To the Editor:
Ductus arteriosus aneurysm is a rare but potentially fatal complication described in both children and adults.1-5
A 1-day-old neonate was referred to our unit for assessment due to dilatation of the right chambers observed during the last obstetric visit. The patient was asymptomatic and physical examination was unremarkable.
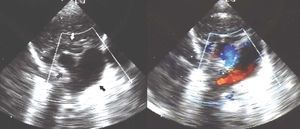
Echocardiography revealed a slight dilation of the right chambers and an aneurysm was visible in the long-axis suprasternal notch view when the transducer was inclined left word. The aneurysm measured 17 13 mm and was located next to the left pulmonary branch, into which some blood flow was visible from the upper limit of the aneurysm (Figure 1). Suprasternal cross-sectional echocardiography revealed filling of the aneurysm with blood from the aorta, with the classical rabbit ear sign (Figure 2). Those findings led to a diagnosis of ductal aneurysm. Complete regression of the aneurysm was apparent at 72 hours and the patient was discharged. Follow-up assessments revealed only a minimal ductal depression in the descending aorta.
Figure 1. Long-axis suprasternal echocardiogram with leftward inclination of the transducer. The aneurysm is indicated by a black arrow, the pulmonary artery and its branches by a white arrow, and blood flow from the aneurysm to the left pulmonary branch by a gray arrow.
Figure 2. Short-axis suprasternal echocardiogram. The aneurysm is indicated by a black arrow, the aortic arch and descending aorta by a gray arrow, and the innominate vein by a white arrow.
Ductal aneurysm can arise spontaneously, even during the fetal period. There are various theories regarding its pathogenesis: incomplete closure with formation of an aortic diverticulum that would then grow, localized mucoid degeneration of the ductal wall that would lead to weakening and subsequent formation of the aneurysm, fetal ductal constriction (a mechanism that could explain the dilation of the right chambers observed here), increased fetal ductal flow, reduction of ductal elastin and substitution with fibrous tissue, connective tissue diseases,1,3,4 etc. It can also occur as a complication of surgical or device closure of the ductus or due to ductal infection.1,2,6
It has generally been an infrequent finding. Lund et al1 reported 144 cases in the literature, with a high rate of complications (31% in infants aged less than 2 months, 66% between 2 months and 15 years, and 47% in adults, with worse rates in cases occurring due to surgery). The most frequently observed complication is rupture of the aneurysm, followed by thromboembolism, bronchial or esophageal erosion, and infection.1,4,7,8
Due to the risk of significant complications, surgical repair of the aneurysm has commonly been recommended if it does not regress early.1,2,7,8
Recently, various extensive neonatal series have been reported describing frequencies between 0.8% and 8% in newborn infants, with a common tendency toward spontaneous regression of the aneurysms during the neonatal period (as in the case presented here), via thrombosis and organization or by progressive reduction in size.3-5 The authors of those studies support a more conservative proposal, recommending resection if the aneurysm persists beyond the neonatal period, if it is associated with connective tissue disease, if there is a thrombus that extends to other vessels, if there is thromboembolism, or if the aneurysm compromises neighboring structures.3-5
In our opinion, given the possible complications and their potential severity, the patient must be closely monitored with the appropriate measures to allow immediate treatment of any complication until the likely regression of the aneurysm occurs.