The incidence and prevalence of atrial fibrillation (AF), a major risk factor for stroke, has increased substantially in the past few years. However, several studies have reported a decline in AF-related stroke rates associated with higher uptake of direct oral anticoagulants (DOACs). This ecological study evaluated the association between DOAC uptake in Spain and the incidence rate (IR) of AF-related ischemic stroke.
MethodsData were obtained from the Registry of Activity of Specialized Healthcare of the Spanish Ministry of Health (RAE-MDS). AF-related ischemic strokes were identified using International Classification of Diseases codes. IR were age-standardized and adjusted to the 2013 European standard population. Poisson regression models were used to identify the association between DOAC uptake and AF-related ischemic stroke in patients aged ≥ 65 years.
ResultsBefore the use of DOACs, the adjusted IR of AF-related ischemic stroke increased steadily from 2005 (IR=2.20 per 100 000 person/y) to 2012 (IR=2.67). Upon DOAC uptake in Spain from 2012 onwards for AF-related ischemic stroke prevention, the IR remained constant or decreased slightly (IR in 2018=2.66). Poisson regression showed that DOAC uptake was a significant predictor for the rate of AF-related ischemic stroke in patients older than 65 years (IRR=0.995; 95%CI, 0.995-0.996).
ConclusionsThis study shows an association between DOAC use and a reduced incidence of AF-related ischemic stroke. While this association is based on aggregate data and cannot demonstrate causality, these findings suggest that higher DOAC uptake could improve health outcomes in AF patients in Spain.
Keywords
Atrial fibrillation (AF) is one of the most frequent cardiac arrhythmias1 and is independently associated with increased morbidity, mortality, and impaired quality of life.2 Both the incidence and prevalence of AF have increased substantially in the past few years, mainly due to population aging, a rise in the number of cardiovascular risk factors, and longer survival in persons with cardiovascular disease. In Spain, the prevalence of AF is> 4% for the population older than 40 years, rising to 8.5% among patients older than 60 years, and 16.5% among those older than 85 years.3
AF is a major risk factor for stroke, increasing risk by 4- to 5-fold across all age groups.4 The recurrence rate of AF-related ischemic stroke is approximately 12% at 3 months, which is higher than the rate for other stroke types. Patients with AF are likely to have more severe strokes than those without AF, resulting in longer hospital stays and higher mortality rates.5
Oral anticoagulation is the gold standard for prophylaxis in AF-related stroke. Oral vitamin K antagonists (VKA) were the mainstay of long-term anticoagulant practice starting in the early 1950s until the last few years. However, their use in clinical practice is challenging, due to problems such as a narrow therapeutic index, drug-drug and drug-food interactions, slow onset and offset, wide variability in individual doses, and the need for frequent international normalized ratio (INR) monitoring. Clinical guidelines now recommend novel direct oral anticoagulants (DOACs), such as rivaroxaban, dabigatran, edoxaban, and apixaban over VKAs for stroke prevention in patients with AF.6 The evidence demonstrating the benefits of DOACs vs VKAs in AF-related stroke prevention has been shown in several randomized clinical trials, meta-analyses of these trials, and real-world studies.7 In addition, several retrospective studies from different European countries have observed a decline in AF-related stroke rates associated with higher DOAC uptake.8–12 However, the relationship between DOAC use and AF-related stroke in Spain remains unknown. DOACs have been approved in Spain since 2012 for the prevention of stroke and systemic embolism in patients with nonvalvular AF, but their use is lower than that in other European countries because they are used as second-line drugs after VKA and use is subject to approval in the form of an inspection visa (ex-ante approval).13,14
Given the existing evidence, the present study aimed to analyze the epidemiology of AF-related ischemic stroke and its association with DOAC uptake in Spain. Specifically, a) the IRs of nonvalvular AF-related ischemic stroke before and after the introduction of DOACs as a treatment option for stroke prevention in patients with AF; and b) the association between DOAC uptake and the frequency of AF-related ischemic strokes.
