Hypertension is one of the most prevalent and poorly controlled risk factors, especially in patients with established cardiovascular disease (CVD). The aim of this study was to describe the rate of blood pressure (BP) control and related risk factors.
MethodsMulticenter, cross-sectional and observational registry of patients with hypertension recruited from cardiology and primary care outpatient clinics. Controlled BP defined as <140/90mmHg.
Results55.4% of the 10 743 patients included had controlled BP and these had a slightly higher mean age. Patients with uncontrolled BP were more frequently male, with a higher prevalence of active smokers, obese patients, and patients with diabetes. The rate of controlled BP was similar in patients with or without CVD. Patients with uncontrolled BP had higher levels of blood glucose, total cholesterol, low density lipoproteins and uric acid. Patients with uncontrolled BP were receiving a slightly higher mean number of antihypertensive drugs compared to patients with controlled BP. Patients with CVD were more frequently receiving a renin-angiotensin-aldosterone axis inhibitor: 83.5% vs. 73.2% (P<.01). Multivariate analysis identified obesity and current smoking as independently associated with uncontrolled BP, both in patients with or without CVD, as well as relevant differences between the two groups on other factors.
ConclusionsRegardless of the presence of CVD, 55% of hypertensive patients had controlled BP. Lifestyle and diet, especially smoking and obesity, are independently associated with lack of BP control.
Keywords
.
INTRODUCTIONHypertension (HT) is one of the most prevalent population risk factors,1, 2, 3 especially in patients with established cardiovascular disease (CVD).4, 5, 6, 7 Controlling HT leads to significant reductions in the prevalence and incidence of target organ damage8, 9 and mortality from CVD.10, 11 However, HT is also one of the most poorly controlled risk factors in patients with and without CVD.4, 6, 7, 12 This highlights the difficulties involved in regulating and controlling blood pressure (BP) and the need to consider lifestyle and diet as well as tolerance and adherence to treatment with several families of antihypertensive drug.13
Controlling HT often requires the use of several antihypertensive agents, especially in elderly patients or those with stroke or diabetes mellitus (DM).14 The European Society of Cardiology and European Society of Hypertension (ESC/ESH) guidelines for the treatment of HT have emphasized that all drugs are equally useful in controlling the condition and that the goal of treatment should be to maximize reduction of cardiovascular risk.14 However, they also listed a number of situations in which a particular group of drugs should be used, especially when CVD is present. Through this analysis of data from the CARDIOTENS 2009 study, we aimed to investigate BP control in a large contemporary sample of patients diagnosed with HT and to determine the variables associated with control in patients with and without CVD.
METHODS Study DesignThe CARDIOTENS 2009 registry was an observational, multicenter, cross-sectional epidemiological study designed by the Hypertension Section of the Spanish Society of Cardiology, and supported by the Research Agency of the Spanish Society of Cardiology. Its aim was to determine the prevalence and control of HT in clinical practice. Patients were recruited from primary care and outpatient cardiology clinics. Inclusion criteria were age ≥ 18 years, possibility of access to the complete clinical record and previous diagnoses of CVD, and signed informed consent to participate provided by the patient or a legal representative. Exclusion criteria were addiction to or consumption of illegal drugs (cocaine, cannabis, psychotropic drugs) and refusal to provide written informed consent. Through member lists of the Hypertension Section of the Spanish Society of Cardiology and listings of doctors in health-care areas in Spain's 41 provinces, 542 physicians were randomly selected. Of those, 89.1% were from primary care settings and 10.9% from cardiology outpatient clinics. Each participating physician agreed to include the first 6 patients meeting the study inclusion criteria on each day of the first week of November 2009. In total, 25 137 patients were recruited, of whom 15 102 (60.1%) had some risk factors or CVD. For the present study, we analyzed the 10 743 patients with a history of HT.
