A cross-sectional study of cardiac resynchronization therapy use in Spain was performed to analyze problems with indications, implantation, and patient follow-up.
MethodsSpanish cardiac resynchronization therapy implanter centers were identified, then the department members were surveyed and the data were recorded by each implantation team.
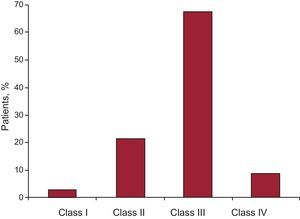
ResultsEighty-eight implanter centers were identified; of these, 85 (96.6%) answered the survey. A total of 2147 device implantations were reported, comprising 85.6% of the overall number of 2518 implantations estimated by the European Confederation of Medical Suppliers Associations for the same period. The reported implantation rate was 46 per million inhabitants versus an estimated implantation rate of 51 per million (European average, 131). Cardiac resynchronization therapy devices accounted for 84% of implantations, and upgrades to previously implanted devices, 16%. The majority of cardiac resynchronization therapy devices were implanted in men (70.7%). The mean age was 68 (12) years, and the mean left ventricular ejection fraction was 26.4% (5%). Most patients (67%) were in New York Heart Association functional class III. The group of patients for whom cardiac resynchronization therapy was indicated according to the latest update of the guidelines was significant: 17.3% among New York Heart Association class II patients and more than 21.6% among patients with atrial fibrillation. In all, electrophysiologists accounted for 73.8% of implanters, followed by surgeons, accounting for 21.4%.
ConclusionsThe latest update of the guidelines is being progressively implemented in Spain, according to data obtained in patients in New York Heart Association class II or with atrial fibrillation. Nevertheless, the number of cardiac resynchronization therapy device implants is still well below the European average.
Keywords
Cardiac resynchronization therapy (CRT) has proven to be effective for the treatment of patients with acute heart failure and wide QRS complex.1, 2, 3, 4 This article analyzes various aspects such as activity, as well as variables such as adherence to the latest update of the clinical guidelines, problems with their implementation, patient selection, CRT implantation and techniques, optimization, and follow-up data on patients with CRT therapy. We also report on CRT implants carried out between September 2010 (date of the latest guidelines) and September 2011. Most hospitals performing CRT implantation in Spain (appendix) participated in the survey. These data allowed us to compare and analyze differences between Spain and other European countries and to identify differences among the autonomous communities.
MethodsAll data were obtained using a 59-question survey. Fieldwork was undertaken to identify all hospitals in each autonomous community that performed CRT device implantation. The fieldwork included all public and private hospitals that volunteered to participate and had an organized system for CRT implantation; hospitals with only sporadic activity were not included. A member from each implanter team voluntarily completed the survey, and the information was introduced into a specially created database. A contract statistician handled the anonymous statistical analysis of the data. The authors of this article were responsible for analyzing the data or reviewing the article and are responsible for its publication.
The population data used to calculate rates per million inhabitants for both Spain and the Spanish autonomous communities were obtained from estimations at 1 January 2011 by the Spanish National Institute of Statistics (Instituto Nacional de Estadística).5 For European populations, the US Census Bureau6 was used. To estimate data representativity, we calculated the percentage of CRT devices shipped compared with the total number of devices implanted in Spain during the same time period. This number is based on data reported by CRT marketers to the European Confederation of Medical Suppliers Associations (EUCOMED),7 with small variations due to the different methods and times of quantitation. The percentages for each of the variables analyzed were calculated from the total number of implanters reporting information on the variable.
Statistical AnalysisThe continuous variables are expressed as no., mean (SD) (minimum-maximum), and median 25th percentile- 75th percentile. The categorical variables are expressed as frequency and percentage. IBM® SPSS® v. 20 was used for the statistical analysis.
Results Implanter CentersA total of 88 CRT implanter hospitals/teams were identified; 85 (96.6%) answered the survey. Of these, 78 were public hospitals and 7 were private. The Table lists the number of implanter hospitals and the number of implants according to autonomous community, as well as the rate per million inhabitants. The results described correspond to the analysis of this sample, which we believe is closely representative of all current CRT therapy in Spain.
