Keywords
INTRODUCTION
Since 1968, when Favaloro1 began revascularization surgery via aortocoronary bypass grafting, technical improvements during intervention and postoperative care have made it possible to obtain positive results in the short- and long-term.2
As the life expectancy of such patients has increased, the occurrence of lesions and vein graft degeneration has become one of the main restrictions to this revascularization technique.3 In particular, since the introduction of the stent, percutaneous coronary intervention (PCI) has become the treatment of choice for patients with saphenous vein graft lesions to prevent the risk of further revascularization surgery.3,4 However, angioplasty in vein grafts is associated with worse outcomes than in native arteries. Balloon angioplasty has a lower procedural success rate and a high incidence of restenosis.5 Although the use of stents has improved these outcomes,6 it is associated with a higher incidence of acute complications than in native arteries. The incidence of distal embolization and periprocedural myocardial infarction is still high due to the friable material in the vein graft lesions.7-12
Since 1998, when Figulla et al13 described their implantation technique without predilatation (direct stenting [DS]), this procedure has undergone gradual development and the type of lesions treated has increased.14 Descriptions of its use in lesions located in saphenous vein grafts is limited.15,16 The technique could be associated with a lower degree of distal embolization and improved final slow flow, because initial aggression to the vessel due to predilatation before stenting is avoided.
The purpose of this study is to compare in-hospital and long-term outcomes of direct stenting and stenting with predilatation in saphenous vein grafts, and to identify the predictors of mortality.
PATIENTS AND METHODS
Lesions and Patients
All the patients who had been treated with stenting between 1 September 1998 and 31 March 2003 for at least 1 lesion located in saphenous vein grafts were selected from the intervention registry of the 2 hospitals participating in this study. The patients were divided into 2 groups depending on the stenting technique used, i.e., with and without predilatation. Patients with lesions treated with both techniques were excluded from the study. The patients were included in each group according to the initial procedure, such that if new revascularization was required and the other technique was used, they stayed in the original group. Demographic and procedural characteristics were obtained from the hospital registries where they had been prospectively introduced. All baseline angiographies and those done after the intervention were analyzed blindly regarding clinical events by 2 experienced interventional cardiologists. The quantitative analysis was done offline with a previously validated edge detection system (CAAS II, V4.1.1. Pie Medical Imaging Maastricht, The Netherlands) in the projection that revealed more severity with the contrast-filled catheter as the reference.
Procedure
Indications for revascularization included all the manifestations of coronary disease, including primary angioplasty. All the stents were premounted on a monorail system. No restrictions were placed on the type of stent used, the catheter guides (6 or 7 Fr), or the use of glycoprotein IIb/IIIa inhibitors. Decisions regarding the stenting technique, the material selected, and the adjuvant drugs was left to the discretion of the interventional cardiologist responsible for each case. Following the protocol of both centers, heparin was administered intravenously to obtain an activated clotting time of 300 s, or of 250 s when glycoprotein IIb/IIIa inhibitors were used. When a residual stenosis >20% persisted which was resistant to high-pressure inflation with the same balloon, additional dilatation with non-compliant balloons of the same or greater diameter was done following the usual protocol of both centers. All dissections were dealt with by implanting a new stent.
All the patients had an electrocardiogram (ECG) before and after the intervention to detect possible new ischemic events. In addition, creatine kinase (CK) and its isoenzyme MB (CK-MB) were measured at 8 h and 24 h after the procedure, following the centers' protocol.
Definitions
Primary Success of Direct Stenting
Direct stenting without predilatation with balloon or preparation via atherectomy.
Procedural Success
Obtaining a residual stenosis <20% and TIMI 3 flow in the target vessel in the absence of worse complications such as death or myocardial infarction with the appearance of new Q waves.
Distal Embolization
Abrupt interruption of filling in 1 of the peripheral branches of the target vessel, distal to the lesion, following the procedure (thrombotic or atheromatous origin).
Calcification
- Mild: single or multiple image of well-defined calcium density, nonlinear, located on the target lesion.