A paper-based, study-specific questionnaire was developed and completed for each patient. As in the 1999 CARDIOTENS registry,4 information was first collected on sociodemographic characteristics, presence of CVD, cardiovascular risk factors, and the patient's clinical history. If diagnosed CVD (ischemic heart disease, angina or heart attack, heart failure or stroke) or risk factors (dyslipidemia, HT, DM or tobacco consumption) were reported in the first section of the questionnaire, more detailed information was collected in a second section dealing with treatment, electrocardiogram (ECG) characteristics, echocardiography, and laboratory data. Patients were required to have ECG data and / or blood tests from the previous 6 months and the study protocol recommended requesting these tests if they were not available from that period. However, patients were not excluded from the study if these data were not available at the enrollment visit or subsequently. BP values and heart rate were collected at the time of consultation. The data collection protocol had to be corrected after printing as diuretics were not included in the section on antihypertensive treatment, but in “other treatments.”
Study VariablesHT was considered to be present if 2 consecutive measurements ≥ 140/90mmHg were obtained or if the patient was taking antihypertensive treatment. HT was considered controlled if the objectives in the re-evaluated 2009 guidelines were met (<140/90mmHg).15 A patient was considered to have a history of dyslipidemia if a prior diagnosis was recorded in the patient's medical records or if they had total cholesterol >220mg/dl or low density lipoproteins (LDL) >160mg/dl.16 Likewise, patients were considered to have DM if there was a prior record of the diagnosis in the medical records, if the patient was taking drug treatment for the disease, or if fasting blood glucose levels of >126mg/dl were recorded on 2 consecutive occasions.17 Patients were considered obese if they had a body mass index (BMI) >30 and were considered to have abdominal obesity when waist circumference was >102cm in men or >88cm in women.16 The glomerular filtration rate was estimated from serum creatinine using the formula from the Modification of Diet in Renal Disease study18: 186×creatinine − 1154×age − 0.203 (× 0.742 for women).
A history of atrial fibrillation was recorded if it was included in any medical report or if there was any ECG recording in the patient's clinical history. A history of ischemic heart disease was recorded for all patients whose medical records or medical reports provided by the patient showed a prior history of myocardial infarction, stable or unstable angina, percutaneous or surgical coronary revascularization, or positive results on ischemia induction (exercise stress test, scintigraphy, stress echocardiogram, etc.). Heart failure was recorded for patients with at least one hospital admission in which this diagnosis was recorded at discharge, as well as for patients with signs and symptoms of the disease and a compatible imaging test (echocardiogram, chest X-ray.). A history of stroke was recorded when a diagnosis of ischemic, hemorrhagic, or transient stroke was included in medical records or a medical report. A history of claudication when walking, lower extremity revascularization, amputation, or an established diagnosis were coded as peripheral arterial disease. The analysis of CVD patients was performed after pooling results from patients with ischemic heart disease, heart failure, peripheral arterial disease, or stroke. Chronic obstructive pulmonary disease (COPD) was recorded as present if the diagnosis figured in the clinical history or if the patient was taking specific medication for the disease.
Statistical AnalysisData were processed using SPSS 15.0 (SPSS Inc., Chicago, Illinois, United States) and 10.0/SE STATA (Stata Corp, College Station, Texas, United States). All variables showed a normal distribution and are presented as means±standard deviation. Categorical variables were assessed using the χ2 test and continuous variables using the Student t test or ANOVA, depending on the number of groups to be compared. Multivariate analysis was performed using binary logistic regression with the forward conditional method. Uncontrolled blood pressure (>140/90mmHg) was entered as the dependent variable and independent variables were those found to be statistically significant in univariate analysis and could have clinically plausible involvement. Independent variables included in the final model were age, sex, DM, current smoker, dyslipidemia, BMI >30, abdominal obesity, COPD, and number of antihypertensive drugs. The possible effect of presence of CVD on the associations explored in the multivariate model was evaluated by analyzing interactions. Model calibration was assessed using the Hosmer-Lemeshow statistic. The model's discriminatory power was assessed using the area under the ROC (receiver-operator characteristics) curve obtained by analyzing the probability of the value predicted by the multivariate model. Internal cross-validation was used to affirm the robustness of the analysis by evaluating the predictive value of the multivariable model in a random selection of 25% (n=2637) of the sample. The results of the multivariate model are adjusted and presented as odds ratios and 95% confidence intervals (CI). Rate of BP control was compared between the two registries using the Student t test. Percentages in each of the records were used to calculate the variance. Statistical significance was set at P<.05.
