Implantable cardioverter-defibrillators (ICDs) have been shown to reduce cardiovascular mortality in patients with heart disease and a high risk of arrhythmias largely associated with reduced left ventricular ejection fraction (LVEF). ICD batteries, however, have a limited life span, and when a battery reaches the end of its life, the generator needs to be replaced if the device is to continue to function. Although there are guidelines on how and when to deactivate ICDs in patients in the final stages of life,1 little has been written about another important decision: whether or not to replace the generator at the time of battery depletion.
ICD follow-up is usually conducted separately from patient follow-up (evaluation of heart disease and comorbidities) and is often undertaken by nurses under medical supervision. Generators should not be automatically replaced at battery depletion. Decisions on replacement vs nonreplacement should only be taken after a full clinical evaluation and consideration of a range of factors, discussed below and summarized in table 1.
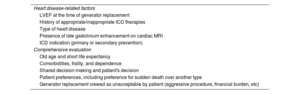
Main factors that may influence the decision not to replace an ICD generator
| Heart disease-related factors |
| LVEF at the time of generator replacement |
| History of appropriate/inappropriate ICD therapies |
| Type of heart disease |
| Presence of late gadolinium enhancement on cardiac MRI |
| ICD indication (primary or secondary prevention) |
| Comprehensive evaluation |
| Old age and short life expectancy |
| Comorbidities, frailty, and dependence |
| Shared decision-making and patient's decision |
| Patient preferences, including preference for sudden death over another type |
| Generator replacement viewed as unacceptable by patient (aggressive procedure, financial burden, etc) |
ICD, implantable cardioverter-defibrillator; MRI, magnetic resonance imaging.
This document is endorsed by the Heart Rhythm, Heart Failure, and Ischemic Heart Disease Associations of the Spanish Society of Cardiology (SEC) and by the Geriatric Cardiology Section of the SEC.
LVEF ImprovementNo randomized controlled trials (RCTs), or even prospective studies, have demonstrated the safety of generator nonreplacement in ICD carriers with LVEF improvement. Nonetheless, patients whose LVEF improves to >45% are considered to be at a low risk of ventricular arrhythmias. The findings of a recent analysis of real-world data on more than 60 000 patients from the National Cardiovascular Data Registry Implantable Cardioverter Defibrillator Registry2 suggest that generator replacement does not offer a survival benefit in many ICD carriers, particularly those with a primary prevention indication and an LVEF >35% at the time of battery depletion. The association between LVEF improvement during follow-up and a reduction in the frequency of ventricular arrhythmia episodes requiring ICD shocks is supported by the results of several meta-analyses. One of these found that patients with an LVEF >35% had a 3-fold higher risk of appropriate ICD therapy after generator replacement than those with an LVEF <35%.3
Optimization of medical treatment and use of new heart failure treatments such as sacubitril-valsartan and sodium-glucose cotransporter type 2 inhibitors have increased LVEF recovery rates. Indeed, a sizeable number of ICD carriers no longer meet the criteria for implantation. Even before the wider-scale use of novel heart failure medications, approximately one-third of primary prevention ICD carriers with heart failure and a low LVEF no longer met the criteria for ICD therapy at the time of battery depletion (their LVEF had improved to >35%).4 Most observational studies have shown that patients without persistent ICD indication at battery depletion have low rates of appropriate ICD therapy after generator replacement,5 although not all studies have found this to be the case.4 There is also evidence that other factors such as ischemic heart disease and age might contribute to a nonnegligible risk of sustained ventricular arrhytmias.6
LVEF improvement is also common in ICD carriers on cardiac resynchronization therapy (CRT). Some authors have shown that it may be safe to downgrade to a CRT pacing system (without ICD function) in this setting when the implant indication was primary prevention,7 although, again, conflicting findings have been published.8 A reduction in ventricular arrhythmia risk appears to be more closely linked to the magnitude of LVEF improvement than to absolute LVEF values. No RCTs have compared generator replacement vs downgrading to a CRT pacing system in ICD carriers on CRT.