Autonomous Community Where the Cardiac Resynchronization Therapy Devices Reported Were Implanted, Number of Implanter Centers, Number of Implants, and Units per Million Inhabitants
| Implant centers, No. (no./million inhabitants | Units | Units/million inhabitants | |
| Total for Spain | 87 (1.88) | 2147 | 46 |
| Andalusia | 14 (1.69) | 373 | 45 |
| Aragon | 2 (1.52) | 21 | 15 |
| Principality of Asturias | 1 (0.94) | 29 | 27 |
| Balearic Islands | 3 (2.73) | 43 | 39 |
| Canary Islands | 4 (1.89) | 87 | 41 |
| Cantabria | 1 (1.73) | 51 | 88 |
| Castile and León | 6 (2.42) | 130 | 52 |
| Castile-La-Mancha | 5 (2.44) | 65 | 31 |
| Catalonia | 9 (1.23) | 265 | 36 |
| Valencian Community | 10 (1.99) | 289 | 57 |
| Extremadura | 2 (1.85) | 64 | 59 |
| Galicia | 4 (2.73) | 58 | 21 |
| Community of Madrid | 18 (2.82) | 414 | 64 |
| Region of Murcia | 2 (1.36) | 52 | 35 |
| Chartered Community of Navarre | 2 (3.21) | 72 | 115 |
| Basque Country | 5 (2.35) | 131 | 61 |
| La Rioja | 1 (3.2) | 8 | 26 |
Some of the differences among various autonomous communities are explained by patient referrals between the communities, rather than underusage of the therapy.
The total number of CRT device implants (first-time implants, replacements, CRT with/without implantable cardioverter-defibrillator [ICD]) reported was 2147 (621 pacemakers and 1486 ICD). According to EUCOMED data, 2518 devices (1833 ICDs and 685 pacemakers-CRT) were implanted during the same period (October 2010-September 2011), accounting for 85.6% of all implants in Spain. Therefore, based on the National Statistics Institute population census of 46 162 024 inhabitants for 2011, the total number of implants per million inhabitants reported was 46. According to EUCOMED, the total number of implants per million inhabitants was 54. Figure 1, Figure 2 show the number of implanter centers and the number of implants according to autonomous community and the number of implants per million inhabitants. Most implants reported were carried out in public hospitals (2028, 94.4%), and the mean number per hospital in Spain was 27 (21) implants. In the series, upgrades to an improved pacing mode accounted for 16.3% (10.6%), representing a substantial percentage of the total number of devices.
Figure 1. Number of implanter centers (centers per million inhabitants) according to autonomous community.
Figure 2. Number of implants (rate of implants per million inhabitants) according to autonomous community.
The main reason for the low rate of inclusion in Spain was improper referral of patients (94% of hospitals reported that patients are not referred), and other hospitals report budgetary restraints. A lack of confidence in the usefulness of CRT was reported by fewer than 12% of hospitals. Less than half the hospitals receive patients from other health areas, and 71% (21%) of patients are from the same health area. To increase the number of implants, most hospitals have proposed that the bulk of continuous training funds be used for courses that target the referring physicians (consistent with answers to similar questions) who acknowledge that CRT is not sufficiently recognized, a fact they believe explains the low rate of implants per million inhabitants.
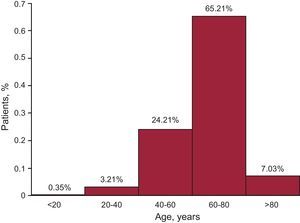
Patient SelectionCRT device implants continue to be indicated primarily in men (70.7%), possibly consistent with the higher incidence of ischemic heart disease and systolic dysfunction in this group. The mean left ventricular ejection fraction was 26.4% (5%), being 28.2% (5%) in patients with pacemakers and 24.7% (6%) in patients with ICDs. The mean patient age was 68 (12) years. Because of the age distribution of the Spanish population, a large majority (63.96%) of patients were between 60 and 80 years of age and very few implantations (5.3%) were performed in patients younger than 40 years of age (Figure 3). Implantation in patients older than 80 years of age is widely accepted by most hospitals in Spain (n=59); however, little more than 6% of these patients undergo this procedure, perhaps due to more numerous comorbidities and lower life expectancy. In this population group, a higher rate (76.6 [30.4]) of pacemaker implants was observed, which practically reverses the pacemaker/defibrillator ratio observed in the group as a whole.