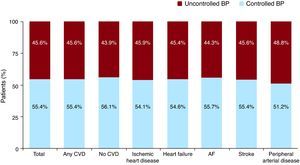
RESULTSOf the 10 743 patients with HT, 5949 (55.4%; 95% CI, 55.1%-55.7%) had controlled BP, compared with 40% (95% CI, 39.9%-40.1%) in the 1999 CARDIOTENS registry, giving a relative increase of 38.5% (P<.01) in the rate of BP control. Patients with uncontrolled BP were slightly younger and more frequently male, with a higher prevalence of active smokers, obese patients, and patients with DM (Table 1). Although no differences were observed in the prevalence of each individual CVD, patients with uncontrolled BP had more often had at least one of the CVDs studied. Nevertheless, the degree of BP control did not vary by presence or absence of CVD (Figure 1). The results of laboratory tests showed that patients with uncontrolled BP had higher levels of blood glucose, total cholesterol, LDL, and uric acid (Table 2).
Table 1. General Characteristics of the Population in Terms of Blood Pressure Control.
| Total | Controlled BP | Uncontrolled BP | P | |
| Patients, n (%) | 10 743 (100) | 5949 (55.4) | 4794 (44.6) | |
| Age | 66.1±12.7 | 66.5±12.7 | 65.5±12.8 | < .01 |
| Male | 50.1 | 48.8 | 51.7 | < .01 |
| Systolic BP (mmHg) | 138.5±15.1 | 127.6±8.7 | 149.4±11.9 | < .01 |
| Diastolic BP (mmHg) | 80±11.2 | 75.1±8.6 | 84.9±11.5 | < .01 |
| Abdominal girth (cm) | 97.8±14.1 | 96.3±13.8 | 99.5±14.3 | < .01 |
| Abdominal obesity | 36.1 | 31.5 | 41.8 | < .01 |
| BMI | 28.9±4.8 | 28.5±4.7 | 29.3±4.9 | < .01 |
| BMI>30 | 30.7 | 25.9 | 36.6 | < .01 |
| Diabetes mellitus | 32.6 | 31.4 | 34.1 | < .01 |
| Dyslipidemia | 49.8 | 49.4 | 50.3 | .37 |
| Smoker | 13.9 | 11.4 | 17.1 | < .01 |
| Prior IHD | 18.6 | 18.2 | 19.1 | .21 |
| Prior heart failure | 12.5 | 12.4 | 12.7 | .54 |
| Prior stroke | 7 | 6.9 | 7.2 | .57 |
| LVH | 17.2 | 14.9 | 20.1 | < .01 |
| Peripheral arterial disease | 5.1 | 4.7 | 5.5 | .04 |
| Atrial fibrillation | 12.5 | 12.6 | 12.4 | .78 |
| CVD | 32.9 | 32.1 | 33.9 | .04 |
| COPD | 13.4 | 12.5 | 14.6 | < .01 |
BMI, body mass index; BP, blood pressure; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease (stroke, heart failure, or peripheral arterial disease); IHD, ischemic heart disease; LVH, left ventricular hypertrophy.
Quantitative variables are presented as mean±standard deviation.
Figure 1. Blood pressure control by presence or absence of cardiovascular disease and each type of heart disease. AF, atrial fibrillation; BP, blood pressure; CVD, cardiovascular disease.