METHODSData sourceData were obtained from the Registry of Activity of Specialized Healthcare-Minimum Data Set (RAE-MDS) of the Spanish Ministry of Health, Consumption and Social Welfare.15 The RAE-MDS is clinical-administrative database and its completion is compulsory for hospitals of the Spanish National Health System, with more than 4 000 000 hospital admissions collected per year. Data from 2005 to 2015 were coded according to the International Classification of Diseases (ICD-9), and data for 2016 and 2018 were coded according to the ICD-10. Information was received on the following variables: year, sex, type of hospital discharge, age, autonomous community, length of hospital stay, main diagnosis, secondary diagnoses, date of birth, date of admission, date of discharge, service, or readmission. For each patient, the primary diagnosis and 14 secondary diagnoses were obtained. As this is a population-based epidemiological study using anonymized data from the RAE-MDS, there was no requirement for ethical approval.
In 2016, the switch from the ICD-9 to ICD-10 codes led to incorrect registration of some diagnoses and an underestimation of the total number of diagnoses. Therefore, data from 2016 and 2017 should be interpreted with caution (especially those for 2016). Data were acquired in Microsoft Access Database files, converted into Microsoft Excel spreadsheets, and imported into the IBM SPSS Statistics software. Approximately 100 000 hospital admissions with a primary diagnosis of “cerebrovascular disease” were collected each year from 2005 to 2018 in the RAE-MDS database. Three secondary diagnoses were reported for more than 85% of the patients and at least 6 secondary diagnoses were reported for more than 50% of the patients, which is an indication of the overall quality of the database.
Oral anticoagulant uptake rates in Spain were estimated based on unit sales and prescription data provided by IQVIA. IQVIA collects monthly data from all public and private prescriptions dispensed throughout Spain. Spanish monthly unit sales from January 2002 to December 2018 were analyzed for the following treatments: apixaban, edoxaban, dabigatran etexilate, rivaroxaban, and acenocoumarol. For DOACs, each unit sale was associated with 1 month of treatment. In addition, we considered that all DOAC sales were correlated only with the treatment of AF since DOAC use in other approved indications is very low in Spain. For acenocoumarol, the most widely used VKA in Spain, we considered a daily dose of 2 mg and the percentage of use only in the AF indication, based on the Study of Medical Prescription, to obtain the monthly unit sales. The Study of Medical Prescriptions is a quarterly study conducted by IQVIA and involves 965 physicians. This study provides information on medical prescription patterns, relating diagnoses with the prescribed treatment and with the treated patients. Yearly use was calculated per drug as the sum of monthly use. Finally, the percentage of DOAC uptake was calculated based on the sum of apibaxan, edoxaban, dabigatran etexilate, and rivaroxaban use divided by the total of oral anticoagulant use (sum of the 4 DOACs + acenocoumarol).
Atrial fibrillation-related ischemic stroke and incidence rateAF-related ischemic strokes were defined as those with “ischemic stroke” as the primary diagnosis and “AF” as a secondary diagnosis, given that neither nonvalvular AF nor AF-related stroke has a specific ICD code (table 1 and table 2 of the supplementary data). The following comorbidities were extracted from the secondary diagnoses: hypertension, diabetes mellitus, lipoprotein metabolism disorder, heart failure, and ischemic heart disease (table 2 of the supplementary data).
Age-standardized crude incidence rates (IR) were calculated by dividing the number of AF-related ischemic strokes in a calendar year by the total number of people in Spain in each age group during the same year. Demographic information was provided by the National Institute of Statistics.16 The IR was adjusted to the 2013 European standard population using 5-year age groups17 to allow international comparisons. The adjusted IR of 10-year age groups was calculated as the mean of the adjusted IR of the two 5-year age groups within that 10-year age group. Incidence rate ratios (IRR) were calculated by dividing the incidence rates of the 2 years of interest.
Statistical analysesStatistical significance was calculated with ANOVA tests using polynomial contrast and Student-Newman-Keuls tests for baseline characteristics over time. Rates were also calculated for qualitative variables and the chi-square test was used to analyze their statistical significance. Linear regression was used to test for linear temporal trends in the following independent variables: number of ischemic and AF-related ischemic strokes, rate of DOAC uptake, and patient characteristics.
To investigate the association between the frequency of AF-related stroke in patients older than 65 years and DOAC uptake, a Poisson regression model was used and IRR were reported. The dependent variable in the Poisson regression was the number of AF-related ischemic strokes per year in patients older than 65 years, while the independent variables were DOAC uptake (as %), time (as a discrete variable, year) and autonomous community (as a discrete variable) to account for the variability in DOAC use observed in the different Spanish autonomous communities. The Spanish population older than 65 years extracted from the website of the National Institute of Statistics16 was used as the exposure variable or reference group. Poisson regression was also used to investigate the association between the number of deaths in patients with AF-related ischemic stroke and DOAC uptake. In the Poisson regression, the dependent variable was the frequency of deaths per year while the independent variables were DOAC uptake and time (year). The number of AF-related ischemic strokes per year was used as the exposure variable or reference group.
