The EXCEL1 and NOBLE2 clinical trials have the largest number of patients and longest follow-up among studies comparing the safety and efficacy of coronary artery bypass grafting (CABG) vs percutaneous coronary intervention (PCI) and stent placement for left main coronary artery (LMCA) revascularization. Until the publication of their results in 2019,1,2 the evidence provided by comparisons of these techniques came from small clinical trials or subgroup analyses from the SYNTAX3 study.
EXCEL and NOBLE have had a huge impact on the cardiovascular scientific community. As an example, the level of evidence conferred on the CABG and PCI recommendations for left main disease in the myocardial revascularization clinical guidelines of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (ESC/EACTS) of 20184 were changed after the publication of the 3-year results of EXCEL.5 However, conflicting interpretations of the EXCEL findings and suspicions regarding manipulation of the data have resulted in public confrontations between the study authors themselves, and between the authors and several cardiac surgery scientific societies. This has ultimately led the EACTS to withdraw its support of the LMCA revascularization recommendations in the latest guidelines6 and The New England Journal of Medicine to conduct a review of the trial.7
This Editorial delves into the details of the NOBLE and EXCEL trials in an attempt to understand their strengths and weaknesses. Our aim is to help readers draw conclusions as unbiased as possible and useful for daily clinical practice in the treatment of patients with LMCA disease and chronic stable angina or non–ST-segment elevation acute coronary syndromes.
THE TWO STUDIES AT A GLANCEEXCEL1 included 1905 patients, 957 in the CABG arm and 948 in the PCI arm with everolimus-eluting stents. At 5 years, the researchers found no differences in the incidence of the composite primary endpoint (death, stroke, or infarction) between surgery (19.2%) and PCI with stent placement (22%; P=.13). The NOBLE trial included 603 patients undergoing CABG and 598 undergoing PCI with biolimus-eluting stents. In this case, there was a higher incidence of the composite endpoint—death, spontaneous infarction, coronary reintervention, or stroke—in the PCI group at 5 years (28% vs 19%; hazard ratio [HR], 1.58; 95% confidence interval [95%CI], 1.24-2.00). That is to say, the clinical outcomes following PCI were inferior.
DESIGN AND PATIENT SELECTIONNOBLE and EXCEL were both designed as 1:1 noninferiority studies to assess the safety and efficacy of PCI vs CABG in LMCA revascularization. The NOBLE trial had no private funding, whereas EXCEL was funded by Abbott Vascular, the manufacturer of the stent used in the study (XIENCE, Abbott Vascular; United States). This involvement of the company was precisely what led to intense controversy and even a journalistic investigation when it became known that one of the study authors held a position within Abbott Vascular, at least 13 others received payments from the company, and an institution dependent on the principal investigator was being financed by Abbott.8
The inclusion and exclusion criteria were similar in the 2 trials. The percentage of patients treated per protocol was high in both studies (NOBLE, 96.2% [1155/1201]; EXCEL, 95.2% [1812/1905]), and there were few crossovers and withdrawals. In both clinical trials, enrollment was slower than expected, which made it necessary to reduce the estimated sample from 2600 to 1905 in EXCEL and to extend follow-up for the primary endpoint analysis in both studies. The sample included relatively young patients (around 66 years) and mainly men (75%-80%) in both cases. The mean SYNTAX score was similar (22.4 in NOBLE and 20.6 in EXCEL), as well as the mean number of coronary grafts in surgically treated branches and the number and length of stents in branches treated percutaneously. The use of second-generation stents was slightly higher in EXCEL (99% vs 92.3%), whereas NOBLE patients were operated more often using on-pump circulation (84.4% vs 70.6%) and underwent fewer revascularizations using bilateral internal mammary artery grafts (28.8% vs 7.9%).
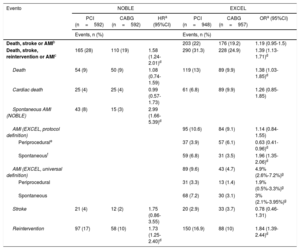
INTERPRETATION OF THE EVENTSThe definition of the composite primary endpoint in NOBLE (death, spontaneous infarction, or coronary reintervention) has been criticized for favoring the CABG arm. It excludes periprocedural infarction, known to be more frequent after CABG, and includes coronary reintervention, which is much more common at mid-term in PCI.9 Based on this definition, the incidence of the primary endpoint was much higher in the PCI arm (table 1), due to a higher incidence of both myocardial infarction and coronary reintervention.