Table 2. Results of Patient Blood Tests According to Degree of Blood Pressure Control.
| Total | Controlled BP | Uncontrolled BP | P | |
| Glycemia (mg/dl) | 112.4±36.1 | 109.8±34.4 | 115.2±37.6 | < .01 |
| Total cholesterol (mg/dl) | 203±43.5 | 198.9±42.3 | 207.6±44.4 | < .01 |
| LDL (mg/dl) | 122.2±36 | 118.8±34.3 | 126.1±37.5 | < .01 |
| HDL (mg/dl) | 52.6±15.7 | 52.9±15.5 | 52.3±15.9 | .06 |
| Triglycerides (mg/dl) | 143.1±67.3 | 138.3±67.1 | 148.5±67.2 | < .01 |
| Creatinine (mg/dl) | 0.75±0.81 | 0.76±0.84 | 0.75±0.77 | .81 |
| Glomerular filtration (ml/min/1.72 m2) | 78.2±213.1 | 76.4±61.8 | 80.2±30.7 | .49 |
| Glycohemoglobin (%) a | 6.8±1.3 | 6.8±1.4 | 6.8±1.3 | .22 |
| Hemoglobin (g/dl) | 13.5±1.6 | 13.4±1.5 | 13.5±1.6 | .03 |
| Uric acid (mg/dl) | 5.6±1.6 | 5.5±1.6 | 5.7±1.6 | < .01 |
BP, blood pressure; HDL, high density lipoproteins; LDL, low density lipoproteins.
Quantitative variables are presented as mean±standard deviation.
a Only in patients with a history of diabetes mellitus.
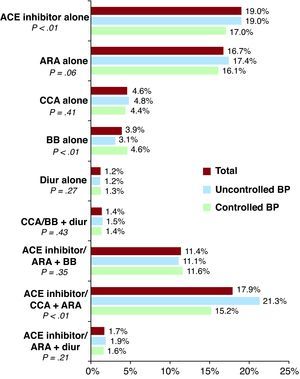
Patients with uncontrolled BP were receiving a slightly higher mean number of antihypertensive drugs compared to those with controlled BP: mean, 1.57±0.80 vs. 1.45±0.78 (P<.01); median, 1 (1-2) vs. 1 (1-2) (P<.01). In general, patients with CVD were treated more frequently (83.5% compared to 73.2% in patients without CVD; P<.01) with drugs that block the renin-angiotensin-aldosterone system (RAAS), such as angiotensin enzyme converting (ACE) inhibitors or angiotensin II AT1 receptor antagonists (ARA). Figure 2 shows the antihypertensive treatments recorded and indicates that there were no major differences in treatment strategies based on BP control.
Figure 2. Utilization rate of each family of antihypertensive drugs or antihypertensive strategy based on the degree of blood pressure control. ACE, angiotensin-converting enzyme; ARA, angiotensin II AT1 receptor antagonists; BB, betablockers; BP, blood pressure; CCA, calcium channel antagonist; Diur, diuretics.
Finally, we performed a multivariate analysis that included all clinically plausible variables which had shown a statistically significant difference in bivariate analysis. The analysis showed a significant interaction related to lack of BP control between presence of CVD and being male (P<.01), dyslipidemia (P=.04), the number of antihypertensive drugs (P<.01), and COPD (P=.01). As shown in Table 3, obesity and active smoking were associated with lack of BP control in patients with and without CVD. The model showed a satisfactory fit (P=.3, χ2=6.94) and good discriminative power (area under the curve=0.73; 95% CI, 0.71 to 0.75; P<.01). The validation analysis showed similar values in the randomly selected 25% of the sample (AUC=0.71; 95% CI, 0.68 to 0.76; P<.01).