Statistical significance was set at P (2-sided)<0.05. The statistical analysis was performed using the IBM SPSS statistics package, version 27.0 (SPSS, United States).
RESULTSPatient populationWe included 910 641 patients with a primary diagnosis of ischemic stroke in Spain between 1 January 2005 and 31 December 2018; of these, 26% (n=233 935) were patients with a secondary diagnosis of AF and who were therefore considered patients with AF-related ischemic stroke (table 1).
Number of total ischemic strokes and AF-related ischemic strokes by year.
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | Total | p trend | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ischemic stroke | 51 423 | 57 018 | 60 569 | 63 742 | 64 345 | 65 726 | 65 599 | 67 235 | 68 806 | 68 060 | 69 293 | 67 396 | 69 613 | 71 816 | 910 641 | <.001 |
| AF-related ischemic stroke | 12 046 (23) | 13 237 (23) | 14 050 (23) | 15 410 (24) | 15 842 (25) | 16 743 (25) | 16 814 (26) | 17 810 (26) | 18 147 (26) | 18 027 (26) | 18 448 (27) | 18 016 (27) | 19 311 (28) | 20 034 (28) | 233 935 (26) | <.001 |
AF, atrial fibrillation.
The data are expressed as absolute numbers or No. (%).
The rate of AF in ischemic stroke increased over the years, from 23% in 2005 to 28% in 2018. There was a significant positive association between time (years) and the number of cases of AF in ischemic stroke (P<.001).
The baseline characteristics of AF-related ischemic stroke patients are shown in table 2. The age of patients with AF-related ischemic strokes significantly increased from 2005 to 2018 (1-way ANOVA, P<.001), with a mean age of 80.5 years in 2018. Across all years, AF-related ischemic strokes were more common in women than in men (women 55.4% vs men 44.6% in 2018).
AF-related ischemic stroke patient characteristics.
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | p trend | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age, y | 78.38± 9.18 | 79.06±9.14 | 79.12±9.15 | 79.25±9.32 | 79.70±9.08 | 79.69±9.15 | 79.82±9.25 | 79.87±9.17 | 80.12±9.16 | 80.22±9.35 | 80.38±9.39 | 80.31±9.50 | 80.49±9.53 | 80.49±9.69 | <.001 |
| Female sex | 58.14 | 59.08 | 58.97 | 58.01 | 59.03 | 58.39 | 57.98 | 57.78 | 57.09 | 57.25 | 56.07 | 55.95 | 55.58 | 55.42 | <.001 |
| Hypertension | 55.04 | 56.50 | 56.78 | 57.37 | 57.77 | 58.96 | 58.59 | 57.89 | 57.92 | 58.00 | 56.36 | 56.17 | 57.09 | 53.87 | .586 |
| Lipoprotein metabolism disorders | 19.97 | 20.75 | 21.94 | 24.30 | 26.61 | 27.75 | 29.36 | 31.76 | 33.66 | 34.65 | 34.97 | 35.04 | 37.15 | 39.19 | <.001 |
| Diabetes mellitus | 27.54 | 26.72 | 27.73 | 27.87 | 28.75 | 28.37 | 28.88 | 28.41 | 29.22 | 29.00 | 28.96 | 28.59 | 29.40 | 30.04 | <.001 |
| Heart failure | 7.54 | 8.23 | 8.10 | 8.53 | 8.80 | 9.42 | 8.77 | 9.42 | 9.11 | 9.51 | 9.19 | 10.50 | 10.92 | 11.44 | <.001 |
| Ischemic heart disease or cardiomyopathy | 15.13 | 15.10 | 14.42 | 15.11 | 14.44 | 14.79 | 14.32 | 14.48 | 14.34 | 13.49 | 13.19 | 15.10 | 15.42 | 15.39 | .765 |
AF, atrial fibrillation.
The data are expressed as mean±standard deviation or percentage.
For all years, more than 50% of patients with AF-related ischemic stroke also had hypertension. The percentage of patients with comorbid lipoprotein metabolism disorders, diabetes mellitus, and heart failure increased between 2005 and 2018, while the presence of hypertension and ischemic heart disease/cardiomyopathy remained steady (table 2).
