Keywords
INTRODUCTION
Occlusion of the left main coronary artery (LMCA) is occasionally found in angiographic studies following acute myocardial infarction (AMI) (1.5% of patients).1,2 When observed, the prognosis is bad unless substantial collateral circulation exists or reperfusion of the causal lesion is immediate.3-5 When neither option is available, most patients die from ventricular arrhythmias or cardiogenic shock.6
Primary angioplasty is the treatment of choice in ST-segment elevation AMI when the conditions pertaining permit intervention.4,7 Although guidelines indicate surgery as the treatment of choice in LMCA, percutaneous coronary interventions (PCIs) are also recommended in patients with cardiogenic shock following AMI. If surgery is impossible in an emergency and with patients at high surgical risk, PCI and mechanical support are considered the first option for treatment.8,9 Notwithstanding, few data are available on this situation and patient numbers in published series are low.2,10-22
A SHOCK study sub-analysis comparing surgical revascularization with PCI in patients with shock following AMI, found no short- and mid-term differences in mortality.17 However, a registry constructed in 2001 reported only 4.9% of patients were susceptible to surgery.18 Improved PCI techniques have now made this a feasible solution for the hemodynamic instability the situation entails.
The primary objective of the present study is to analyze a series of patients with LMCA disease and AMI undergoing emergency PCI and determine in-hospital mortality and its predictors, out-of-hospital mortality, and repeat revascularization. The secondary objective is to determine the short-term mortality associated with cardiogenic shock.
METHODS
Patients and Definitions
In a tertiary hospital, we enrolled 71 consecutive patients with severe unprotected LMCA lesion undergoing emergency procedures following AMI between January 1999 and February 2007. The principal indication was ST-segment elevation AMI (STEAMI) (42 patients, 59%), with primary percutaneous transluminal coronary angioplasty (PTCA) (33 patients) or following failed thrombolysis (6 patients). In 3 patients, STEAMI evolution was >24 h. Of 29 (41%) patients without evidence of ST-elevation on ECG, 20 were in cardiogenic shock. In 9 patients, LMCA was treated for persistent ischemia observed in coronary angiography studies.
We defined AMI as myocardial necrosis marker elevation (CK-MB and troponins) accompanied by electric changes and/or chest pain characteristic of ischemia.23 Emergency PCI was indicated for AMI with or without hemodynamic instability during the procedure, together with chest pain and persistent dynamic electric changes on ECG, with or without ST-elevation. Severe LMCA lesions were considered to cause signs and symptoms and produced angiographic stenosis >50%. In all patients, LMCA was unprotected and presented no permeable aortocoronary grafts to left anterior descending (LAD) or circumflex (Cx) arteries. We considered distal LMCA lesions bifurcated when they affected the LAD or Cx origins. We defined LMCA occlusion as absence of flow or TIMI flow I in LAD and Cx. We defined cardiogenic shock as systolic blood pressure <90 mm hg with signs of hypoperfusion or need for vasoactive drugs intra-aortic balloon counterpulsation iabc to maintain blood pressure p
Procedures were considered successful when they resolved angiographic stenosis, with anterograde TIMI III flow without death in the catheterization laboratory.
Events analyzed in the study were any-cause death and repeat revascularization.
Procedure
Initially, we administered 100 IU/kg unfractioned heparin, or 70 IU/kg when associated with glycoprotein (GP) IIb/IIIa inhibitors. Patients receiving conventional stents were administered double antiplatelet therapy for at least 1 month; those receiving drug-eluting stents (DES) had double therapy for at least 1 year. The strategy used in treating bifurcated lesions was left to the discretion of the operator, as was use of predilatation, prophylactic IABC, or intravascular ultrasound.
Drug-eluting stents were first used in our center in March 2003. In the present study we used Cypher (Cordis Corp. Johnson & Johnson), Taxus (Boston Scientific Corporation), and Endeavor (Medtronic) devices. Choice of stent type was at the discretion of the operator. Clinical follow-up was conducted in all patients through check-ups, reports and telephone calls.
