Keywords
INTRODUCTION
Different studies over the last few years have shown that intracoronary infusion of mononuclear bone marrow cells (MBMC) in patients with acute myocardial infarction improves ventricular function,1-12 to variable degrees. Although the mechanism is still unknown, there are transdifferentiation and nesting hypotheses of a response to a supposed paracrine effect of the infused cells themselves. In many clinical studies favourable ventricular remodelling and an improvement of the ejection fraction have been seen, althaugh the factors that affect the degree of functional recovery are not well known. There is data that suggests that this is greater when a larger number of cells are infused8,11,12 during the first 7 days post-infarction or greater if this is done after day 611; the beneficial effect is more detectable in extensive infarctions.6,8
In chronic infarction, the scenario is completely different. In general, adverse remodelling has already taken place, and, if extensive, cardiac failure is almost inevitable. Although disease evolution in this type of patient depends on medical treatment and a possible revascularization, the long term prognosis is complicated.
Cell therapy may play a beneficial role in this type of patient, even if, at the moment, there are no known chemotactic factors that favour nesting.13 Different clinical studies, using different strategies and routes of administration, and also different types of cells, have shown a favourable effect,14-20 although more information is required. With respect to intracoronary infusion with autologous MBMCs, there is little information in patients with chronic myocardial infarction that suffer severe ventricular function depression and heart failure.17,18
This clinical trial analyses the evolution of 19 patients with chronic extensive anterior infarction and heart failure treated with intracoronary infusion of MBMCs.
METHODS
Patient Screening and Study Protocol
From June 2005 to January 2008, 19 patients were consecutively screened for this study that complied with the following inclusion criteria: a) anterior chronic myocardial infarction (more than 1 month since the acute episode), with stable sinus rhythm; b) revascularization of the left anterior descending artery (LAD) or other ischemic territories, if these exist; c) depressed ventricular function (ejection fraction [EF<40%]) after an old infarction; d) symptoms of heart failure, in spite of receiving optimum medical treatment; and e) acceptance of the study protocol. The exclusion criteria were: a) over 80 years of age; b) concomitant haematological disease or cancer; c) pregnancy; d) participation in another study; and e) poor life expectancy. The aforementioned protocol had been accepted by the clinical trials committee of our hospital and the corresponding regional body. All patients were initially studied both clinically and echocardiographically during study pre-screening. At that time, they were ensured optimum medical treatment for their heart failure. After pre-screening, all the patients underwent leftheart catheterization to study ventricular function and determine that complete revascularisation had been achieved. After providing a signed an informed consent, all patients were programmed for cell therapy.
Autologous bone marrow cells were obtained without prior stimulation and were not cultured. Under local anaesthesia, repeated punctures and aspirations over an iliac crest were performed until reaching a total volume of between 100 and 150 mL of bone marrow. Mononuclear cells were isolated by Ficoll-Hypaque density gradient centrifugation (density 1077) in a COBE 2991 semiautomatic cell processor. After undergoing three washes, the MBMCs were filtered and re-suspended in 10 mL NaCl at 0.9% with heparin 0.1% and infused into the patient by the intracoronary route, not later than 3 hours after puncture.
To carry out intracoronary infusion, the LAD was temporarily occluded to create a stagnant distal flow that would favour diffusion of the cell suspension into the capillary tree. After infusion, patients were sent to the ward, where they were monitored electrocardiographically so as to detect any changes or arrhythmias after cell infusion. Serial determinations of serum enzymes over 24 hours were also performed. Finally, patients were discharged under medical treatment and closely followed-up by means of frequent telephone calls. At 6 months, patients were admitted for a clinical study identical to that performed at baseline and a subsequent haemodynamic study on follow-up, with a repetition of functional studies using the same methods. After a year of follow-up, the clinical and echocardiographic studies were repeated in ambulatory conditions. Surviving patients continued under clinical follow-up indefinitely.
