We aimed to describe the feasibility and preliminary outcomes of commissural alignment (CA) for the balloon-expandable transcatheter heart valve.
MethodsThe relationship among native commissures and transcatheter aortic valve implantation neocommissures was analyzed in 10 consecutive patients with tricuspid severe aortic stenosis undergoing transcatheter aortic valve implantation after guided implantation based on computed tomography analysis with a self-developed software. CA was predicted by in silico bio-modelling in the 10 patients and the calculated rotation was applied during crimping. Degrees of CA and coronary overlap (CO) were measured through 1-month follow up computed tomography. Transvalvular residual gradients and the rate of paravalvular leak were also analyzed.
ResultsMean commissural misalignment was 16.7±8°. Four patients showed mild misalignment but none of them showed a moderate or severe degree of misalignment. The in silico model accurately predicted the final in vivo position with a correlation coefficient of 0.983 (95%CI, 0.966-0.992), P <.001. Severe CO with right coronary ostium occurred in 3 patients likely due to ostial eccentricity, and CO was not present with the left coronary artery in any of the patients. Mean transaortic gradient was 6.1±3.3mmHg and there were no moderate-severe paravalvular leaks.
ConclusionsPatient-specific rotation during valve crimping based on preprocedural computed tomography is feasible with balloon-expandable devices and is associated with the absence of moderate or severe commissural misalignment and left main CO.
Keywords
In recent years, the indications for transcatheter aortic valve implantation (TAVI) have been expanded from patients who are ineligible or at high risk for surgical aortic valve replacement to patients who have a lower risk profile.1,2
Despite advances in technology and improvements in valve devices, several factors can affect the mid- to long-term durability of the prosthesis such as the degree of expansion, the geometry of the stent frame, calcifications, and left ventricular outflow tract protrusion.3,4 Another critical point is commissural alignment (CA) between native and prosthesis commissures. Recent research demonstrates that preprocedural planning is key to achieve CA, demonstrating feasibility, safety and advantages in reducing coronary artery overlap.5–7 CA feasibility and benefits are better defined for self-expandable devices.6,7 However, there is no evidence on the feasibility of CA with the novel balloon-expanding Myval (Meril Life Sciences Pvt. Ltd, India), and in general, the chances of achieving adequate CA with balloon-expandable devices are limited according to current evidence.6
METHODSThe relationship among native aortic commissures and transcatheter heart valve (THV) commissures was analyzed in 10 patients undergoing TAVI with the Myval device. All patients were included in the accurate CA project approved by the local ethics committee and provided informed consent. Computed tomography (CT) based models were analyzed leading to: a) in silico model for TAVI simulation preprocedurally; and b) in vivo determination of the degree of CA and coronary overlap. Pre- and postprocedural CT was available in all patients.
Computed tomography acquisitionCT scans were acquired in a 128-row detector scan with a 0.625mm slice thickness. Studies were contrast-enhanced, multiphasic and electrocardiographic gated. For the analysis, 70% of the cardiac cycle was selected.
MeasurementsThe orientation of THV commissural posts, native valve commissures and left coronary artery were measured in a perpendicular cross-section multiplanar reconstruction of the aortic root as the clock-faded deviation angle starting at the right coronary (0°), which was positioned at 12 o’clock, as previously described.7 Measurements were drawn considering an angle with the tip in the center of the aorta, which was considered also the center of the THV stent frame. This angle was determined from each commissural post of the prosthesis (where neocommissures are sutured) to the commissures of the native valve. Mean commissural misalignment (CMA) was calculated for each patient as the mean value of the 3 measurements performed per patient (1 per commissure). Thye final result was categorized according to previous consensus5 as: aligned (0-15°), mild CMA (15-30°), moderate CMA (30-45°), and severe CMA (45-60°). In addition, an angle equal or lower than 20° from the commissural post to the coronary ostia was defined as significant coronary overlap5 (figure 1 of the supplementary data).