- Moderate: image of linear calcium density, located on one side of the target lesion and non-visible on a fluoroscopic image snapshot.
- Severe: image of linear calcium density, located on both sides of the target lesion and visible with fluoroscopy even on a snapshot image.
Tortuosity
- Moderate: 2 bends >75 degrees or 1 bend 90 degrees proximal to the target lesion.
- Severe: 2 bends >90° proximal to the target lesion.
Thrombus
Radiopaque filling defect visible in multiple projections surrounded by contrast agent.
Myocardial Infarction
Elevated CK approximately twice the normal value.
Follow-up
This was done via personal structured interviews at 6 months and at the end of the first year of follow-up. A telephone call completed the check-up period. In the case of dead patients, the information to determine the cause of death and the events occurring before this was obtained from family members, the referring physicians and their medical records. Death due to non-cardiac causes was not recorded as a follow-up event; such patients were considered to be living patients who had completed follow-up on the date of the non-cardiac death.
Statistical Analysis
Continuous variables are expressed as mean ± standard deviation (SD) and categorical ones as absolute value and percentage. Student's t test was used to compare means and chi-squared test to compare ratios. All values were evaluated bilaterally and P-values ≤.05 were considered statistically significant. The Kaplan-Meier method was used for survival analysis and new revascularization in the treated vessel and a log-rank test to compare both groups. Cox's regression analysis was used for the variables that could be clinically associated with a worse prognosis during follow-up to determine long-term independent predictors of cardiac mortality in the global series. The data were analyzed with SPSS version 12.0 for Windows.
RESULTS
During the study period, 137 lesions were analyzed in 117 patients of which 71 (60%) patients and 83 lesions (60%) belonged to the DS group. No significant differences were found between the 2 groups regarding age, coronary risk factors, previous myocardial infarction, previous angioplasty, ejection fraction, and the age of the graft. There were more women and less use of abciximab in the DS group. Patient characteristics are shown in Table 1.
The angiographic characteristics of the lesions are shown in Table 2. There were no major angiographic restrictions to the use of DS (calcification, tortuosity, and angulation). Lesions in the PD group had more stenosis, smaller minimum luminal diameter, smaller reference diameter, and a trend toward less TIMI grade 3 flow prior to PCI. All lesions due to restenosis were treated with DS.
No differences were found between the 2 groups (Table 3) regarding the success of the procedure. Only 1 patient died before discharge (DS group). This occurred 4 days after the intervention due to an initially unnoticed retroperitoneal hemorrhage. The other cases in which the procedure was unsuccessful (1 in the DS group and 4 in the PD group) were due to a final TIMI flow <3 despite using adenosine and intracoronary nitroprusside. Significant differences were found regarding distal embolization which were more frequent in the PD group. There was a trend toward a greater frequency of non-Q wave myocardial infarction in the PD group, but this did not reach statistical significance. Outcomes by lesion are shown in Table 4.
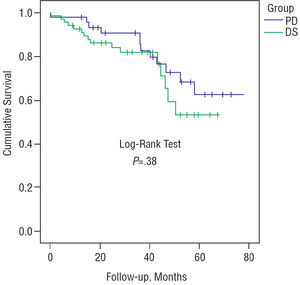
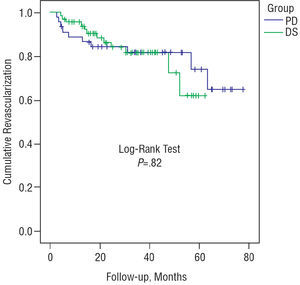
Median follow-up time was 36.1 months (mean, 35.1±19.3). Clinical follow-up was successfully completed in 99% of the patients. Three patients from each group died from non-cardiac causes (2 strokes, 3 malignant tumors, and 1 aneurysm of the abdominal aorta). Fifteen patients from the DS group died from cardiac causes: 1 after heart transplantation, 2 due to cardiogenic shock in hospital, and the rest from myocardial infarction and/or sudden death at home. Eleven patients in the PD group died from cardiac causes: 1 from cardiogenic shock in hospital and the rest also from myocardial infarction and/or sudden death at home. Global survival in the series at 12, 24, 36, 48, and 60 months was 94±2%, 87±3%, 82±17%, 67±8%, and 58±7%, respectively. The data are shown in Table 5 and Figure 1 for both groups. The global revascularization rate for the target lesion was 14% and 20.5% for the treated vessel; in an additional 6% the vessel was occluded and revascularization was not carried out later. There were no differences between the 2 groups regarding any of the 3 aspects mentioned (Figure 2).