Figure 3. Histogram of the number of cardiac resynchronization therapy implants according to age bracket.
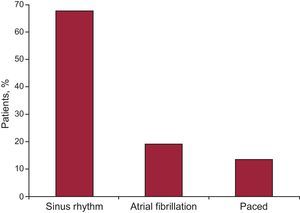
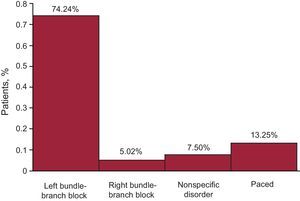
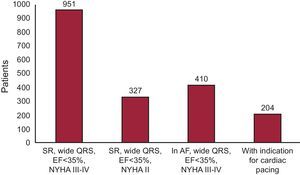
Most patients had an ischemic (48%) or idiopathic (46%) etiology, and CRT was indicated for valve disease or congenital heart disease in only a few patients. The majority of patients (67%) were in sinus rhythm (Figure 4), and the indication of atrial fibrillation accounted for 19%. Likewise, most patients (76.5%) had left bundle-branch block, followed by right bundle-branch block in 4.3% of patients and abnormal intraventricular conduction in 6.7%; all others were paced (Figure 5, Figure 6, Figure 7).
Figure 4. Rhythm of patient receiving cardiac resynchronization therapy.
Figure 5. Distribution of patients (n=2069) and electrocardiographic disorder.
Figure 6. Distribution of patients and New York Heart Association functional class.
Figure 7. Histogram of the clinical profile of patients receiving cardiac resynchronization therapy (n=1892) as per guidelines. AF, atrial fibrillation; EF, ejection fraction; NYHA, New York Heart Association; SR, sinus rhythm.
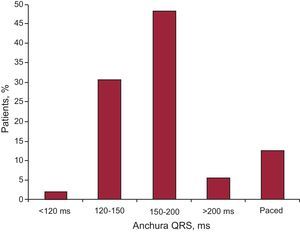
A total of 18 hospitals reported that they currently consider CRT to be indicated in patients with narrow QRS and mechanical asynchrony, an indication not within the latest clinical guidelines; these 18 centers account for almost 20% of hospitals, but for a much lower percentage of patients. The same observation was made regarding the number of hospitals (n=27) that perform CRT in patients with a standard indication for cardiac pacing, which means, among other things, a greater acceptance of CRT in these patients. In terms of QRS complex duration, although a significant number of hospitals acknowledged in previous questions that they consider CRT to be indicated in narrow QRS with mechanical asynchrony, in reality this indication accounted for a very low percentage of patients (2.1%). The largest (48.2%) group had a QRS complex duration of 150 ms-200 ms; 30.6% had QRS 120 ms-150 ms, and only 5.7% had QRS >200 ms (Figure 8).
Figure 8. QRS complex width in patients who received a cardiac resynchronization therapy device.
Implantation Tools and TechniquesIn Spain, CRT devices are most commonly implanted by electrophysiologists (73.8%), followed by cardiac surgeons (21.4%) and pacemaker specialists (8.3%); other specializations (interventional cardiologists, catherization specialists, and vascular surgeons) account for a lower percentage. The total sum exceeds 100% because various specializations perform the procedure in some hospitals.
The duration of implantation was considerably shortened from the initial times for the techniques, and the mean procedure time in Spain is currently 121.9 (38.7; range, 55-240) min. Epicardial (surgical) implants are used in many hospitals (32%), and the transseptal route is used in only a few (4.7%). The mean percentages of pacemakers and ICDs implanted in each hospital were 33.3% and 66.6%, respectively.