Comparison of the combined events occurring in the EXCEL and NOBLE studies
| Evento | NOBLE | EXCEL | ||||
|---|---|---|---|---|---|---|
| PCI (n=592) | CABG (n=592) | HRa (95%CI) | PCI (n=948) | CABG (n=957) | ORa (95%CI) | |
| Events, n (%) | Events, n (%) | |||||
| Death, stroke or AMIb | 203 (22) | 176 (19.2) | 1.19 (0.95-1.5) | |||
| Death, stroke, reintervention or AMIc | 165 (28) | 110 (19) | 1.58 (1.24-2.01)d | 290 (31.3) | 228 (24.9) | 1.39 (1.13-1.71)d |
| Death | 54 (9) | 50 (9) | 1.08 (0.74-1.59) | 119 (13) | 89 (9.9) | 1.38 (1.03-1.85)d |
| Cardiac death | 25 (4) | 25 (4) | 0.99 (0.57-1.73) | 61 (6.8) | 89 (9.9) | 1.26 (0.85-1.85) |
| Spontaneous AMI (NOBLE) | 43 (8) | 15 (3) | 2.99 (1.66-5.39)d | |||
| AMI (EXCEL, protocol definition) | 95 (10.6) | 84 (9.1) | 1.14 (0.84-1.55) | |||
| Periprocedurale | 37 (3.9) | 57 (6.1) | 0.63 (0.41-0.96)d | |||
| Spontaneousf | 59 (6.8) | 31 (3.5) | 1.96 (1.35-2.06)d | |||
| AMI (EXCEL, universal definition) | 89 (9.6) | 43 (4.7) | 4.9% (2.6%-7.2%)g | |||
| Periprocedural | 31 (3.3) | 13 (1.4) | 1.9% (0.5%-3.3%)g | |||
| Spontaneous | 68 (7.2) | 30 (3.1) | 3% (2.1%-3.95%)g | |||
| Stroke | 21 (4) | 12 (2) | 1.75 (0.86-3.55) | 20 (2.9) | 33 (3.7) | 0.78 (0.46-1.31) |
| Reintervention | 97 (17) | 58 (10) | 1.73 (1.25-2.40)d | 150 (16.9) | 88 (10) | 1.84 (1.39-2.44)d |
CABG, coronary artery bypass grafting; HR, hazard ratio; AMI, acute myocardial infarction; PCI, percutaneous coronary intervention; OR, odds ratio
The NOBLE study expressed risk associations by the HR and EXCEL by the OR, as the principle of proportionality of risks was not met.
Definition of periprocedural AMI in the EXCEL5 study: a) creatine kinase MB isoenzyme (CK-MB) ≥ 10 times the upper limit of normal, or b) CK-MB ≥ 5 times the upper limit of normal together with some of the following signs of ischemia: b1) compatible electrocardiographic changes; b2) angiographic evidence of occlusion or significant de novo stenosis of a graft/stent or native vessel; b3) imaging evidence of new loss of myocardial viability or new regional wall motion abnormality.
Spontaneous AMI (> 72hours after PCI or CABG): detection of CK-MB or troponin change plus evidence of ischemia (see note e in this same footnote).5
In contrast, the design of the primary endpoint in EXCEL favored the PCI arm by excluding coronary reintervention. Furthermore, the conclusion that PCI was not inferior to CABG was mainly due to the definition of myocardial infarction, which increased the periprocedural acute myocardial infarction (AMI) rate in the CABG arm by 37% (table 1). The definition of periprocedural AMI in EXCEL was modified along successive versions of the research protocol,8 and was not established until 6 weeks before publication of the 3-year results,5 which certainly contravenes the CONSORT recommendations.
The most commonly accepted description of myocardial infarction corresponds to the universal definition10 and not that included in the final report of the 5-year EXCEL results, which was based on creatine kinase MB isoenzyme (CK-MB) thresholds. These were identical for CABG and PCI, and no other concurrent criteria were required, such as electrical or echocardiographic changes, or angiographic evidence of new coronary disease. The authors initially refused to report the incidence of periprocedural AMI according to the third universal definition, arguing that electrocardiograms are not routinely performed after PCI and therefore, the incidence could be biased, and that the data had not been prospectively recorded.8,11
Faced with insistent requests from numerous authors and a journalistic investigation by the BBC, the authors backpeddled and made public the myocardial infarction rates based on the third universal definition (table 1).6,7,10,11 Following this change, the incidence of the event was much higher in the PCI group (9.6% vs 4.7%, a difference of 4.9%; 95%CI, 2.6-7.2). Unfortunately, the authors did not provide information on the incidence of the primary endpoint once the description in the previous one had been corrected.