Bilchick et al.2 recently proposed combining LVEF values with predicted annual arrhythmic mortality based on the Seattle Proportional Risk Model to estimate the survival benefit associated with ICD generator replacement. Late gadolinium enhancement on cardiac magnetic resonance imaging is also now known to be associated with an increased risk of ventricular arrhythmias and should perhaps be taken into account when making a final decision on generator replacement.9
Absence of Appropriate ICD TherapyMost patients do not receive appropriate ICD therapy during the average lifespan of a generator. In the INSURE10 (INcidence free SUrvival after ICD REplacement) trial, the risk of appropriate therapy after generator replacement was 3 times higher in patients who had already received appropriate shocks; a similar figure was reported by Weng et al.11 Nonetheless, 21% of patients without former appropriate ICD therapy received appropriate shocks after generator replacement, and this rate was even higher in another study, at 27%.4 Although some studies have reported lower rates of appropriate ICD therapy after generator replacement, the absence of prior appropriate therapy should not constitute the sole reason for nonreplacement. In brief, while a history of appropriate ICD therapy would tip the balance in favor of replacement, absence of such a history should not automatically exclude this option.
Short Life Expectancy, Older Age, Comorbidities, and FrailtyCandidates for generator replacement are generally older. Older age per se, however, is not a reason for nonreplacement, although it is associated with a higher risk of noncardiac mortality and fewer ICD benefits. Scores from comorbidity scales featuring different combinations of diseases indicate that comorbidity increases the risk of noncardiac death after ICD implantation (the most frequently identified risk factor alongside age is kidney failure). Nonetheless, as shown in a systematic review for the 2017 clinical practice guideline for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death, ICD implantation is associated with reduced mortality in real-world settings, even in patients with several comorbidities.12 The more recent European Society of Cardiology guidelines on the prevention of sudden cardiac death indicate that forgoing ICD implantation could be considered in certain patients based on age and comorbidities (class IIa recommendation).9
Although complications associated with generator replacement are uncommon, the risk of occurrence increases slightly with older age and comorbidities. While these factors alone are not generally considered a contraindication for generator replacement, they should be included in the decision-making process and in the information given to patients.
Finally, a comprehensive geriatric assessment, including an evaluation of frailty and dependence, should be performed before ruling out generator replacement in older patients with comorbidities. It should also be noted that frailty is sometimes reversible, although difficult to assess. Involvement of a geriatric specialist to help with decision-making in problematic cases is thus recommended.
Shared Decision-MakingAdvance planning and shared decision-making are crucial when assessing candidacy for ICD generator replacement. However, clinical opinions vary widely on the advisability of performing this procedure and on the steps to be taken in the decision-making process. Shared-decision making is relatively commonplace prior to ICD implantation, but despite being recommended by the American Heart Association,13 it is often overlooked during follow-up or at the time of battery depletion. A structured approach integrating both evidence and patient preferences enables clinicians and patients to work together to reach a decision.
Generator replacement or nonreplacement is not generally something that patients think about in advance. It is therefore important to provide them with a balanced picture of the available evidence, to discuss the risks and possible benefits of each option, and to give them time to process this information. Recommending replacement is easy when the patient's wishes concur with medical opinion, but it is important to explore the reasons behind these wishes and to ensure that the patient understands the implications of their decision. In addition, this process, together with a note of the values influencing the patient's final decision, must be recorded in the patient's medical record. The use of tools and strategies to support shared decision-making is recommended, particularly when dealing with older patients, many of whom will have been raised in a paternalistic social and medical environment and some of whom may not want to engage in shared decision-making.
The Patient's DecisionLewis et al.14 found that most ICD carriers were unaware that generator replacement was optional and that more than 25% would have considered nonreplacement had they know it was a possibility. The clinical characteristics of these patients were similar to those of the patients who would have chosen replacement, suggesting there are other issues at play. Not all patients who have to pay for a new generator, for example, might be willing or able to do so, while others express a clear preference for sudden death. Irrespective of this consideration, patients need to understand that there is no such thing as a zero risk of ventricular arrhythmias during follow-up and that choosing to forgo generator replacement could result in sudden cardiac arrest.