In silico simulationSimulated biomodels of the final THV position were designed from CT acquisition and accurate CA orientation was prospectively estimated. The biomodel meshes and centerlines were exported to a computer assisted design software (Rhinoceros, MCneel and Associates, United States) where further analysis was made. The optimal rotation of the valve for achieving a commissural aligned implant was estimated using a self-developed script–as previously described for alternative self-expandable devices7–which allows a controlled rotation of the 3-dimensional virtual valve (video 1 of the supplementary data).
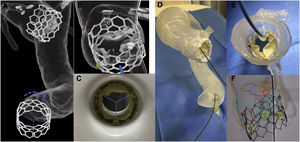
In vivo demonstrationMyval devices were crimped as the in silico model orientation predicted to avoid CMA as shown in figure 1. CT scans from 10 consecutive patients who received Myval were performed 1 to 3 months after the procedure to obtain a precise comparison with the simulated model and CA was studied.
A: in silico simulation of a Myval device implantation in patient-specific aortic biomodel illustrating the effect of a 60° rotation in the final implant position. B: detailed view of the aortic root with a commissural alignment implant of a Myval device, see how the neo-commissures (red asterisks) match the native commissures and how the left coronary ostium (yellow asterisk) is centered between the adjacent neo-commissures. C: valve crimping with the commissures oriented as previously calculated. D: in vitro accurate commissural alignment implant of a Myval device in a patient-specific 3-dimensional printed phantom. E: trimmed view of the previous 3-dimensional printed phantom (the aortic arch has been removed), a Judkins left catheter is engaging the left coronary artery, highlighting the absence of coronary overlap of the neo-commissures (red asterisks). F: valve implantation without significant commissural misalignment (commissural post marked by red asterisks and native commissures represented as green peaks).
Differences among in silico and in vivo results were calculated taking as reference the native commissure orientation in each case. The degree of agreement between the different measures was obtained, taking each of the measurements as independent, with Lin's concordance correlation coefficient. Statistical analysis was performed using R 3.6.3 (R Foundation for Statistical Computing, Austria).
RESULTSA patient-specific clockwise or counter-clockwise rotation was performed to match the commissural posts of the prosthesis with the native commissures in the aortic root biomodel. Then, the TAVI procedure was performed as standard of care, after crimping the valve into the delivery system, as previously described, to achieve the predicted angle (figure 1).
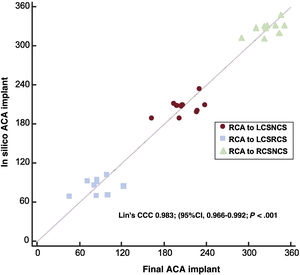
As shown in table 1, in silico simulation suggested correct alignment in all patients and in vivo procedures demonstrated correct alignment in 6 of the 10 patients and mild misalignment in the remaining 4 patients. There were no cases of moderate or severe CMA. The mean degree of misalignment was 16.7±8°. The concordance of the commissural post orientation in the in silico THV implants to the final commissural post orientation was high, with a Lin's concordance correlation coefficient of 0.983 (95% confidence interval [95%CI], 0.966-0.992), P <.001 (figure 2).
Degree of commissural misalignment in the in silico simulation and in vivo procedure.
Correlation of commissural post orientation among in silico and in vivo results according to post-TAVI computed tomography scan. 95%CI, 95% confidence interval; CCC, concordance correlation coefficient; LCSNCS, commissural post between left coronary sinus and noncoronary sinus; LCSRCS, commissural post between left coronary sinus and right coronary sinus; RCA, right coronary artery; RCSNCS, commissural post between right coronary sinus and noncoronary sinus.
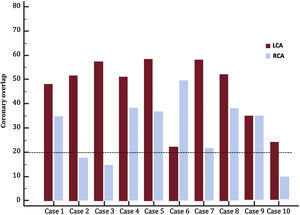
Regarding the degree of coronary overlap, patient-specific details are presented in figure 3. Out of 10 patients, 3 of them (patients 2, 3 and 10 in figure 3) showed significant overlap of the ostium of the right coronary artery and the commissural post. In contrast, none of the patients showed severe coronary overlap of the left coronary artery ostium. The main findings are summarized in figure 4.