In terms of the implant system, 51.1% of hospitals stated that the main technical obstacle for an initial implant was lead introduction in the selected vein, followed by stability (26% of hospitals), and lastly, coronary sinus canalization and catheter guide withdrawal. For coronary sinus cannulation, 45.2% of hospitals use a catheter guidewire with an electrophysiology catheter support and 42.8% use only a catheter guidewire.
Most hospitals (82%) do not routinely use specific subselectors for vein selection, but only when the vein is not directly cannulated. Only 13% of hospitals use them in their usual procedure. Venoplasty of a vein that does not allow the lead to be initially advanced is also nonroutine: 82% of hospitals never perform venoplasty and select another, technically more favorable vein, and 13% reported that they perform this procedure only occasionally. Regarding the lead cables, 70.2% of hospitals initially use a bipolar lead for introduction in the selected coronary vein, 32.1% use a quatripolar lead, and 5.9% use an “active fixation” lead. The right ventricular lead is also placed differently in the various hospitals. The final site of the right electrode was high septal in 7.3% of hospitals, medioseptal in 20.1%, and the classic apical site in 72.7%. Thus, 38% of hospitals reported the use of alternative implant sites for the right ventricle and 62% did not.
Most hospitals (72.6%) do not use any method to enhance siting for left pacing before implantation, for example, to assess viability or scarring. Echocardiography is used for this purpose by 14.2% of hospitals, computed tomography by 4.7%, and magnetic resonance imaging by 9.5%. Regarding lead placement in the left ventricular vein as assessed by the question, “How satisfied are you with final lead placement?”, 60.4% rated the site as optimal, 29.3% as adequate, and 10% as suboptimal. The final site of the left ventricular lead in each vein stated was anterior in 2.15%, anterolateral in 13.1%, lateral in 42.4%, posterolateral in 45.1%, and middle cardiac vein in 2.1% of patients.
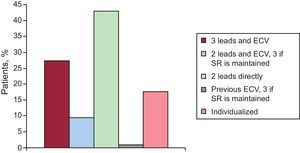
Management of Patients in Atrial FibrillationIn the case of implants in patients with atrial fibrillation, a wide variety of answers were received from all groups (Figure 9). Some hospitals (27.4%) implant 3 catheters including the atrium and perform electrical cardioversion, while others (9.5%) implant 2 and use cardioversion, and implant an atrial catheter if sinus rhythm is maintained. However, most (42.8%) implant 2 directly in the right and left ventricles. Another large group (21.4%) use individualized treatment according to clinical characteristics. A large majority of hospitals (63%) do not routinely perform node ablation in all patients in atrial fibrillation, but only when clinically indicated; however, 5.9% generally perform the procedure in all patients with atrial fibrillation who receive a CRT device. Patients in atrial fibrillation at the time of implantation who achieved sinus rhythm over their clinical course accounted for 0%-20% of the total (mean, 11.1 [10%]).
Figure 9. Management of patients in atrial fibrillation. ECV, electrical cardioversion; SR, sinus rhythm.
Perioperative Complications of Cardiac Resynchronization Therapy Device ImplantationThe reports of complications were generally few, but included procedural mortality (0.3% [1.5%] and hemorrhage in the pacemaker pocket (6.1% [7.1%]) as the most common, as well as pneumothorax, cardiac tamponade/pericardial effusion, hemothorax, coronary sinus dissection, phrenic nerve pacing, and lead dislodgement.
Postimplantation Programming and Follow-upIn terms of device optimization following implantation, most hospitals (54.7%) evaluate QRS complex width and set the VV and atrioventricular intervals using this information, but 27.3% use the automatic algorithms provided by some devices. A large group (19%) keeps the parameter within nominal parameters and performs optimization only when necessary, while another group (27.3%) performs echocardiographic optimization.