Table 3. Results of Multivariate Analysis of Variables Associated With Uncontrolled Blood Pressure.
| Variables | All patients | Patients with CVD |
| Age | 1 (0.99-1); P=.2 | 0.99 (0.99-1); P=.84 |
| Male | 1.05 (1.03-1.08); P<.01 | 0.97 (0.95-1); P=.1 |
| Smoker | 1.2 (1.06-1.37); P<.01 | 1.62 (1.28-2.05); P<.01 |
| BMI>30 | 1.35 (1.21-1.51); P<.01 | 1.36 (1.17-1.59); P<.01 |
| Abdominal obesity | 1.38 (1.24-1.54); P<.01 | 1.2 (1.04-1.4); P=.01 |
| Diabetes mellitus | 1.05 (0.94-1.18); P=.38 | 1.16 (1.01-1.34); P=.04 |
| Dyslipidemia | 1.01 (1.06-1.37); P=.89 | 0.83 (0.72-0.97); P=.02 |
| Number of antihypertensive drugs | 1.45 (1.35-1.55); P<.01 | 1.14 (1.05-1.25); P<.01 |
| COPD | 1.17 (0.99-1.4); P=.07 | 0.84 (0.71-0.99); P=.01 |
BMI, body mass index; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease (including ischemic heart disease, heart failure, stroke and peripheral arterial disease).
The main result of this analysis of the CARDIOTENS 2009 data is that lack of BP control is associated with factors related to lifestyle and diet, especially obesity and smoking, and that the presence of CVD interacts with BP control. Patients enrolled in the registry showed similar characteristics to those recruited in other studies2, 6, 12, 19, 20, 21, 22, 23 so the present results can likely be extrapolated to daily clinical practice. The rate of controlled BP was higher than that observed in previous HT registries4, 12 and coincides with the growing trend reported in other countries, including the United Kingdom, which reported a rate of controlled BP of 52%,22 and the United States, with a corresponding figure of 50.1%.2 Comparison with the 1999 CARDIOTENS registry also showed a significant and relevant increase of 38.5% in the rate of HT control.
Measures aimed at changing dietary patterns and sedentary lifestyles are the first step in treating HT,14 though they are also useful in combating other risk factors such as hypercholesterolemia16 or DM17 and should be maintained even when initiating or maintaining drug treatment. However, the number of scientific publications dealing with lifestyle control and diet in cardiovascular prevention is much lower than those addressing risk factors, which probably reflects the lower interest in this aspect of treatment.24 Obesity forms the pathophysiological basis underlying most cardiovascular risk factors25 and is also an independent risk factor for CVD.26 It is highly prevalent in patients with HT, though weight loss is often an elusive goal despite its known benefits for HT and associated metabolic abnormalities.27
The relationship between smoking and CVD has been clearly established, particularly in terms of its involvement in atherosclerosis. Our results show that smoking is also independently associated with lack of BP control and therefore they extend the relevance of tobacco control in cardiovascular prevention. Smoking induces endothelial dysfunction, vasoconstriction, insulin resistance, and dyslipidemia, certain forms of which could explain our results.28 On the other hand, smokers are more sedentary and have less healthy29 diets and these are factors which can directly raise BP. Unfavorable lifestyles and diets are also associated with poorer compliance with medical treatment30 and a different perception of individual cardiovascular risk.