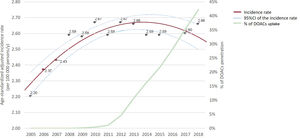
DOAC uptakeThe percentage of DOACs, which have been indicated in Spain for the prevention of stroke and systemic embolism since 2012,13 increased, rising steeply and steadily from 4.6% in 2012 to 42.22% in 2018 (table 3).
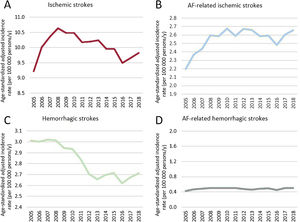
Incidence rate of atrial fibrillation-related ischemic strokeThe trend in the IR of ischemic, hemorrhagic, AF-related ischemic, and AF-related hemorrhagic strokes in 2005 and 2018 is shown in figure 1. The IR were age-standardized and adjusted to the 2013 European standard population. The IR of ischemic stroke increased from 9.22 (per 100 000 persons/y) in 2005 to 10.6 in 2008. From 2008 onwards, the IR decreased to 9.8 in 2018 (figure 1A). A similar trend was seen in the IR of hemorrhagic stroke, which decreased from 2008 to 2013 (figure 1C). However, the IR of AF-related stroke did not follow the trend observed for total strokes (compare figure 1A to figure 1B; and figure 1C to figure 1D). Despite the reductions observed for total ischemic and total hemorrhagic stroke from 2008, the IR of both ischemic and hemorrhagic AF-related strokes increased from 2005 to 2011.
When we focused on AF-related ischemic strokes, the IR increased from 2.20 in 2005 to 2.67 in 2012 (figure 1B and table 4). The highest increase during the period 2005 to 2012 was observed in patients older than 85 years (from 3.32 in 2005 to 4.40 in 2012) in both men and women. The IR was higher in men than in women across all age groups and years (table 4). Upon the introduction of DOACs for the prevention of stroke and systemic embolism13 in 2012, the IR in the general population remained constant or slightly decreased (from 2.67 in 2012 to 2.66 in 2018), with the largest decrease in patients aged 75 to 84 years (from 8.00 in 2012 to 7.68 in 2018). In contrast, the IR increased slightly in patients older than 85 years (from 4.40 in 2012 to 4.50 in 2018). In women aged 65 to 84 years, the IR decreased markedly (IR in women aged 65-74 years in 2012, 3.47; in 2018, 3.08; IR in women aged 75-84 years in 2012, 7.75; in 2018, 7.18), while in men, the IR increased from 2012 to 2018 (from 2.81 to 2.99).
Incidence rate (per 100 000 person/y) age-standardized and adjusted to the European standard population 2013 of AF-related ischemic stroke.
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population | ||||||||||||||
| All ages | 2.20 | 2.37 | 2.43 | 2.59 | 2.58 | 2.67 | 2.59 | 2.67 | 2.66 | 2.59 | 2.59 | 2.48 | 2.60 | 2.66 |
| 65-74 | 3.45 | 3.41 | 3.66 | 3.90 | 3.73 | 4.11 | 3.78 | 4.06 | 3.92 | 3.92 | 3.83 | 3.71 | 3.86 | 4.02 |
| 75-84 | 6.84 | 7.14 | 7.25 | 7.62 | 7.77 | 7.83 | 7.66 | 8.00 | 8.07 | 7.65 | 7.74 | 7.46 | 7.73 | 7.68 |
| ≥ 85 | 3.32 | 4.00 | 4.08 | 4.38 | 4.44 | 4.53 | 4.39 | 4.40 | 4.42 | 4.34 | 4.36 | 4.08 | 4.35 | 4.50 |
| Women | ||||||||||||||
| All ages | 2.08 | 2.25 | 2.32 | 2.42 | 2.45 | 2.52 | 2.41 | 2.49 | 2.45 | 2.38 | 2.34 | 2.25 | 2.36 | 2.40 |
| 65-74 | 2.97 | 2.95 | 3.18 | 3.31 | 3.25 | 3.56 | 3.07 | 3.47 | 3.30 | 3.18 | 2.97 | 2.95 | 3.03 | 3.08 |
| 75-84 | 6.63 | 7.01 | 7.18 | 7.33 | 7.55 | 7.63 | 7.40 | 7.75 | 7.65 | 7.31 | 7.31 | 6.93 | 7.24 | 7.18 |
| ≥ 85 | 3.36 | 4.04 | 4.06 | 4.41 | 4.50 | 4.53 | 4.45 | 4.38 | 4.36 | 4.33 | 4.29 | 4.15 | 4.35 | 4.52 |
| Men | ||||||||||||||
| All ages | 2.28 | 2.43 | 2.50 | 2.70 | 2.64 | 2.77 | 2.71 | 2.81 | 2.85 | 2.76 | 2.83 | 2.75 | 2.93 | 2.99 |
| 65-74 | 4.03 | 3.96 | 4.22 | 4.58 | 4.28 | 4.75 | 4.60 | 4.73 | 4.63 | 4.77 | 4.81 | 4.62 | 4.85 | 5.13 |
| 75-84 | 7.14 | 7.33 | 7.37 | 8.02 | 8.05 | 8.10 | 8.02 | 8.31 | 8.62 | 8.09 | 8.33 | 8.28 | 8.55 | 8.49 |
| ≥ 85 | 2.97 | 3.59 | 3.75 | 3.88 | 3.89 | 4.14 | 3.92 | 4.12 | 4.21 | 4.05 | 4.17 | 3.92 | 4.40 | 4.52 |
AF, atrial fibrillation.