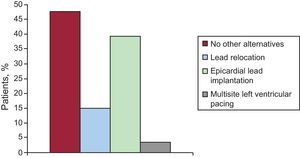
In most hospitals, the implanter group also provides clinical follow-up of the patient (67.8%). The CRT responder rate observed in Spanish hospitals is 73.8 (9%). This benefit was observed in patients immediately after CRT implantation in 17.8%, at 1 month in 50%, after 6 months in 15.4%, and at no time point in 21.4%. For nonresponders ineligible for transplantation, 47.6% of hospitals acknowledge no alternatives other than medical therapy optimization (Figure 10). However, 15.4% resite the lead at an alternative site, and many perform an epicardial (surgical) procedure if the lead cannot be placed in a lateral vein, considered ideal or if the vein does not exist (39.2%). Only a few groups perform multisite pacing (2 in the left ventricle) (3.5%).
Figure 10. Alternative treatment for cardiac resynchronization therapy nonresponders.
Late ComplicationsRegarding late complications observed with CRT, most centers acknowledge a significant percentage of inappropriate shocks in patients with an ICD-CRT device as primary prevention (8.4 [6.7%]). Lead dislodgement and phrenic nerve pacing were virtually the only late complications of the left ventricular lead that were reported.
Remote Patient and Device ManagementPatients using a device that allowed remote monitoring had the following distribution: fewer than 10% of patients at 36.9% of hospitals, 10%-40% of patients at 17.8% of hospitals, 40%-60% of patients at 9.5% of hospitals, 60%-80% of patients at 7.1%5 of hospitals, and more than 80% of patients at only 22.6% of hospitals. However, the hospitals that use remote monitoring acknowledge that this modality has shortened visit intervals by 35.7%. These institutions believe that this has helped improve the prognosis in 21% of patients and to optimize programming in 20%. These data are subjective estimations that would have required an additional controlled study specifically designed for this purpose.
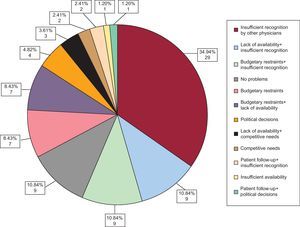
Discussion Activity Data Listed in the Register and Adherence to Clinical GuidelinesThe number of CRT implanter centers has gradually increased in Spain up to the 88 identified: 24 hospitals reported 10 or fewer implants, 12 (14.2%) reported 50 or more implants/year, and no hospitals reported more than 100 implants per year. The total number of implants reported was 2147. Based on the EUCOMED data, the estimated total number is 2518, or more than 85% of the total number of implants in Spain. Dividing this number among all Spanish hospitals gives a mean of 27 (21) implants per hospital, a figure which reflects the wide dispersion of hospitals for a relatively low total volume compared with the European data. The main reason for the low rate of inclusion in Spain is improper referral of patients (patients are not referred) (Figure 11). It should be stressed that information should be given to the primary healthcare physicians and internists who, along with cardiologists, follow these patients and refer them when needed. Most hospitals do not report an increase in the number of devices indicated following the publication of the new CRT clinical guidelines in 2010, probably because the indications of functional class II and in atrial fibrillation were already recognized, as observed in the 2008 European Register.4 Although the new guidelines include recommendations on the type of device (pacemaker or ICD), most centers do not report an influence on the number of devices indicated.
Figure 11. Main reasons for the low rate of inclusion in Spain. Multiple answers have been combined for greater understanding.
Patient ScreeningThe management of patients with acute heart failure is increasingly complex and costly, precisely at a time of stronger budgetary restraints due to the economic crisis. This situation may compromise appropriate treatment for many patients, particularly for the use of new therapies. Cardiologists’ skill in selecting ideal patients and improving efficiency is key. In our study, clinical evidence was the basis for most indications (eg, the presence of left bundle-branch block, sinus rhythm, and high functional class). As with all registers and clinical studies, it will always be extremely difficult to determine how many patients were unable to gain access to this therapy. Although many hospitals are currently using CRT in patients with narrow QRS complex and mechanical asynchrony and in patients with conventional cardiac pacing, the number of patients included by the hospitals for this reason is very low.