DM, old age, and CVD are usually considered impediments to BP control.14 The VIIDA registry, which was also carried out in Spain, identified DM and left ventricular hypertrophy as the main factors associated with lack of BP control, while CVD was associated with greater control.31 In a sub-analysis of the PREV-ICTUS study, which included patients with HT aged >60 years, obesity was identified as one of the factors independently associated with lack of BP control.32 In a registry of patients with CVD recruited in primary care settings, obesity, DM, peripheral arterial disease, and prior stroke were also identified as factors associated with lack of BP control.33 Our data also showed obesity to be a factor in poor BP control, but further identified smoking as a risk factor. Smoking is not mentioned as a risk factor in any of the earlier registries. Moreover, the fact that diabetes is not associated with poorer BP control could be explained by the fact that we adopted the goal for BP control (below 140/90mmHg) recommended in the European Society of Hypertension's updated treatment guidelines for HT.15
We also found that age and CVD were not associated with worse BP control, which could reflect an improvement in the treatment of these patients. However, a significant interaction of CVD in the relationship between some variables and lack of BP control was observed. The above mentioned United States2 and United Kingdom22 registries used a population design, but did not analyze differences in the degree of BP control based on the presence of CVD. Our results provide evidence that the presence of CVD modifies the association of certain variables to lack of BP control. Of particular relevance is the finding that DM is associated with lack of BP control only in patients with CVD. This finding coincides with those of previous registries31 and could explain why patients with DM have not experienced the same decline in CVD mortality as nondiabetic patients,34 despite the known mortality benefits associated with better control of cardiovascular HT.11 The number of antihypertensive drugs used showed a much weaker association with stroke, which reflects use of these drugs for indications other than the mere control of BP. These include the antianginal effectiveness of betablockers, calcium antagonists or ACE inhibitors and ARA in the presence of heart failure or ventricular dysfunction. Furthermore, the presence of CVD cancelled out the association between being male and lack of BP control observed in patients without CVD. On the other hand, this phenomenon was observed in the case of dyslipidemia, which was associated with better BP control in CVD patients, which probably indicates increased awareness about the disease, the need to follow lifestyle and dietary measures and to comply appropriately with the recommended medication.
Finally, if we compare data from this study with that from its predecessor, performed in 1999,4 it can be observed that the level of BP control has noticeably increased, as BP was controlled in fewer than 40% of patients with HT but without CVD and in 20% of patients with CVD in the earlier study. This trend towards improved control rates is consistent with results published recently in other countries, such as 50.1% according to the third NHANES (National Health and Nutrition Examination Survey)2 the United States or 54% in the United Kingdom.22 These figures coincide almost exactly with our results. Moreover, although RAAS blockade was used in under 50% of patients with CVD in the previous registry its use is now widespread, a finding which also mirrors results from other national12, 19, 20 and international22, 23 registries. The fact that the rate of control in the current registry is similar in patients with and without CVD may be due to the unification of the control target (<140/90mmHg15), but also to improvements in patient treatment.7, 20 The evolution in treatment can be influenced by differences in diagnostic criteria, marketing of new drugs, or prescription-related legislation, but it certainly reflects an important advance in the treatment of patients with HT.
The CARDIOTENS 2009 registry had some limitations that deserve consideration. First, as a cross-sectional observational study, it is not possible to identify risk factors, only associations between clinical variables. Also, these designs often lead to the observation that patients with poorer BP control tend to have more treatments due to their being more complex patients. It is also important to note that other factors that could have been identified as limiting BP control, including race, cultural factors, adherence, other concomitant treatments, or duration of HT, were not analyzed. Moreover, the fact that most patients were included by primary care physicians may mean that they are not representative of other areas of medicine in which HT patients are treated, such as internal medicine, nephrology, or neurology. Another important limitation is that investigators were not selected randomly from all physicians nationwide, but by randomly inviting doctors registered in community listings. Physicians participating in the study may therefore have been more motivated and more aware of the importance of these studies. Notably, the prevalence of diuretic use was very low, a finding which is clearly related to the data collection protocol, which had to be corrected once printed.
CONCLUSIONSRegardless of the presence of CVD, 55% of patients with HT had controlled BP. Lifestyle and diet, especially smoking and obesity, were related to lack of BP control.
FUNDINGThe CARDIOTENS 2009 registry was supported by an unrestricted grant from RECORDATI laboratories, Spain.
CONFLICTS OF INTERESTNone declared.
Received 20 December 2010
Accepted 4 March 2011
Corresponding author: Departamento de Cardiología, Hospital Universitario de San Juan, Ctra. Valencia-Alicante s/n, 03550 Sant Joan d’Alacant, Alicante, Spain. acorderofort@gmail.com