The role of the clinician in such cases is to distinguish between the different areas of the decision-making process and ensure that the patient understands that their decision may not match the professional viewpoint and could entail risks. It is important to distinguish between the objective decision made by the clinician or medical team (which expects the benefits of replacement to outweigh the risks) and the subjective decision made by the patient, who decides to undergo what they consider to be a tolerable rather than an unbearable procedure.
Downgrading to Another DeviceSome patients will still need pacing once it has been decided not to replace the ICD generator. Early ICD connectors (DF-1) have 3 contacts: 2 for the defibrillation coils and 1 for pacing and sensing. In such cases, the generator can be disconnected, the 2 coil contacts disconnected, and a pacemaker connected to the pacing and sensing contact. Most modern ICD generators have a single DF-4 connector that cannot be connected to a pacemaker generator. In this case, a new ventricular pacing lead will need to be implanted. Alternatively, a new generator with a deactivated shock function could be implanted, but this is obviously much more expensive.
If the goal is to main resynchronization only in a patient with a CRD defibrillator system with a DF4 connector, a standard pacemaker could be connected to the left ventricular lead. Placement of a new pacing lead in the right ventricle will need to be considered if the goal is to maintain biventricular pacing, but this procedure is more complex and carries a higher risk of complications.
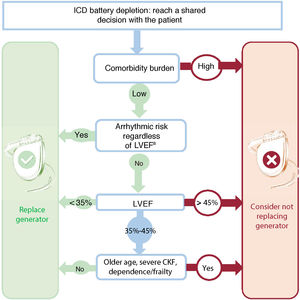
Clinical ImplicationsRCTs evaluating the benefits of ICD generator replacement in doubtful situations are strongly recommended. In the meantime, clinicians should note that generator replacement is not mandatory and apply a decision algorithm similar to that shown in figure 1, which can easily be incorporated into ICD follow-up units. The recommendations of this algorithm should not be taken as a definitive guide. It is difficult to predict sudden cardiac arrest, and decisions can be particularly challenging in certain populations, such as older patients.15 In brief, LVEF recovery (following resynchronization and/or adjustment of medical treatment) reduces the risk of ventricular arrhythmias, especially in patients with dilated cardiomyopathy without late gadolinium enhancement. Accordingly, nonreplacement of a generator could be contemplated in patients with a primary prevention ICD who show an improvement in LVEF (especially when this reaches >45%) and do not have a history of appropriate therapy from the device. Finally, there is some evidence of a significant residual risk of appropriate therapy after generator replacement, even in elderly patients without prior appropriate ICD therapy. Both clinicians and patients thus need to be willing to accept some uncertainty, particularly in the setting of ischemic heart disease.
Proposed algorithm for guiding decisions on ICD generator replacement at the time of battery depletion. CKF, chronic kidney failure; ICD, implantable cardioverter-defibrillator; LVEF, left ventricular ejection fraction.
a Ischemic and arrhythmogenic heart disease, ventricular arrhythmias, and appropriate therapy.
Decisions on whether or not to replace an ICD generator at the end of battery life should be taken after a careful evaluation of the associated risks and benefits and of individual patient circumstances. Factors that should be taken into account include heart disease-related factors (etiology and LVEF), ICD indication (primary or secondary), previous ICD therapies, comorbidities, life expectancy/quality of life, and frailty/dependence. The final decision should be taken by the patient, who will have been adequately informed about potential benefits and the risk of complications.
FundingNone.
Conflicts of InterestNone.
Expert review committee: José Daniel Martínez-Alday, Hospital Universitario de Basurto, Bilbao, Spain; Marta Pachón, Servicio de Cardiología, Hospital Universitario de Toledo, Toledo, Spain; José María Tolosana, Servicio de Cardiología, Hospital Clínic, Universitat de Barcelona, Barcelona, Spain.