Figure 1. Long-term survival.
Figure 2. New revascularization of the treated vessel.
The Cox model was used for the variables that could clinically be associated with a worse long-term prognosis. Ejection fraction (numerical) and smoking habit at the time of PCI were the only independent predictors, whereas procedure-related myocardial infarction was an effect modifying variable in the final model (Table 6).
DISCUSSION
The outcomes of direct stenting and stenting with predilatation in saphenous vein grafts were compared in this study. The most relevant findings are that the distal embolization rate was significantly higher in the predilatation group with a trend toward a greater frequency of periprocedural myocardial infarction. In addition, although the immediate results were satisfactory in both groups, the long-term prognosis was unfavorable in a high percentage of cases. There were no differences between the 2 groups regarding survival and revascularization rates during follow-up. Ejection fraction and smoking habit at the time of PCI were predictors of cardiac mortality.
Immediate Results
Stents are the most effective devices in the treatment of ischemic heart disease with PCI in vein graft lesions.6,8,9,11,17,18 Thus, previous studies have shown that balloon angioplasty is not a good choice in such interventions due to the high rate of restenosis,19,20,21 and that the use of new devices has not led to significant progress.22-26 The lesions located in saphenous vein grafts have different characteristics to those in the native vessels with greater cellular and less fibrotic components, more necrotic debris, cholesterol, thrombi, and foamy cells.10,19 Thus, one of the greatest restrictions to stent implantation with predilatation is the risk of distal embolization, with a high incidence of periprocedural myocardial infarction.7-12
In our series we found a significant difference in the direct stenting group with less distal embolization associated with a trend toward a lower incidence of periprocedural myocardial infarction. It is likely that with a larger sample significant differences would have been found in myocardial infarction rates. Although all the myocardial infarctions recorded were non-transmural, the relationship between elevated enzymes and mortality is well known.26-29 Despite the fact that the multivariate analysis carried out in our series did not reach statistical significance regarding periprocedural myocardial infarction, the trend was also verified, which means that with a larger number of patients it would probably have functioned as an independent predictor of long-term mortality. The advantage of direct stenting compared to stenting with predilatation in the treatment of lesions with thrombus has already been demonstrated in previous series.30-34 Other embolization factors described in previous series include the extent of the disease, the presence of ulcers and plaque volume.7
Although this was not a randomized study, and given that the decision regarding which technique to use was exclusively at the discretion of the interventional cardiologist, the percentage of lesions treated with DS (60%) is clearly higher than the rates in native vessels14 with DS being achieved in all the lesions. This could be due to the absence of those characteristics that in native vessels cause implantation failure, such as calcification, tortuosity, or angulation.13,35-45
The need to use multiple stents per lesion was higher than in the published series,36,37,43,45,46 basically due to a greater percentage of cases with coverage deficits caused by the different composition of the lesions, e.g., more friable content leading to displacement toward the lesion's edges. Finally, the need for postdilatation and dissection remained within the limits published in a series of DS. The probability of losing the stent is very low. According to previous studies, such losses especially occur when removing it with the guide catheter following implantation failure; similarly, in the absence of primary implantation failure, the chances of losing it is strongly reduced.39,47,48
Our series is similar to the direct stenting series described by Leborgne et al,15 regarding graft age, the percentage of thrombus, abciximab use, vessel diameter, the success of the procedure, distal embolization events, and absence of reflux. The only difference was a higher percentage of periprocedural myocardial infarction, which could be due to the different, and more aggressive, approach to treating the lesion s by using a larger balloon/artery radius.