Management of Patients in Atrial FibrillationThe management of patients in atrial fibrillation who receive a CRT device varies considerably in Spain, and most hospitals do not routinely perform node ablation in all patients in atrial fibrillation but only when clinically indicated. These data are certainly conditioned by the experience of each hospital in the percentage of patients who are in atrial fibrillation at the time of implantation and who achieve sinus rhythm over their clinical course.
Postimplantation Programming and Follow-upMost hospitals currently perform optimization by empirically considering only the QRS complex width and the atrioventricular interval. There is no evidence to recommend echocardiographic optimization of pacing intervals in all patients after CRT.8, 9, 10, 11 Empirical programming of the atrioventricular interval around 120 ms and the VV interval to achieve the narrowest QRS in the surface electrocardiogram appears to be adequate in terms of cost-effectiveness. Optimal pacing intervals vary over time as ventricular remodeling processes develop and also with changes in hemodynamic and sympathetic tone conditions occurring during exercise. Remote monitoring for the management of patients with CRT is still not widely used in Spain. However, the hospitals that use it acknowledge that they have greatly reduced visit intervals as a result and believe that the technique has enhanced patient improvement.
Comparison With European DataThe arrhythmia (European Heart Rhythm Association) and heart failure groups of the European Cardiology Society maintained a CRT register in Europe from November 2008 to June 2009.4 This European register included 140 hospitals selected from 13 countries, with a total of 2438 patients, a figure probably well below 10% of implants performed in Europe. The mean age of patients included in this register was 70 years. In all, 78% patients were in New York Heart Association functional class III or IV and 22% were in class I and II. These figures are somewhat similar to our data, but are from 2 years earlier and precede the publication of large class II studies, probably because the experience of these hospitals (many of whom certainly participated in those studies) was already positive in this regard. The EUCOMED7 data provide information on the number of implants and types of devices in Europe. The mean number of CRT implants is 131 per million inhabitants, including ICD-CRTs (100) and pacemaker-CRTs (31). Germany (175 implants/million) is the country with the highest number of implants, whereas Spain (51 implants/million) continues to rank last among the countries reporting data to EUCOMED. Figures were above the mean for Italy (200), the Netherlands (163), and the Czech Republic (163), but below the mean for Portugal (59) and Spain (51), among others.
Differences Among Autonomous CommunitiesNoticeable differences in the rate of implants were seen among the various autonomous communities. The mean rate estimated in this study was 46 per million inhabitants, with levels above the mean in the Chartered Community of Navarre, Cantabria, the Community of Madrid, Basque Country, Extremadura, the Valencian Community, and Castile an León, in that order. All others were below the mean: Andalusia, Aragon, the Principality of Asturias, the Balearic Islands, the Canary Islands, Castile-La Mancha, Catalonia, Galicia, the Region of Murcia, and La Rioja. As with other device implants, the differences can be partly explained by demographic differences in the population and by the number and extent of development of arrhythmia units in the various autonomous communities.12, 13, 14, 15, 16, 17
LimitationsDespite efforts to locate hospitals with an active CRT implant program, some hospitals may not have been identified. However, the total number of implants reported, which is similar to that reported by EUCOMED, suggest that the data presented are indicative of the actual situation in Spain. We have no information on patients assessed for CRT who did not receive an implant or on unsuccessful attempts at implantation.
ConclusionsThe new indications recommended by the guidelines are gradually being implemented, according to data obtained from patients in class II or with atrial fibrillation. Nevertheless, the number of CRT device implants is still well below the European average. Further efforts are needed to ensure that this treatment reaches all potential patients in Spain who could benefit from it.
Conflicts of interestNone declared.
Acknowledgements
To all the professionals, for their voluntary and selfless participation.