Statistical Analysis
Continuous variables are shown as mean (SD). The Fisher exact test was used to analyze differences in percentages. We constructed univariate logistic regression models to analyze predictors of inhospital mortality. Multivariate logistic regression analysis of in-hospital mortality included the following variables: occluded LMCA, number of vessels, distal lesion, shock, and incomplete revascularization. We constructed Kaplan-Meier survival curves to determine post-discharge follow-up mortality. Statistical significance was defined as a bilateral value of P<.05 or confidence intervals (CI) not including the unit. Calculations were performed using SPSS 13.
RESULTS
Baseline patient characteristics are in Table 1 and angiographic characteristics in Table 2. Lesions affected the bifurcation in 72% of patients; in 30% the RCA was found to be occluded. Procedure characteristics are in Table 3. The most frequently employed technique was provisional stenting (85%). Almost half of the patients received a DES (47%) and in 3 patients implantation was impossible. Forty-seven (66%) patients presented cardiogenic shock. The procedure was successful in 83%.
In-hospital Mortality
Thirty-three (47%) patients died during hospitalization, 11 of these (16%) in the catheterization laboratory. All deaths were cardiac except a hemorrhagic complication in 1 patient with STEAMI. In-hospital mortality was independent of presence or absence of evidence of ST-segment elevation on ECG (48% vs 45%; P=.92) and cardiovascular risk factors. Principle predictors of in-hospital mortality are in Table 4. In univariate analysis, increased in-hospital mortality associated with need for IABC and orotracheal intubation, LMCA occlusion, and incomplete revascularization. Multivariate predictors that associated with greater in-hospital mortality were incomplete revascularization and shock.
Mortality and Revascularization in the Long-Term Follow-up
Following discharge, we conducted a median follow-up of 32 (1-88) months in 39 patients.
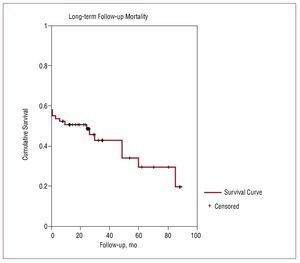
To 47% in-hospital mortality, we added 10.3% any-cause mortality at 1 year of out-of-hospital follow-up, and 28% mortality in the full follow-up (Figure). All deaths were cardiac except 3 (1 stroke, 1 kidney failure, and 1 undetermined death of a patient aged 93 years). Ten (14%) patients required repeat revascularization, 6 of these at the first 6 months. Four of these patients underwent repeat LMCA revascularization (1 patient underwent surgery, the other 3 had PCIs).
Figure 1. Long-term Kaplan-Meier survival curve
Patients With Cardiogenic Shock
Characteristics of patients with shock prior to or during the procedure are in Table 5. Diabetes mellitus, number of diseased vessels, and RCA occlusion associated with cardiogenic shock. The percentage of shock was similar in patients with and patients without ST-elevation. In-hospital mortality was greater in patients with shock. Follow-up of patients surviving to discharge revealed no differences in mortality between those with and those without cardiogenic shock (log rank test =0.4).
DISCUSSION
In this series of patients with AMI and severe unprotected LMCA disease, emergency PCI was a therapeutic option. However, this entails high in-hospital mortality, especially when associated with cardiogenic shock and when complete revascularization is not achieved.
Finding LMCA disease is not infrequent in coronary angiography. It is observed in 5% of patients with stable angina, 7% of patients with AMI, and 3%-5% of coronary angiographies for chest pain or heart failure.7
Cardiogenic shock and ST-elevation AMI are urgent conditions requiring immediate treatment.24 Few previous studies of emergency LMCA surgery exist and these enrolled selected patients. Given that emergency surgery is often unavailable and that these are high-risk patients, percutaneous treatment and mechanical support has been recommended.9
However, current data on emergency percutaneous treatment in this situation are scarce. The principle series of LMCA disease treated with angioplasty and coronary stents correspond to stable patients or series of patients, in which urgent procedures represent different, often small, percentages.9,16,25-28
In our series, the patients with acute unprotected LMCA disease are at high risk. They present a number of cardiovascular risk factors, prior AMI is frequent, and coronary angiography reveals extensive coronary disease in a high percentage of cases. Cardiogenic shock is the principal complication of emergency percutaneous treatment, which fundamentally distinguishes it from the procedure of choice.20,26
In-hospital Mortality
Of 71 patients receiving emergency treatment for LMCA disease, 47% died in hospital, 16% in the catheterization laboratory. Previous studies reported series with similar or greater in-hospital mortality (Marso et al,11 70%; Lee et al,14 44%) associated with a higher percentage of cardiogenic shock in the population studied. In our series, 66% had cardiogenic shock versus 92% reported by Marso et al.