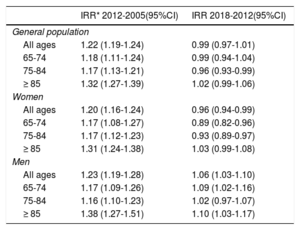
To compare periods before and after DOAC uptake, IRRs were calculated by dividing the IR of the 2 years of interest for the period before and after the introduction of DOACs: 2005 to 2012 and 2012 to 2018 (table 5). The IR of AF-related ischemic stroke increased from 2005 to 2012 (IRR, 1.22; 95% confidence interval (95%CI), 1.19-1.24)), with a higher increase in patients older than 85 years for both men and women. In the post-DOAC introduction period, the IR remained constant or decreased slightly (IRR<1) in the general population and in women younger than 85 years. In men, IRR> 1 in the post-DOAC period indicated an increase in the IR, but this increase was considerably lower than during the pre-DOAC period (2012-2005 IRR, 1.23; 95%CI, 1.19-1.28; 2018-2012 IRR, 1.06; 95%CI, 1.03-1.10).
IRR for the period before (2012-2005) and after (2018-2012) DOAC uptake.
| IRR* 2012-2005(95%CI) | IRR 2018-2012(95%CI) | |
|---|---|---|
| General population | ||
| All ages | 1.22 (1.19-1.24) | 0.99 (0.97-1.01) |
| 65-74 | 1.18 (1.11-1.24) | 0.99 (0.94-1.04) |
| 75-84 | 1.17 (1.13-1.21) | 0.96 (0.93-0.99) |
| ≥ 85 | 1.32 (1.27-1.39) | 1.02 (0.99-1.06) |
| Women | ||
| All ages | 1.20 (1.16-1.24) | 0.96 (0.94-0.99) |
| 65-74 | 1.17 (1.08-1.27) | 0.89 (0.82-0.96) |
| 75-84 | 1.17 (1.12-1.23) | 0.93 (0.89-0.97) |
| ≥ 85 | 1.31 (1.24-1.38) | 1.03 (0.99-1.08) |
| Men | ||
| All ages | 1.23 (1.19-1.28) | 1.06 (1.03-1.10) |
| 65-74 | 1.17 (1.09-1.26) | 1.09 (1.02-1.16) |
| 75-84 | 1.16 (1.10-1.23) | 1.02 (0.97-1.07) |
| ≥ 85 | 1.38 (1.27-1.51) | 1.10 (1.03-1.17) |
DOAC, direct oral anticoagulant; 95%CI, 95% confidence interval; IRR, incidence rate ratio.
In summary, while the IRs of AF-related ischemic stroke increased from 2005 to 2012 (2.20 to 2.67, an increase of 21.6%), this tendency reversed or stabilized after the introduction of DOACs in Spain in 2012 (2.67 to 2.66, a decrease of 0.63%) (figure 1 of the supplementary data). The IRRs of the post-DOACs period (2012-2018) were lower than the IRRs of the pre-DOACs period (2005-2012) across all age groups and both sexes. The temporal trend in AF-related ischemic stroke, which follows an inverted-U-shaped curve, is presented in figure 2 together with the DOAC uptake rates.