Appendix. List of public and private hospitals, according to autonomous community, that participated and physicians who completed the survey| Andalusia | |
| Hospital de Jaén, Jaén | Rocio Cozar |
| Hospital Clínico Virgen de la Victoria, Malaga | Javier Alzueta |
| Hospital Nuestra Señora de Valme, Seville | Juan Leal |
| Hospital Costa del Sol, Malaga | F. Ruiz Mateas |
| Hospital Universitario Virgen del Rocío, Seville | A. Pedrote |
| Hospital Universitario Puerta del Mar, Cadiz | Lucas Cano |
| Hospital Universitario Virgen Macarena, Seville | Ernesto Diaz Infante |
| Hospital Carlos Haya, Malaga | Manuel Rodríguez |
| Hospital Clínico San Cecilio, Granada | Jose Miguel Lozano |
| Hospital Juan Ramón Jiménez, Huelva | Joaquín Barba |
| Hospital Universitario Reina Sofía, Cordoba | Amador López Granados |
| Hospital Torrecárdenas, Almeria | Franc Tornes |
| Hospital Virgen de las Nieves, Granada | Silvia López |
| Aragon | |
| Hospital Clinico Universitario Lozano Blesa, Zaragoza | Gonzalo Rodrigo |
| Hospital Universitario Miguel Servet, Zaragoza | Antonio Asso |
| Principality of Asturias | |
| Hospital Universitario Central de Asturias, Oviedo | José Rubin, David Calvo |
| Balearic Islands | |
| Hospital Son Llàtzer, Palma de Mallorca | Xavier Fosch Mur |
| Hospital Son Dureta, Palma de Mallorca | Carmen Expósito |
| Clínica USP-Palmaplanas, Palma de Mallorca | Antonio Berruezo |
| Canary Islands | |
| Hospital Universitario de Canarias, San Cristobal de La Laguna | Aníbal Rodríguez, Francisco Bosa |
| Hospital Universitario de Gran Canaria Dr. Negrín, Las Palmas de Gran Canaria | Eduardo Caballero Dorta |
| Hospital Nuestra Señora de Candelaria, Santa Cruz de Tenerife | Rafael Romero, Julio Hernández |
| Hospital Universitario Insular de Gran Canaria, Las Palmas de Gran Canaria | Olga Medina |
| Cantabria | |
| Hospital Marqués de Valdecilla, Santander | Victor Exposito |
| Castile-La-Mancha | |
| Complejo Hospital Universitario de Albacete, Albacete | A. Sacristán |
| Hospital Nuestra Señora del Prado, Talavera de la Reina | Alfonso Macías |
| Complejo Hospitalario de Toledo, Toledo | Miguel Angel Arias |
| Hospital General de Ciudad Real, Ciudad Real | Javier Jimenez Diaz |
| Castile and León | |
| Hospital Universitario de León, Leon | Marisa Fidalgo, J.M. Glez Rebollo |
| Hospital General Yagüe, Burgos | Javier Garcia |
| Hospital Nuestra Señora de Sonsoles, Avila | A. Borasteros |
| Hospital Clínico Universitario de Valladolid, Valladolid | Jerónimo Rubio |
| Hospital Universitario del Rio Hortega, Valladolid | Diego Pérez, Benito Herrero |
| Complejo Hospitalario de Salamanca, Salamanca | Claudio Ledesma |
| Catalonia | |
| Hospital Universitari Germans Trias i Pujol, Badalona | Roger Villuendas |
| Hospital Sant Joan de Déu, Esplugues de Llobregat | Giorgia Sarquella |
| Hospital Clínic, Barcelona | Chema Tolosana |
| Hospital Universitari Joan XXIII, Tarragona | Alfredo Bardají |
| Hospital del Mar, Barcelona | Victor Bazan |
| Hospital de la Santa Creu i Sant Pau, Barcelona | Xavier Viñolas |
| Hospital Universitari de Bellvitge, L’Hospitalet de Llobregat | Ignasi Anguera |