Two facts not frequently mentioned in the literature are, first, that in-hospital mortality does not differ in patients with and patients without evidence of ST-elevation on ECG and, second, that a substantial number of patients present no evidence of ST-elevation on ECG (41%). This latter percentage is similar to that found in the ULTIMA study (9% with ST-depression; 9%, complete left bundle branch clock; and 12% with no changes on ECG).11
In univariate analysis, need for orotracheal intubation and IABC, cardiogenic shock and incomplete revascularization, number of diseased vessels, distal lesion, LMCA occlusion, and RCA occlusion all predicted increased mortality. In multivariate analysis, cardiogenic shock and incomplete revascularization associated with increased mortality. These data reaffirm the indication for complete revascularization in these patients, especially when cardiogenic shock persists.
Previous series describe RCA or left coronary artery occlusion, cardiogenic shock10,12,19 or need for IABC13 as predictors of bad prognosis. Other predictors have been absence of collateral circulation in RCA,12,19 use of inotropics,16 ST-elevation in aVR and aVL on ECG,19 and failed procedures.13
Distally located lesions affecting the bifurcation also associate with greater mortality.20 In our series, more than half of the patients presented bifurcated distal lesions which, in univariate analysis, associated with increased in-hospital mortality.
Patients With Cardiogenic Shock
Cardiogenic shock is especially frequent in patients who present diabetes with extensive disease, RCA occlusion or depressed left ventricular ejection fraction. It also occurs in patients with previous conserved ejection fraction. Incidence of cardiogenic shock was similar in patients with and without ST-elevation. Patients with shock had greater in-hospital mortality (62% vs 17%).
The in-hospital mortality previously described in patients with LMCA disease and cardiogenic shock is high, reaching >80% in several series.21,22
An earlier registry of 38 patients (73% with shock) found a seven-fold increase in in-hospital mortality in patients with shock.13
Mortality and Revascularization During Follow-up
At the first year follow-up, out-of-hospital mortality was 10%; at 32 months follow-up it was 28%. Repeat revascularization was required in 14%, and 6% underwent repeat LMCA revascularization. Previous studies reported incidence of mortality at the first year varied from absence of events in short series to 11% in larger series.2,12,14-16 In our study, survival curves were similar in patients surviving on admission, independently of the presence or absence of shock during the event, although this analysis may be limited due to the small sample size.
Limitations
When we began our registry, no randomized studies of DES in infarction had been published. Consequently, only 47% of patients received DES. Drug-eluting stents can reduce the restenosis rate during follow-up. We conducted no systematic angiographic follow-up, so the restenosis rate may be an underestimate due to asymptomatic patients. The limited number of participants in our study produces extreme estimates with wide-ranging CIs. Reinfarctions were not analyzed during follow-up after discharge.
CONCLUSIONS
In our series, with a high number of patients with LMCA disease and AMI, percutaneous intervention is a therapeutic option. However, inhospital mortality continues to be high even in AMI without evidence of ST-segment elevation on ECG, especially if associated with cardiogenic shock and when complete revascularization is not achieved.
ABBREVIATIONS
AMI: acute myocardial infarction
DES: drug-eluting stent
LMCA: left main coronary artery
PCI: percutaneous coronary intervention
Correspondence: Dr. J.A. Hurtado Martínez.
Almudena, 1, 12.º E. 30005 Murcia. España.
E-mail: josehurtadomartinez@yahoo.is
Received October 4, 2008.
Accepted for publication June 10, 2009.