In their celebrated editorial published in Revista Española de Cardiología in 2011, Danchin and Puymirat defined the period between 1980 and 2020 as “the three glorious decades of cardiology”.1 Their optimism was justified: while mortality from ischemic heart disease had continually increased in countries such as the United States until the end of the 1970s, becoming the leading cause of death,2 mortality from this cause markedly decreased in most Western countries, including Spain, between 1980 and 2010.1,2 However, from 2008 to the middle of the last decade, Spain underwent a major economic recession, whose consequences are still evident today in many aspects. In this context, an updated analysis of recent mortality trends was considered particularly pertinent.
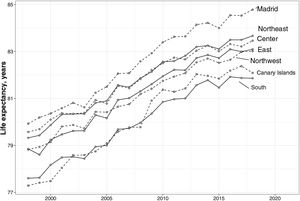
In an article recently published in Revista Española de Cardiología, Hervella et al.3 present an in-depth study of the changes in ischemic heart disease mortality in Spain between 1998 and 2018, using data from the Spanish National Institute of Statistics (INE). The authors should be congratulated for their robust, detailed, and flawless epidemiological analysis, which includes overall results and those stratified by age and sex groups and for each of the Spanish provinces, all appropriately adjusted by age. Taken together, the study shows that the positive trends in ischemic heart disease mortality also extend to the 2008 to 2018 period and mark a new “glorious decade” in Spain. The INE data on life expectancy during the same period confirm the good news (figure 1)4 and rule out the possibility that these trends were the consequence of marked increases in deaths from other causes. Spain has one of the longest life expectancies in the world and it continues to rise.5
Life expectancy by NUTS 1 region in Spain from 1998 to 2018. Provinces grouped into 7 regions using the NUTS 1 classification of Eurostat. Source: Spanish National Institute of Statistics.4 Eurostat, European Statistical Office; INE, National Institute of Statistics; NUTS, nomenclature of territorial units for statistics.
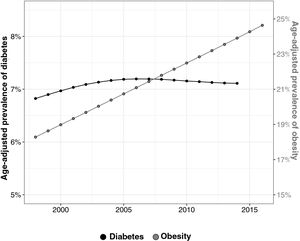
The data reported by the authors are particularly striking if we consider that various factors coexisted during the study period with potentially negative impacts on cardiovascular health. The aforementioned economic recession led to major cuts in health care and research in Spain, with direct effects on waiting lists, emergency department saturation, patients’ perception of care quality, and scientific innovation.6,7 In parallel, the age-adjusted prevalence of obesity highly significantly increased, as well as that of diabetes, until the mid-2000s (figure 2).8,9 This inconsistency between the increase in certain metabolic risk factors and the continual decrease in mortality together accentuate even further the “Mediterranean paradox” in Spain, whose causes are being clarified.10
Prevalence of diabetes and obesity in Spain from 1998 to 2016. Data from the Non-Communicable Disease Risk Factor Collaboration (NCD-RisC) project.8,9
Access to high-quality publicly funded health care might contribute to this paradox by increasing the number of risk factors being diagnosed while simultaneously ameliorating their effects through optimal treatment. However, the Hispanic/Latino population in the United States, who have much more limited access to health care, exhibit a similar paradox11: they have higher prevalence of risk factors such as obesity and diabetes vs the non-Hispanic/Latino population of European descent (with people of Mexican descent showing the highest age-adjusted prevalence of diabetes in the country, at 25%).12 In addition, Hispanic/Latino people in the United States frequently face adverse socioeconomic factors, particularly first-generation immigrants, who often lack health insurance.11 Despite everything, this group has much lower cardiovascular mortality than other groups, which contributes to a 3-year higher life expectancy than the population of European descent.13 This phenomenon cannot be entirely explained by the”salmon bias” (the return of migrants at death to their country of origin, which means that their deaths are not counted in the vital statistics of their host country)11; therefore, other possible protective factors include certain cultural aspects related to strong social and familial cohesion.14 In the coming years, studies such as the Hispanic Community Health Study/Study of Latinos (a 100% Hispanic/Latino cohort) and the Miami Heart Study (∼50%) will help to better explain the resilience of this group to cardiovascular death, with possible implications for the Mediterranean paradox, given the clear cultural similarities.
