. Although the analyzes were adjusted for variables of severity of HF, patients attending cardiology services had better HRQoL scores, which were probably due to their clinical profile being better than that of patients attending internal medicine services. It is also likely that these differences may have been due to factors not collected prospectively and which better define patients regarding social aspects or frailty.
No independent association was found between HRQoL and several variables commonly used to stratify patient risk factors (such as left ventricular ejection fraction, renal function, or hemoglobin function). This result highlights the importance of incorporating HRQoL as an additional measure when assessing patients with HF, because other clinical variables used to stratify risk do not provide the information obtained from instruments that measure the patients’ perception of health, nor do they provide information on limitations, which differs from those obtained using physiological or biological measures.8
Finally, the impact of HF on HRQoL should be assessed in specific geographic areas. The European Commission has drawn attention to the differences between European countries in perceived health status and the importance of conducting studies on these specific aspects in each geographical area. This study is of relevance, because it provides novel data on HRQoL in Spanish patients with HF and adds new data on the determinants of HRQoL that complement published material on patients from other cultural or geographical environments.29
LimitationsThis study has the limitations inherent to all cross-sectional studies because it does not provide information on longitudinal changes of the study variable or on its association with the clinical determinants under investigation. The study population represented a subgroup of patients with HF and systolic dysfunction who are typically assessed in Spanish outpatient clinics. It is therefore not possible to determine if the results can be extrapolated to other populations of patients with HF, such as those with preserved left ventricular ejection fraction or who do not attend follow-up at outpatient clinics. This study addressed clinical variables and thus does not provide specific information on the impact of psychosocial variables or lifestyle and dietary habits on HRQoL.
CONCLUSIONSThis Spanish multicenter study found that patients with CHF have worse HRQoL than the general population and other patients with chronic diseases. High correlations were found between specific and generic measures of HRQoL. Several clinical factors, such as advanced age, female sex, advanced functional class, recent hospitalization, and greater comorbidity were associated with HRQoL independently of other prognostic factors. Patient treatment in Spanish cardiology services is independently associated with better quality of life, which is probably due to their better clinical profile.
FUNDINGPfizer S.L.U. promoted and funded the VIDA-IC study.
CONFLICTS OF INTERESTJ. Comín-Colet, M. Anguita, F. Formiga, L. Almenar, M.G. Crespo-Leiro, and L. Manzano received honoraria as members of the VIDA-IC assessment committee. J. Muñiz received honoraria for his collaboration in the independent statistical analysis. J. Chaves and T. de Frutos are employees of the Medical Department of Pfizer S.L.U. and collaborated in the VIDA-IC study.
We would like to thank all the researchers and patients who collaborated in the VIDA-IC study.
The study was acknowledged and supported by the Heart Failure and Transplantation Section of the Spanish Society of Cardiology and the Heart Failure Section of the Spanish Society of Internal Medicine.
Fieldwork was conducted by SANED. Statistical analyses were performed with the collaboration of ODDS S.L.