To the Editor:
With great interest, we have read the article by Bayes de Luna1 about the new electrocardiographic nomenclature for Q-wave myocardial infarctions. The article is very interesting in as much as it provides an electrocardiographic correlation with the magnetic resonance image, verified with gadolinium contrast. The eternal dilemma about the nomenclature of different cardiologic segments based on surface electrocardiograms is not exclusive to the world of ischemic cardiopathies. Cosío et al2 proposed new terminology to designate the localization of the accessory pathways as a function of their spatial anatomic location using new technologies, like magnetic resonance.
This brings us back to the complexity of the electrocardiogram—a basic diagnostic tool of incalculable value—which are simple to obtain but still present numerous enigmas in their interpretation. As Bayés de Luna says,1 in the light of experience, "don't believe in immovable, lifelong dogmas." So, interpreting electrocardiograms is subject to innumerable factors of spatial resolution: cardiac obliquity, verticalization, or horizontalization of the central axis, thoracic conformation, precise electrode positioning, etc. Occasionally, even in patients with apparently normal ECGs, we discover a Brugada type I pattern by positioning the electrodes in the second intercostal space.3
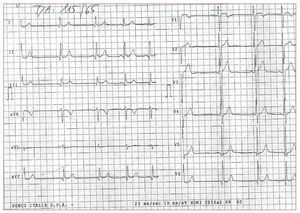
In Figure 1, we present an ECG that, analyzed in detail, is very similar to the one presented at the end of Bayés de Luna's article: predominant qR in leads on the limbs, and V5, V6, together with a marked RS morphology in V1 (90 ms in duration) with ST and negative T elevation in the same lead (as in the ECG presented by Bayés de Luna). A noteworthy difference (apart from the fact that our ECG presents a sinus arrhythmia), is that the ECG presented by Bayés de Luna portrays an rSr' pattern and ST rectification in III, which in principle would not be justified by ischemia given that, as the author explains, the AMI in the ECG under study is "lateral, without compromising the inferior wall" (as is borne out by the sagittal magnetic resonance image). Our ECG corresponds to a man aged 24 years, asymptomatic and without cardiovascular risk factors, referred to our cardiology clinic from primary care for respiratory sinus arrhythmia. Despite the curious V1 morphology, the patient was slightly built, 1.79 m tall, 80 kg in weight, and presented no pectus excavatumor pectus carinatum-type chest deformities. Electrodes were correctly positioned, the chest x-ray showed no obvious cardiac apex deviation, and echocardiograms were normal (including wall thickening and segment contractility). Logically, our patient was not suspected of having transmural "posterior" (or lateral, in the new terminology) AMI.
Figure 1
While we agree with the proposed new terminology for Q-wave AMI,4 as it seems a better reflection of the reality, we would point out that, although surface ECG continues to be the fundamental diagnostic tool, it stills holds undiscovered secrets.