Degrees from the commissural post of the prosthesis to the coronary ostia detailed by patient. An angle lower than 20° reflects a high risk of coronary overlap (post in front of the ostium) and also, lower efficacy of eventual BASILICA technique if required in the future before valve-in-valve procedure. Patients 2, 3 and 10 had significant overlap of the ostium of right coronary artery and the commissural post; none of the patients showed severe coronary overlap of the left coronary artery ostium. LCA, Left coronary artery; RCA, right coronary artery.
Central illustration. The strategy for rotation of the prosthesis and the expected results are reflected on the left side of the figure. On the right side, the main findings are summarized including: a) the degree of counter-clockwise (red) or clockwise rotation (blue) when crimping; b) the degree of commissural alignment of the prosthesis (green) with the native commissures (blue) and numerical range of degrees for patients with good commissural alignment (from 7° to 18°) and in those with mild commissural misalignment (from 22° to 30°); c) the degree of coronary overlap for both right (blue) and left (red) coronary ostia with the commissural posts of the prosthesis (cases with severe coronary overlap are pointed out with a pink asterisk).
The mean transaortic gradient was 6.1±3.3mmHg and there was no moderate-severe paravalvular leak.
DISCUSSIONCA is crucial for 2 reasons: a) commissural misalignment might be related to more difficult coronary reaccess if eventually needed and could be related to higher rates of central aortic regurgitation, greater residual gradients, and increased blood stagnation in the leaflets/sinuses of Valsalva, potentially linked to faster prosthesis degeneration5; b) coronary overlap occurring when coronary ostia are too close to the prosthesis commissural posts, is relevant if there is an eventual need for repeated valve intervention (TAVI-in-TAVI), since it is associated with a well-known and life-threatening risk of coronary obstruction; although it can be prevented by the BASILICA technique (bioprosthetic scallop intentional laceration to prevent iatrogenic coronary obstruction),6 if the coronary ostia are not in the center of the neo-sinuses but close to the commissural posts of the first prosthesis, the coronary ostia can be occluded even after leaflet laceration.
Several strategies have been developed for CA during self-expandable TAVI procedures but none of them have been demonstrated to be feasible for balloon-expandable devices. Indeed, prior techniques tried to achieve adequate alignment of balloon-expandable devices by orienting the delivery system during the deployment, which resulted in a highly unpredictable final position of the prosthesis when implanted due to difficult identification of neocommissures in the crimped devices. The proposed patient-specific technique in our research suggest that: a) CA of native and prosthetic valves can be achieved with no need to manipulate the delivery system within the patient but by CT-based planning, avoiding moderate and severe misalignment in all cases; b) coronary overlap with the commissural posts could be avoided in all patients for the left coronary artery and in 70% of patients for the right coronary artery, which still showed 3 cases of coronary overlap likely due to the greater eccentricity of the right coronary ostia in the native sinuses of Valsalva.
These findings might have important prognostic relevance in the long-term and are particularly relevant for low-risk patients undergoing TAVI. In addition, the findings for the Myval device are likely reproducible with the Sapien-3 device (Edwards Lifesciences, United States), although future research is needed to confirm these findings.
Commissural alignment and transcatheter heart valve prosthesis durabilityThere is no clear evidence yet of the association between CMA and transvalvular gradient or coronary filling; however, a significantly higher rate of mild central aortic regurgitation has been described in moderate or greater CMA, probably due to stent frame deformation.5 Residual aortic regurgitation is a factor that has been previously associated with earlier valve degeneration but, to date, no comparison of conventional implant vs CA planned TAVI has been performed. Of note, the degree of misalignment with Myval was greater than that previously reported for the Acurate neo device (Boston Scientific, United States) using the same software (7.7±3.9°),7 which might be due to variability in measurements but could also potentially be related to a less precise rotation of the valve when crimped than the rotation of the delivery system of self-expandable devices when CA is attempted. In crimped self-expandable valves, the neocommissures are always oriented in the same position within the delivery system; in contrast, maintaining an intentional orientation of balloon-expandable devices while crimped is not easy due to minor rotation within the crimper system.