Long-Term Survival
Cardiac death is the leading cause of mortality after revascularization surgery with ranges between 41% and 63%, according to the different series published.49,50 The results of our series are consistent with the long-term survival analysis studies in patients treated with PCI in saphenous vein grafts. These have yielded satisfactory immediate results but less favorable final outcomes.8,10,51
Thus, PCI in patients with previous surgery should be regarded as a palliative procedure.17 In fact some authors recommend carrying out PCI in native vessels whenever possible even when there is complete obstruction or to consider the possibility of new revascularization surgery.52 In previous series, the factors that had an effect on long-term survival were ejection fraction,17,19,22 age,3,19 extent of the vascular disease,17 full revascularization,17 diabetes,3,52 CK elevation after the intervention,53 and restenosis rate.17,19 In our series, only the ejection fraction (numerical) and smoking habit at the time of PCI were associated with greater long-term mortality; no relation to restenosis or graft occlusion was found. No differences were found in long-term mortality between the two series, in contrast to the series of Leborgne et al,15 where they reported a significant difference in mortality at 12 months (5.3% with DS and 10.4% with PD; P=.045). This series and ours are the only 2 that to date have analyzed mortality regarding PCI in saphenous vein grafts, since the studies with sufficient statistical power designed to compare mortality between DS and PD dealt with native vessels, and none of them found differences in mortality.35,40,42
Revascularization of the Treated Vessel
One of the most important restrictions to PCI in saphenous vein grafts is the need for new revascularization in the treated vessel. The factors reported as having an influence are residual stenosis,54,55 disease progression,17,54 dyslipidemia,55 ostial location,9,18,22 and restenotic lesion.22 To date, the stent is the only device which has reduced this rate. The pattern of new revascularization is different in native vessels and in vein grafts. Thus, whereas in the former it occurs around the 6th month and only occasionally after the ninth, in vein grafts it can take place later. In a series published by Douglas,56 32% occurred in the first 6 months, but it rose to 43%, 61%, and 64% after 6-12 months, 1-5 years, and 5 years, respectively. In another series by Hong et al,57 the greatest increase in revascularization occurred up to the 8th month, but given that later cases took place it is advisable to continue follow-up for at least 1 year. In our series, 70% of new revascularization occurred between the 11th and 19th month. The reason for this late pattern, according to some authors, could be the larger reference diameter, which meant more time would be required to reach a minimum luminal diameter sufficiently small to yield clinical findings.57 Cases of earlier restenosis have been associated with ostial lesions and the smaller reference diameter.55 In this case, and unlike the findings reported by Leborgne et al,15 no differences were found in revascularization rates between the 2 groups. This also is in line with most studies that compare the restenosis rate between direct stenting and stenting with predilatation in native lesions.35,40,42
Limitations
This was a retrospective study and therefore is subject to the limitations of this type of design. Thus, it was not possible to determine the myocardial infarction rate during follow-up. On the other hand, the decision regarding the treatment strategy, and thus allocation to one group or the other, depended exclusively on the interventional cardiologist responsible for the procedure. There was an imbalance regarding sex, the diameter of the treated vessels, and abciximab use between the 2 groups due to the lack of randomization.
CONCLUSIONS
Stent implantation without predilatation in saphenous vein graft lesions makes it possible to reduce the risk of distal embolization and achieves a lower incidence of periprocedural myocardial infarction compared to the conventional technique. The immediate outcome is satisfactory with both techniques but long-term survival is less favorable. There were no differences between the 2 groups regarding mortality and revascularization. Ejection fraction and smoking habit were the main predictors of survival during follow-up.
I. Lozano and R. López-Palop declare themselves consultants to Boston Scientific, SCIMAB group.
Correspondence: Dr. I. Lozano.
Servicio de Cardiología. Hospital Universitario Central de Asturias.
Instituto, 7, 2.o derecha. 33201 Oviedo. Asturias. España.
E-mail: IMLML9@hotmail.com