Functional Studies
Echocardiographic Ventricular Function Studies
In all cases, a complete echocardiographic study was performed with digital acquisition of two-dimensional images of the left ventricle of, at least, 3 cardiac cycles in 4 and 2 chamber apical projections and also parasternal projections at a baseline, mid and apical level. In all cases the sector explored and field depth were optimized to obtain a frequency of, at least, 60 images per second. The images were sent to a work station for their subsequent analysis. Ventricular volume and ejection fraction were measured by 2 expert echocardiographers, who were unaware of the study conditions, using the Biplane Simpson method. In patients with poor echographic windows, echo-enhancers were used to achieve appropriate views of the endocardial border.
Angiographic Ventricular Function Studies
For each study condition a complete left sided haemodynamic study was performed to register systemic arterial blood pressure and enddiastolic blood pressure and, at least, one left ventriculography at 30º right anterior-oblique projection. During each study ventriculogram an attempt was made to obtain a sinus beat and a post-extrasystolic beat for analysis, with the aim of studying the contractile reserve of the left ventricle. Post-extrasystolic beats were obtained by inducing premature beats with the catheter itself, once a sinus heart cycle with good opacity had been obtained. In all cases, the R-R' interval of the induced premature beat and the R-R' of the post extra-systolic pause were registered and measured.
We performed all the calculations and measurements of ventricular function in our own laboratory. Two expert angiographers, who were unaware of the study conditions, drew the enddiastolic and endsystolic silhouettes using the CASS system. Volumes and EF were determined and regional motility analysed. Sheehan's method21 was used to study asynergy, dividing the superimposed silhouettes by 100 radii of systolic wall shortening, from enddiastole to endsystole. The abnormal contracting segment (ACS) was defined as the percentage of radii that showed akinesia or dyskinesia. The areas of the anterior wall affected by the old infarction included the ACS and the hypokinetic chords surrounding such segment. Therefore, the functional behaviour of the infarcted myocardium after treatment was observed in a series under identical conditions, favouring evaluation of any possible recovery. Series evaluation of contractile reserve was assessed by means of post-extrasystolic enhancement analysis.
Flow Velocity and Coronary Flow Reserve
The FloMap® (Cardiometrics, Mountain View, California) system was used. Baseline studies of coronary flow reserve (CFR) on the LAD were always carried out before the intracoronary infusion of cells and at 6 months of follow-up. A 0.014" Doppler guidewire was introduced and the tip was placed distal to the treated segment of the LAD, registering flow velocity in a continuous manner. The mean velocity peak was obtained at baseline and after the administration of an intracoronary bolus of 60 μg of adenosine. CFR was calculated as the ratio between maximum flow velocity during adenosine peak effect and baseline flow velocity.
Biological Study
Aliquot amounts of the infused MBMCs suspension were taken to determine cell immunophenotype by means of three-colour flow cytometry. The cells were marked with monoclonal antibodies bound to phycoerythrin-cyanine-5 (PECy5) or peridine-chlorophyll-protein (Per-CP) in comparison with human CD34 (BD Biosciences, San José, CA, USA), and the following monoclonal antibodies marked with fluorescein isothiocyanate or phycoerythrin: CD38, CXCR4, CD31,CD146, CD45 (BD Pharmingen, San Diego, CA, USA), CD133 (Miltenyi Biotec, Auburn, CA, USA), CD90, VEGFR2 (R&D Systems, Minneapolis, USA), HLA-DR and CD117 (BD Biosciences) in a FACSCanto flow cytometer with a double laser using Cell-Quest software (Becton Dickinson, San José, CA, USA). At least 2000 events were analyzed for each marker.
For in vitro culture of endothelial stem cells, the cells were re-suspended in EBM-2 (Cambrex Bio Science, Walkersville, USA) medium with 20% foetal bovine serum at a concentration of 1´106 cells/mL and cultured on plates pre-treated with fibronectin (BD Biosciences Labware, Bedfor, USA) with a change of medium every 48 hours for 2 weeks, after which the colonies formed by the endothelial stem cells were quantified by counting under an inverted microscope.