| Hospital Universitari Arnau de Vilanova, Lleida | F. Worner, J. Tomás, Berta Daga |
| Hospital Universitari Vall d’Hebron, Barcelona | Angel Moya, Jordi Pérez Rodón |
| Valencian Community | |
| Hospital Clínic Universitari, Valencia | Ricardo Ruiz Granell |
| Consorci Hospital General Universitari, Valencia | Aurelio Quesada |
| Hospital Universitari i Politècnic La Fe, Valencia | M.J. Sancho Tello, Chimo Osca |
| Hospital de Xàtiva, Xàtiva | Manuel Rodriguez Serra |
| Hospital General de Castelló, Castelló de la Plana | Jose Diago, Eloy Domínguez |
| Hospital Dr. Peset, Valencia | Llorens Miralles |
| Hospital Universitari Sant Joan d’Alacant, Sant Joan d’Alacant | Vicente Bertomeu |
| Hospital General Universitario de Alicante, Alicante | Juan Gabriel Martinez |
| Hospital del Vinalopó, Elche | Juan Antonio Fernández |
| Hospital de Torrevieja, Torrevieja | Miguel Godoy |
| Extremadura | |
| Complejo Hospitalario de Cáceres, Caceres | Javier Portales |
| Hospital Infanta Cristina, Badajoz | J. Fernandez de la Concha, J.J. Guerrero |
| Galicia | |
| Hospital Povisa, Vigo | María Vazquez |
| Hospital do Meixoeiro, Vigo | Xulio Beiras Torrado |
| Hospital Juan Canalejo, A Coruña | L. Perez Alvarez, Enrique Ricoy |
| Complejo Hospitalario Universitario de Santiago de Compostela, Santiago de Compostela | Javier Garcia Seara |
| Community of Madrid | |
| Hospital Central de la Defensa Gómez Ulla, Madrid | Miguel Rubio |
| Fundación Jiménez Díaz, Madrid | Jose M. Rubio |
| Hospital Universitario La Paz, Madrid | Jose Luis Merino, Jorge Silvestre, Rafael Peinado |
| USP Hospital San Camilo, Madrid | Concepción Moro |
| Hospital Ramón y Cajal, Madrid | A. Hernández-Madrid, R. Matía, Inmaculada Sánchez |
| Hospital Universitario de Getafe, Getafe | F.G. Cosío, Ambrosio Núñez |
| Hospital Severo Ochoa, Leganés | Angel Grande |
| Hospital 12 de Octubre, Madrid | María López Gil, Jesús Rodríguez |
| Hospital Clínico San Carlos, Madrid | Javier Moreno |
| Hospital Gregorio Marañón, Madrid | Felipe Atienza |
| Hospital Quirón, Madrid | José Angel Cabrera |
| Hospital de Sanchinarro, Madrid | Jesús Almendral |
| Hospital Puerta de Hierro, Majadahonda | Ignacio Fernández Lozano |
| Hospital de Fuenlabrada, Fuenlabrada | Joaquín Alonso, Alejandro Curcio |
| Region of Murcia | |
| Hospital Universitario Virgen de la Arrixaca, El Palmar | Arcadio García Alberola |
| Hospital de Lorca, Lorca | Jorge Silvestre |
| Chartered Community of Navarre | |
| Hospital de Navarra, Pamplona | José Ramón Carmona |
| Clínica Universidad de Navarra, Pamplona | Ignacio García Bolao |
| Basque Country | |
| Hospital Nuestra Señora de Aránzazu, San Sebastián | Tx. Porres |
| Hospital de Basurto, Bilbao | J.M. Ormaetxe, M. Fe Arcocha |
| Hospital de Galdakao, Galdakao | J. Zumalde |
| Hospital de Cruces, Baracaldo | Andrés Bodegas |
| Hospital Txagorritxu, Vitoria | José Ferrer |
| La Rioja | |
| Hospital San Pedro, Logroño | Diego Lorente |
Received 13 February 2012
Accepted 18 March 2012
Corresponding author: Unidad de Arritmias, Servicio de Cardiología, Hospital Ramón y Cajal, Ctra. Colmenar Viejo Km 9,100, 28034 Madrid, Spain. antoniomadri@gmail.com