Trend in the incidence rate of AF-related ischemic stroke in the general population and percentage of DOAC uptake. In 2016, the International Classification of Diseases (ICD) codes switched from ICD-9 to ICD-10. This switch caused incorrect registration of some diagnoses and underestimation of the total number of diagnoses; therefore, the incidence rate of 2016 was not used for curve fitting. The incidence rate curve fitting was performed with a quadratic model (R2 quadratic=0.825). The incidence rate was adjusted to the 2013 European standard population. AF, atrial fibrillation; 95%CI, 95% confidence interval; DOACs, direct oral anticoagulants.
The age-standardized crude IRs of AF-related ischemic stroke and the IRR calculated with the crude IR are reported in table 3 and table 4 of the supplementary data.
Poisson regression between DOAC uptake and atrial fibrillation-related ischemic strokePoisson regression showed that DOAC uptake was a significant predictor of the rate of AF-related stroke in patients older than 65 years (IRR, 0.995; 95%CI, 0.995-0.996), indicating that for each unit increase in DOAC uptake, the IR of AF-related ischemic stroke in this population decreased by a factor of 0.5%. The population older than 65 years was used as the exposure group.
Length of hospital stay and in-hospital mortality rateThe length of hospital stay and in-hospital mortality rate for AF-related ischemic strokes from 2005 to 2018 are shown in table 6. The number of days of hospital stay days substantially decreased throughout the study period (1-way ANOVA, P<.001). Length of hospital stay was slightly lower in the post-DOAC period (mean, 9.57; SD, 0.16) than in the pre-DOACs period (mean, 11.35; SD, 0.65), decreasing from 2008 to 2012 and stabilizing from 2012 onwards (table 6).
Length of hospital stay and mortality rate of AF-related ischemic stroke.
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospital stay, number of days | 11.88±14.02 | 11.93±13.96 | 11.58±12.25 | 11.80±15.03 | 11.23±12.03 | 10.84±14.01 | 10.18±11.55 | 9.66±10.53 | 9.85±12.82 | 9.50±10.30 | 9.32±10.25 | 9.62±13.02 | 9.52±12.91 | 9.54±18.31 |
| Mortality rate | 15.33 (14.69-15.98) | 16 (15.38-16.63) | 15.72 (15.13-16.33) | 15.47 (14.90-16.04) | 15.57 (15.01-16.14) | 16.16 (15.60-16.72) | 15.21 (14.67-15.76) | 14.97 (14.45-15.50) | 15.1 (14.59-15.63) | 14.8 (14.29-15.32) | 15.35 (14.83-15.87) | 14.88 (14.36-15.40) | 14.16 (13.67-14.65) | 14.6 (14.11-15.09) |
AF, atrial fibrillation; 95%CI, 95% confidence interval; SD, standard deviation.
The data are expressed as mean±standard deviation or % (95%CI).
The in-hospital mortality rate of patients with AF-related ischemic stroke also decreased over time, especially from 2010 to 2018 (table 6). Poisson regression showed that DOAC uptake was a significant predictor of the number of in-hospital deaths in patients with AF-related ischemic stroke (IRR, 0.993; 95%CI, 0.990-0.997) when the number of AF-related strokes was used as an exposure variable.
DISCUSSIONThis study is the first to analyze trends in the IR of AF-related ischemic stroke in Spain during a 14-year period and to evaluate its association with DOAC uptake. We found that the rate of AF in ischemic stroke increased over the years, from 23% in 2005 to 28% in 2018, probably mainly due to population aging and enhanced detection and diagnosis. The IR of AF-related ischemic stroke also increased from 2005 to 2012. However, since 2012, when DOACs were introduced as a treatment option for AF-related ischemic stroke prevention, the IR generally decreased or remained constant. In agreement with our results, Freixa-Pamias et al.18 found a significant decrease in the annual incidence of AF-related ischemic strokes, from 2013 to 2019, in a health area of a regional hospital in Barcelona (Spain). In parallel, DOAC use increased from 5.5% in 2013 to 46.8% in 2019 in that health area.18
Throughout the study period (2005-2018), the proportion of patients with comorbidities such as lipoprotein metabolism disorders, diabetes mellitus, and heart failure increased in patients with AF-related ischemic stroke. Other comorbidities, such as hypertension, ischemic heart disease, and cardiomyopathy remained steady. This finding suggests that the IR reduction from 2012 onward is not caused by a decrease in comorbidities. Rather, we observed a statistically significant association between DOAC uptake and the reduction in AF-related ischemic strokes in patients older than 65 years by Poisson regression analysis. In the general population, the largest IR decrease was found in the group aged 75 to 84 years. In patients older than 85 years, the IR still increased slightly from 2012 to 2018, most likely due to population aging. Nevertheless, this increase was lower than that during the pre-DOAC period. In summary, the IRR decreased in all age groups and both sexes in the post-DOAC period (2012-2018) compared with the pre-DOAC period (2005-2012). This IRR decrease in the post-DOAC period was also observed when the IRR was calculated using age-standardized crude IR.