Until then, and returning to Spain, what are the possible causes of such durable success that can even resist an unprecedented economic recession? Previous studies have used the IMPACT model to assess the contribution of the control of certain risk factors and specific cardiovascular treatments to the lower coronary/cardiovascular mortality.1 Although this is not the case in the article by Hervella et al.,3 previous analyses in both Spain and other countries have consistently reported balances between improvements in prevention and treatment,1 which is why it is reasonable to expect a similar result in this case. More recent versions of the model, such as IMPACTSEC, permit a detailed examination of the potential population effects of these large-scale policies15; however, this model has not yet been applied to Spain.
The identification of the political, economic, social, and health care organizational factors that have contributed to these trends in ischemic heart disease mortality—the causes of the causes—may be useful for guiding health care policies that help to maintain these trends in the coming years. Thus, we feel compelled to speculate on some of the possible factors. In addition, and despite the intuitively expected mortality increase due to the economic recession, studies of this issue report the opposite, at least in the short-term: mortality tends to fall during modern economic recessions.16 These fluctuations according to economic situation are less evident in countries that invest in their social safety nets, whereas, in countries that reduce their social spending with austerity measures, economic growth without this protective net is associated with increased mortality compared with downturns, in which mortality falls in the short-term.16 Questions must be asked about the long-term effects of these processes, particularly in the case of Spain, where many of the austerity measures persist despite the economic growth observed from 2014 to the start of the COVID-19 pandemic.
Due to increased unemployment, the Spanish recession led to many families living together under the same roof. The broad social and familial support is part of the concept of familism described in Hispanics/Latinos, which is possibly cardioprotective,14 and the work by Fuster et al.17 has suggested that group support improves adherence and coronary risk factor control. Might this increased coresidence of family members have been a factor in the resilience to ischemic heart disease or at least its improved prognosis during the recession? Irrespective of this possibility, because the worst results were observed in the southern half of the country,3 which was particularly affected by unemployment and where the proportion of people per household is higher than the Spanish average,18 the benefits of this possible mechanism, if any, are slight.
Tobacco consumption further decreased during the study period, from 39% to 28% in men and from 25% to 19% in women between 2001 and 2017, according to Spanish Ministry of Health data.19 These figures, while positive, nonetheless indicate that there is still room for improvement. Antismoking laws, such as Law 42/2010, which concerns public health measures against smoking and regulates the sale, supply, consumption, and advertising of tobacco products,20 have not only helped to reduce the number of smokers, but also limited the exposure of nonsmokers to tobacco smoke. The effect of this passive exposure as a cardiovascular risk factor is well documented and the potential health benefits of this type of measure are enormous in this population group, a perfect example of the population strategy of prevention proposed by Geoffrey Rose.21
Finally, in the years evaluated by Hervella et al., major advances were made in Spain in multiple aspects of primary care, cardiovascular medicine, and other related medical specialties, from improvements in preventive treatments such as statins22 and antihypertensives to the full implementation of treatments such as primary angioplasty. Also noteworthy are actions to optimize diagnostic and treatment processes in cardiovascular patients, from the full development of chest pain units and Infarction Code Programs1 to, in a broader sense, improvements in the management of complex chronic patients, such as those with chronic ischemic heart disease or heart failure and the integration of hospital and regional care in certain areas.23 These and other quality improvements are particularly commendable in the context of cutbacks6 and highlight the resilience of medical staff in Spain, whose dedication and perseverance regarding the pursuit of excellence have resisted the effects of the recession.
Despite the positive tendencies reported by the authors and the justified resulting optimism, the presented data also indicate opportunities for improvement that should not be ignored. First, analysis of regional differences reveal a striking gradient that, although lower than in previous eras, indicates the need for additional effort in the southern half of Spain and in the Canary Islands.3 In our analysis of life expectancy by region (figure 1), major regional heterogeneity is also evident, which includes lower life expectancy in the southern region (Extremadura, Andalusia, Murcia, Ceuta, and Melilla) and the Canary Islands compared with Madrid, Castile and León, Castile-La Mancha, and the northeastern area (the Basque Country, Navarre, La Rioja, and Aragon). A detailed assessment of the regional differences in health care policies, risk factor prevalences, access to preventive measures, implantation of primary angioplasty networks, application of cardiovascular treatments, and chronic management models for patients might shed light on key factors explaining the good general outcomes, particularly in the northern half of the country, and accordingly guide national and local policies in the coming years.