Two recent reports analyzed the impact of various infarction definitions on long-term mortality in the EXCEL trial and the SYNTAXES12 study. The main conclusion was that periprocedural AMI exclusively defined using biomarker criteria has an effect on long-term mortality after PCI, but not after surgery. However, the definition of infarction based on biomarkers plus electrical changes does have an impact on long-term mortality after CABG.
One finding of the EXCEL trial that deserves special attention is that 5-year all-cause mortality was higher in the PCI arm (OR, 1.38; 95%CI, 1.03-1.85).1 The authors explained this difference by arguing that it was a spurious result stemming from statistical chance (it was a secondary endpoint) and that it could hardly be biologically plausible because no differences were detected in cardiovascular mortality (OR, 1.26; 95%CI, 0.85-1.85). However, this explanation is clearly biased and deserves a somewhat deeper reflection: a) death is the only event that cannot be relativized or biased by a definition; b) it is the most serious hard event possible; c) assignment of the cause of death was not blinded in EXCEL, hence there is a risk of classification bias; and d) denying the biological plausibility that all-cause mortality was higher in the PCI arm because noncardiovascular causes were not acknowledged, is the same as denying that any such cause might exist. A recent meta-analysis of 23 clinical trials reported that PCI led to an increase in both cardiovascular mortality (incidence ratio, 1.24; 95%CI, 1.05-1.45) and noncardiovascular mortality (incidence ratio, 1.19; 95%CI, 1.00-1.41) relative to CABG. Therefore, it does not make much sense to expatiate on the causes of death when comparing mortality rates according to the type of revascularization.13
In summary, the EXCEL analysis leads us to reject or, at least, question its conclusions, considering that the all-cause mortality and risk of infarction were higher in the group undergoing PCI and the incidence of the primary endpoint according to standarized definitions was never provided.
In the light of these considerations, the current revascularization recommendations in the 2018 EACTS/ESC clinical practice guidelines are open to doubt, as they defend percutaneous revascularization with the same strength as surgical revascularization for patients with a low SYNTAX score (I A), and as an alternative (II A) in patients with intermediate risk. As mentioned above, EACTS has withdrawn its support for the guideline recommendations on left main revascularization pending an independent investigation of EXCEL.6
After EXCEL and NOBLE, 2 aggregate-data meta-analyses were published, incoporating data from these 2 trials, from the subgroup analyses of the SYNTAX study, and from 2 small clinical trials.14,15 The meta-analysis by Ahmad et al.14 found no difference at 6 years in mortality (relative risk [RR]=1.03; 95%CI, 0.81-1.32), stroke (RR=0.74; 95%CI, 0.35-1.50), or AMI (RR=1.22; 95%CI, 0.96-1.56). Unplanned revascularization was more frequent after PCI (RR=1.73; 95%CI, 1.49-2.02). Zhang et al.15 reported no significant differences in the event death, stroke or infarction in patients with a low or intermediate SYNTAX score (HR, 1.20; 95%CI, 0.85-1.70), and a higher incidence following PCI in those with a high SYNTAX score (HR, 1.64; 95%CI, 1.20-2.24). These 2 meta-analyses analyzed events defined differently (such as AMI), they used aggregate data (not patients), included different types of stents and surgical strategies, and combined clinical trials with trial subgroup analyses. Thus, the comparisons contained markedly heterogeneous elements, and once again, the conclusions should be interpreted with caution.
CONCLUSIONSAt this point in time, decades after the first comparisons between PCI and CABG, surgery continues to be a superior option in certain clinical and anatomic situations. As PCI has undergone development, so has CABG. In particular, the outcomes of this surgery have greatly improved for the treatment of LMCA disease because of the more widespread use of arterial grafts, aortic no-touch techniques, and complete revascularizations.1,2
It is difficult to generalize the conclusions of NOBEL and EXCEL to all patients with LMCA disease. Both trials have characteristics that make their external validity low and, as has been discussed, their results should be interpreted with caution. For this reason treatment decisions for each individual patient should be made by a multidisciplinary heart team headed by experts, which adds the experience in each center to the evidence from these studies and includes an analysis of the local results at short-, mid-, and and long-term.16 However, all told and according to the results of these 2 clinical trials, surgery should be the first option to consider when contemplating LMCA revascularization.
CONFLICTS OF INTERESTThe authors have no conflicts of interests.