Our analysis showed a reduction in the in-hospital mortality rate of AF-related ischemic stroke throughout the study period, which Poisson regression revealed to be significantly associated with DOAC uptake. However, the reduction in the in-hospital mortality rate was observed from 2010, 2 years before the introduction of DOACs in Spain. Therefore, this decrease cannot be attributed solely to greater DOAC use. Advances in the management of ischemic stroke over the last decade, including the use of fibrinolytic therapy, thromboendarterectomy, and the implementation of the “Stroke Code” are essential in the reduction of stroke mortality and length of hospital stay. Moreover, the RAE-MBS collects in-hospital deaths only. It does not collect out-of-hospital mortality, ie, deaths in patients after discharge. Therefore, the mortality rates reported in this study are underestimated and could be misleading. Additionally, it is not known whether patients were being treated with DOACs before their death, thereby casting doubt on the relationship between the mortality rate and DOAC use. In summary, the significant association observed between DOAC uptake and the reduction in mortality rate should be interpreted with caution.
Another important trend observed in this study was the reduction of the length of hospital stay from the beginning of the study to the end. The length of hospital stay was slightly lower in the post-DOAC than in the pre-DOAC period. However, and similar to the in-hospital mortality rate, the observed reduction in hospital stay cannot be attributed solely to the increase in DOAC use. Other factors may also play a role, such as the disuse of bridging therapy, the lower severity of the strokes, and the reduction in clinical follow-up. In addition, the reduction in length of hospital stay also corresponded to the general trend observed in Spain for any disease, given the improvement in care processes, treatments, and surgical procedures.
Strengths and weaknessesThe limitations of this study are primarily related to the data source and its ecologic design. Data obtained from the RAE-MBS was for hospital discharge only, and no information was available on patient follow-up or patient medication. Therefore, we were unable to adjust for comorbidities such as diabetes, hypertension, or heart failure to assess their impact on the association between DOAC uptake and the number of AF-related ischemic strokes. Furthermore, the number of patients identified who were under treatment with DOACs, the type of DOAC they were prescribed, and their medication adherence was unknown. In addition, the time of initiation of DOACs therapy was not measured and thus we were unable to assess whether patients with an AF-related stroke were already receiving DOAC treatment before the event or whether it was initiated after the event. Given the lack of control of the potential confounding factors, the association between DOAC uptake and AF-related ischemic stroke should be interpreted with caution. This is the main weakness of any ecological study, making it potentially susceptible to the “ecological fallacy”. We acknowledge that the association between DOAC uptake and the number of AF-related ischemic strokes observed in our study may differ from the causal association at an individual level, and that there are several confounding factors that could impact the observed association. In summary, our study describes an association between DOAC use and the incidence of AF-related ischemic stroke but cannot prove causality.
Another major limitation of this study is the switch of the ICD codes from ICD-9 to ICD-10 in 2016, which caused incorrect registration of some diagnoses and underestimation of the total number of diagnoses. Therefore, the data from 2016 and the comparison between the 2005 to 2015 and 2016 to 2018 datasets should be interpreted with caution. The potential bias introduced by the switch in codification is likely to be systematic and nondifferential. In our dataset, we observed a lower number of any type of stroke in 2016 than in 2015 and 2017 (table 1 and figure 1), according to the undercoding of diagnoses due to the ICD switch. However, this reduction did not affect the calculations of IRR (calculated using the IR from 2012 and 2018) or the results of the Poisson regression. In relation to the diagnostic codes, AF-related ischemic strokes were defined as those with “ischemic stroke” as the primary diagnosis and “AF” as a secondary diagnosis. Using the current study design, we were unable to identify the study population more precisely by differentiating between patients with ischemic stroke due to AF and those due to other embolic sources. Equally, our primary outcome of hospitalized AF-related ischemic stroke did not capture patients managed in the community or those who died before hospital admission.