The functional analysis of the chemotactic capacity of the infused cells was carried out in a modified Boyden chamber (BD Biosciences Labware) in the following manner: the upper chamber of a Transwell 24 well plate with a 6.5 mm diameter Matrigel membrane with 8 μM pores was loaded with 5x104 MBMCs and the lower part of the chamber with EBM-2 + Stromal-derived-growth-factor-1 (SDF-1, 100 ng/mL, R&D Systems), or with EBM-2 + Vascular Endothelial Growth Factor (VEGF, 100 ng/mL, R&D Systems) or medium only. The plates were incubated at 37ºC, with 95% humidity and 5% CO2 for 24 hours, after which, and after observation under an inverted microscope with an automatic field counting system, the percentage of migrated cells was calculated.
Statistical Study
Data are expressed as mean (standard deviation). To compare mean values non-parametric tests were used (Wilcoxon for paired data and Mann-Whitney for independent data). The differences between the 3 conditions of the echocardiographic study in the same patient were analysed using a non-parametric test for k related samples (Friedman test). Linear correlation between quantitative variables was analysed using the Pearson test, obtaining the r correlation index and its statistical significance. Values of P<.05 were considered statistically significant.
RESULTS
Clinical Evolution
The 19 patients screened had an average age of 56 (8) years; 17 are men and 2 women. The mean time from infarction up to the time of the study was 27 (45) months. Two of them had automatic defibrillators implanted since they had suffered lethal arrhythmias, 16 of them had undergone revascularisation during the acute phase or later; on the other hand 3 patients had not had any haemodynamic studies prior to infarction and were revascularised, with implantation of drug eluting stents, before inclusion in the study. Currently the average follow-up time is 21 (11) months.
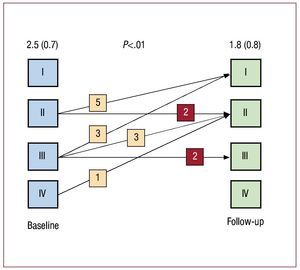
All patients showed good evolution after the intracoronary infusion of MBMCs. None of the patients presented any arrhythmias worthy of mention during the following 24 hours or any significant elevation of blood enzymes (average CPK peak was 125 [39] IU). All patients were discharged under medical treatment and closely followed-up. Six patients required re-hospitalization due to heart failure and 3 due to angina. Two patients suffered re-stenosis and another patient suffered coronary disease progression, all required repeat revascularization. Three patients died during follow-up (6, 9, and 11 months later) due to myocardial infarction, heart failure and stroke, respectively. Evolution of the functional grade in the survivors can be seen in Figure 1. It is possible to determine that, in general, there was an improvement in functional grade, with no detectable changes seen in 4 patients. The stress test with oxygen consumption at 6 months did not show significant changes, however neither was deterioration observed (23 [8] vs 24 [8] mL/Kg/ min; ns).
Figure 1. Functional grade evolution. In general, an improvement of functional grade was seen, with no detectable changes in 4 patients.
Biological Study
Patients received an average of 10.02 (0.9) x108 MBMCs. The number of infused cells that expressed each of the studied phenotypes was detected by flow cytometry, as also their functional characteristics in relation to migration and formation of endothelial colonies, as is detailed in Table 1.
Functional Evolution
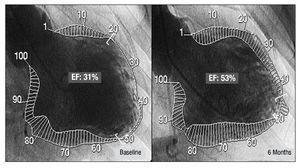
Table 2 shows the changes observed in ventricular volumes in the whole group of patients with angiographic follow-up at 6 months and echocardiographic follow-up at 1 year after cell therapy. The ejection fraction measured angiographically showed an average net gain of 5% that was somewhat greater (10%) when assessed echocardiographically. There were no significant changes in angiographic ventricular volumes, thus, no worsening of ventricular remodelling was seen at 6 months. Analysing regional function of the sinus beat, a significant decrease in the number of hypokinetic or akinetic chords was seen in the ventriculogram. Therefore, functional improvement is based on a certain recovery of the peri-infarction areas of the anterior wall (Figure 2). Indeed, no direct correlation was seen between ejection fraction gain and chord gain (r=0.57; P<.02). However, a significant changes were seen in the ACS. LAD coronary flow reserve remained within normal values and was similar to baseline values. With reference to post-extrasystolic beats, neither were there any significant changes in ventricular volumes, or ejection fraction, or ACS. However, there was significant decrease in the number of hypokinetic or akinetic chords in the anterior peri-infarction area. No significant changes were observed in extra-systolic enhancement, which seemed to have remained at the same level at the end of 6 months.