Repeat valve intervention and coronary ostia re-accessLaceration of previously implanted valve leaflets (BASILICA technique) has been reported to reduce coronary occlusion risk in valve-in-valve procedures.8 However, the presence of misalignment of the commissures might reduce the efficacy of this complex technique. In addition, in recent years, there is a growing population that requires a coronary angiogram after a TAVI procedure. Differences among this procedure compared with conventional angiograms are described and practical guides for coronary access after TAVI are available.9 Balloon-expandable devices have a significantly better profile for future coronary engagement compared with self-expandable different iterations as described by Ochiai et al.10 in the RESOLVE study (up to 34.8% of difficult engagement with self-expandable devices vs 15.7% for left coronary artery and up to 25.8% vs 8.1% for right coronary artery). Our findings for the Myval device suggest that CA might reduce the risk of poor engagement of the left coronary artery almost completely and minimize it for the right coronary artery.
LimitationsThe main limitation of this study is the reduced sample size and the lack of a control group. All patients had mild or moderate tortuosity of the aorta and ilio-femoral axis; therefore, the potential impact of this factor on the predictability of the final prosthesis orientation remains unknown. Future research will attempt to overcome these limitations.
CONCLUSIONSCA of the balloon-expandable Myval TAVI device can be achieved based on the analysis of the CT allowing a patient-specific orientation of the valve when crimped. As a result, moderate and severe CMA and the risk of coronary overlap of the left main can be successfully avoided. Cross validation of this technique in larger series is ongoing (NCT05097183).
FUNDINGThis investigation received funding resources from the Sociedad Española de Cardiología (SEC) with the grant number: SEC/FEC-INV-CLI 21/023. Alfredo Redondo Diéguez is a beneficiary of a Contrato Rio Hortega grant from the Instituto Carlos III: CM20/00068. I.J. Amat-Santos is principal investigator of a FIS (Fondo de Investigación en Salud) grant No. PI21/01188 (Instituto de Salud Carlos III, Madrid, Spain).
AUTHORS’ CONTRIBUTIONSA. Redondo, C. Baladrón, and I.J. Amat-Santos conceived the original idea. S. Santos-Martínez, A. Redondo, E. Gonzalez-Bartol, A. Barrero, P. Sánchez-Luna, A. Revilla-Orodea, C. Baladrón, A. Serrador, J.A. San Román, and I.J Amat-Santos conducted the research. All authors approved the final version of the manuscript.
CONFLICTS OF INTERESTI.J Amat-Santos is proctor for Meril Life, Medtronic, and Boston Scientific.
- •
Commissural alignment (CA) has emerged as a topic of great interest in parallel with the growing number of low-risk patients treated with TAVI. The greater long-term survival implies an increased number of patients requiring coronary re-access and showing valve degeneration and need for TAVI-in-TAVI with the potential risk of coronary obstruction. While several strategies for CA have been developed for self-expandable devices, some of them require manipulation of the delivery system during implantation, which requires the identification by angiography of the commissural posts in the crimped valve, an aspect that is extremely challenging with balloon-expandable crimped valves.
- •
The final orientation of the implanted TAVI can be predicted by computed tomography analysis. This has already been proved for self-expandable devices, requiring the insertion of the delivery system in a patient-specific rotation. For balloon-expandable TAVI, the valve itself is rotated during its crimping on the balloon to a patient-specific orientation. This avoided moderate and severe misalignment of the commissures and also the overlapping of the commissural posts with the ostium of left main in all patients. Investigation to determine the hemodynamic and clinical impact of this strategy is warranted.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2022.03.003