While we acknowledge the limitations of this study, it also has several strengths. To our knowledge, this is the first nationwide population-based study conducted in Spain to evaluate the relationship between DOAC uptake and the epidemiology of AF-related ischemic stroke. Another strength of this study is the large and robust dataset used. Unlike clinical trials and small observational studies, this study contains data on the real-life conditions of 910 641 ischemic stroke patients and 233 935 patients with AF-related ischemic stroke, gathered over 14 years (2005-2018), which was able to successfully reflect the trends in patient health.
Our current findings corroborate previous studies reporting significant associations between increased DOAC uptake and a lower rate of AF-related stroke in England,8 Sweden,10 Germany,11 and Italy.12 However, the association is weaker in Spain than in these other European countries, likely due to DOAC underprescription. Although DOAC use has increased in Spain up to 42.22% in 2018, it is still far below the average in other European countries (average in Europe in 2018: 67.9%).19 DOAC prescription in Spain is subject to ex-ante approval, theoretically based on the recommendation of use defined in the latest Spanish Medicine Agency Therapeutic Positioning Report (TPR) of 2016,14 limiting their use mostly to second-line treatment after poor VKA control. Moreover, many physicians continue to prescribe VKA for patients who would be eligible for DOAC therapy based on the TPR requirements because of: a) the hurdle of obtain approval; b) the lack of direct access to analyze the INR20 and c) physicians’ perceptions of the rate of good control of VKA-treated patients.21 If DOAC use in Spain continues to increase to match that in other European countries, stronger associations may be found between DOAC uptake and the incidence of this type of stroke. An urgent update of the current Spanish guidelines to meet the recommendations of European and American guidelines is necessary. The inclusion of current favorable evidence of DOAC use for stroke prevention and the elimination or alleviation of prescribing restrictions, would likely improve patient prognosis and quality of life and decrease the costs and economic burden associated with AF-related stroke.
CONCLUSIONSThis is the first national population-based study conducted in Spain over 14 years that has evaluated the association between DOAC uptake and the epidemiological trend in AF-related ischemic stroke. While we analyzed only aggregate data and were unable to include possible confounding factors, we observed an association between an increase in DOAC use and a decline in AF-related ischemic stroke. These results are consistent with those of previously published European studies and suggest that higher DOAC uptake could enhance health outcomes in AF patients in Spain.
- -
The incidence and prevalence of AF, a major risk factor for stroke, have increased substantially in the past few years.
- -
Recent international guidelines encourage DOAC use for stroke prevention in AF patients.
- -
Studies from several European countries, such as Sweden, England, Germany, and Italy, have found associations between decreases in AF-related stroke rates and increased oral anticoagulant use.
- -
This is the first nationwide population-based study conducted in Spain using hospital discharge data from a robust database (RAE-MBS) over 14 years (2005-2018).
- -
The IR of AF-related ischemic stroke increased from 2005 to 2012. However, since 2012, when DOACs were introduced in Spain, the IR decreased or remained constant.
- -
The increase in DOAC uptake was significantly associated with a reduction in AF-related strokes in patients ≥ 65 years. However, this association is only a descriptive association and cannot demonstrate causality.
- -
These findings may help health care providers to encourage DOAC use to prevent AF-related ischemic strokes.
Bayer Hispania, S.L. has unconditionally funded the performance of this study with medical writing, editorial assistance, and analysis by Ingress-Health HWM GmbH.
AUTHORS’ CONTRIBUTIONSWe further attest that all the authors have substantially contributed to the material and/or intellectual content, data analysis, and interpretation of the data. All authors have participated in drafting, reviewing, and revising the manuscript and have approved its submission.
CONFLICTS OF INTERESTA. Llorac and M. Genís-Gironés are employees of Bayer Hispania S.L. B. Antolin-Fontes is an employee of Ingress-Health HWM GmbH. P. Rebollo was an employee of Ingress-Health Spain S.L. J. Díaz-Guzmán, A.I. Pérez Cabeza, I. Roldán-Rabadán, J. García-Alegría, R. Freixa-Pamias and C. Escobar-Cervantes report personal fees from Bayer, Boehringer Ingelheim, Daiichi-Sankyo and Bristol-Myers Squibb-Pfizer outside the submitted work.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2021.07.009