Figure 2. Functional ventriculographic changes in one patient who was a clear responder to the cell infusion.
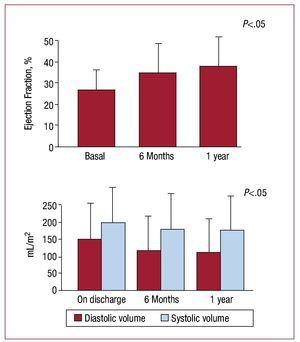
Analyzing serial changes in ventricular function by echocardiographic methods, a significant decrease in ventricular volume is seen at 1 year together with an improvement in EF (Figure 3).
Figure 3. Changes in volumes and ejection fraction seen on ultrasound.
Analyzing angiographic functional changes individually, 2 kinds of response to cell therapy were seen: on the one hand, the apparent "nonresponders" with net changes of their ejection fraction <3% or even with deterioration (Group I; n=9); on the other hand, those that had a gain greater than 3% (Group II; n=8) and that, therefore, could be considered "responders" to the hypothetical effects of current cell therapy. The 3% cut-off point was adjusted by a good distribution of the 2 groups of patients and because it was the mean change in the study control group TOPCARE-AMI.2 No significant changes were seen either in ventricular volume or in ejection fraction in Group I patients. However, they did present greater ventricular volume and more adverse remodelling at baseline. Significant changes in global and regional function were seen in Group II patients, with an average net gain of 10% (range, 6-22) in ejection fraction (Table 3).
Factors Related to Recovery
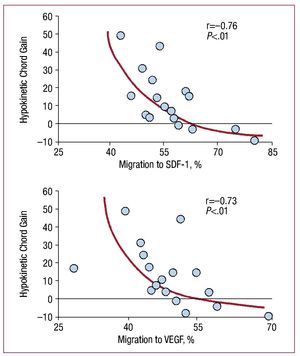
Table 3 also shows the parameters analysed in the univariate analysis. The total number of infused cells did not seem to make any difference in this study: although this number was quite homogeneous, and was greater than 10´108 in 79% of the patients. The time from revascularisation to implantation does seem to make a difference, as also concomitant hypertension. On the other hand, Table 4 shows a linear correlation matrix between functional recovery parameters and parameters of the biological in vitro study. As can be seen in this Table, a persistent inverse relation was seen between functional gain parameters and biological parameters indicating a tendency to migration in the sample of infused cells. When we carried out a careful analysis of these relationships we saw that some are exponential for certain parameters (Figure 4). Furthermore, paradoxically, they suggest that when there is more specific migration of the cells to SDF-1 and to VEGF, there is less functional recovery. However, there was no relation between functional gain and CXCR4.
Figure 4. Exponential correlation between hypokinetic chords gain with migration, in percentages, to stromal derived factor 1 (SDF-1) and with migration to vascular endothelial growth factor (VEGF).
DISCUSSION
The patients screened for this clinical trial had as a common factor an old prior infarction and poor residual ventricular function, in spite of having undergone complete revascularization. They were receiving optimum medical treatment to combat ventricular remodelling, although they had some symptoms of heart failure. Therefore, this was a homogeneous group of high risk and difficult to treat patients. In any case, the risk of mortality in these patients is high, whether due to arrhythmias or heart failure. Different studies carried out with patients in similar conditions have shown the efficacy of different forms and strategies of cell therapy (variations both in route of administration and in type of cell used). These studies showed clinical improvement and functional gain in patients with chronic infarction.14-20 Our findings also suggest that intracoronary infusion of MBMCs may produce a modest functional benefit, although some patients show a greater gain.