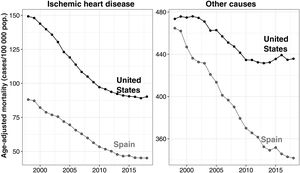
Second, in the temporal trend graphs for individuals younger than 74 years by Hervella et al., a striking slowing of the downward trend has been observed since 2010, particularly since 2015.3 In figure 3, these trends are analyzed by comparison of Spain and the United States and by exploring mortality from other causes.24 Although the attenuated fall in ischemic heart disease mortality has been similar in the 2 countries, this trend has been accompanied by a stabilization in mortality from other causes in the United States, and even an increase, a phenomenon not observed in Spain. This attenuation in the United States has been studied, and we believe that the same research would be valuable in Spain. An increasingly gradual decline is expected when the absolute figures are already low, and this is particularly evident in women younger than 74 years. However, the precise co-occurrence of this slowdown with the years of the economic recession and the aforementioned austerity during the years of subsequent economic recovery is a warning about their potential health consequences if this hardship is maintained over time.
Age-adjusted mortality for ischemic heart disease and other causes in Spain and the United States from 1998 to 2018. Data from the Institute for Health Metrics and Evaluation/Global Burden of Disease (IHME/GBD).24.
Finally, the study focuses on mortality,3 an indisputably relevant primary endpoint. Nonetheless, this leaves an important part of the epidemiological equation unanswered. What have been the trends, during the same period, in the incidence and prevalence of ischemic heart disease in Spain? In the United States, the incidence also significantly declined until 2013 but appears to have since stagnated.2 It would be expected that some of the mechanisms described would also result in a lower incidence; however, specific studies in our setting are necessary. Regarding prevalence, in a context of a) continuous population aging in Spain, and b) a strong association between age and incidence for most cardiovascular diseases, this decreased mortality, if not accompanied by marked improvements in incidence, may paradoxically increase the number of elderly patients with ischemic heart disease, often with heart failure, and other comorbidities requiring considerable investment in resources to ensure care in accordance with the quality expectations of the system.
In this context of the potential overload of the health care system with patients with chronic diseases, it should be noted that one of the groups most adversely affected in recent years by the Spanish economic situation and austerity policies have been health care professionals themselves. Those working in cardiology, intensive care, primary care, emergency services and medical emergencies, cardiac surgery, and other related specialties, who have achieved these extraordinary results through considerable professional and personal effort, have experienced a highly significant deterioration in their job stability during the last decade, as well as a significant decrease in their purchasing power. Working conditions in primary care are particularly difficult and have led to several strikes, and data indicate a rapid increase in burnout syndrome among all health care workers. Working conditions in public health and cardiovascular epidemiological research are also precarious.
Thus, as we celebrate these mortality results, we encourage the political leaders of Spain to realistically reflect on and never forget the extraordinary human sacrifice that has been required to achieve them. In our opinion, given the marked population aging, plans must be made to support future successes involving the sustainable use of resources, placing greater emphasis on population actions in public health that help to control the incidence of disease. A lower number of people with these diseases and, thus, lower spending on their care would permit, together with other necessary initiatives, improved working conditions for workers that reflect their long years of training, effort, and high level of responsibility.
In any environment that aspires to motivate its workers and maintain good long-term results, the data presented by Hervella et al. can only lead to positive reinforcement, not to penalties or additional cuts. Only through policies that prioritize primary and primordial prevention can we help to balance the complex economic-health care equation. This would result in greater sustainability of the system, with cardiovascular patients continuing to receive excellent care and the country's health care and public health professionals enjoying their profession in nonprecarious conditions and, decade after decade, continuing to achieve results that-in full agreement with Danchin and Puymirat-can only be described as glorious.
FUNDINGNone.
CONFLICTS OF INTERESTThe authors declare that they have no relationship with industry that is relevant for the content of this manuscript.