There are therefore responders and non-responders to the intracoronary infusion of MBMCs in terms of ventricular function. In certain patients there is clear functional improvement (Figure 2), whereas others do not show functional changes or even suffer a deterioration of their EF. The factors affecting response are not known, although according to our observations, neither age, nor time from infarction, CR, extra-systolic enhancement, or the number of cells infused, seem to be factors influencing response. However, time from revascularization to cell infusion could have some influence (Table 3). The time between revascularization and cell implant was shorter in responders. Although there was always an intervening period of months, a short period between both procedures seems to favour functional recovery. Indeed, we cannot rule out a late revascularization effect, especially in patients that underwent revascularization close to cell therapy. Similarly, hypertension was more frequent in non-responders.
In relation to the analyzed biological parameters, there is a persistent inverse relationship between functional parameters and those biological parameters that are related to a tendency to migration. It has been shown that the recruitment of bone marrow stem cells by the myocardium is determined by a positive SDF-1 gradient, driven, by a greater concentration of cytokines in the myocardium in relation to the coronary vascular tree, and in circulating blood in relation to bone marrow.22 This mechanism acts naturally in the pathophysiological conditions subsequent to acute infarction, but in chronic infarction, the gradient is reversed23 and the neovascularizing capacity of the MBMCs is markedly reduced.24 This impedes recruitment and consequent nesting of the stem cells in the myocardium suffering from chronic infarction. Intracoronary infusion of a large number of cells with the capacity to migrate to SDF-1 may be useful in an inverted SDF-1 gradient situation that impedes the chemotaxis that is indispensable for extravasation and cell nesting. Our results show that infusion of a higher percentage of cells with rapid migratory capacity (24 hour in vitro migration) to SDF-1 causes significantly less functional recovery. The explanation for this phenomenon could be found in the recent discovery that the bone marrow has at least two stem cell niches. One perivascular niche capable of rapid mobilization, and one osteoblastic niche, where quiescent cells reside, that is to say the true immature stem cells which, in response to SDF-1 only migrate after several days.23 It is possible that, if we think of a hypothetical paracrine effect of cell infusion,25 myocardial functional improvement is due to the action of these cells in a quiescent or non-differentiated state that are capable of contributing all kinds of growth factors to peri-infarction tissue. This surprising finding, however, requires confirmation by a greater number of studies, as also studies carried out in acute disease, in which the situation is completely different.
Study Limitations
This was a prospective study without a control group for purposes of comparison. Furthermore, the group of patients studied, although homogeneous, is small, therefore results must be interpreted very cautiously and require confirmation by larger series. On the other hand, the possible clinical improvement detected in our surviving patients could be due to a certain placebo effect, given the marked social interest in advances in cell therapy. However, this cannot be said of the changes in ventricular function.
CONCLUSIONS
Intracoronary infusion of MBMCs in patients with chronic anterior infarction and severe depression of ventricular function could generate a slight clinical and ventricular function improvement, this effect was more pronounced in a group of patients which we have called responders (Group II): Patients in this group had been revascularized during the last 7 months on average and did not suffer from hypertension. When correlation was established between functional gain parameters and the results from the in vitro biological study, an inverse relation was found between functional parameters and those biological parameters that are characteristic of a state inclined to migration. This paradoxical finding requires confirmation, but may have a significance we need to understand.
ABBREVIATIONS
ACS: abnormal contracting segment
CFR: coronary flow reserve
EF: ejection fraction
MBMC: mononuclear bone marrow cell
SDF: stromal-cell derived growth factor
VEGF: vascular endothelial growth factor
SEE ARTICLE ON PAGES 1117-9
Correspondence: Dr. J.M. Suárez de Lezo.
Servicio de Cardiología. Hospital Universitario Reina Sofía. Avda. Menéndez Pidal, s/n. 14004 Córdoba. Spain.
E-mail: grupocorpal@grupocorpal.com
Received July 28, 2009.
Accepted for publication January 26, 2010.