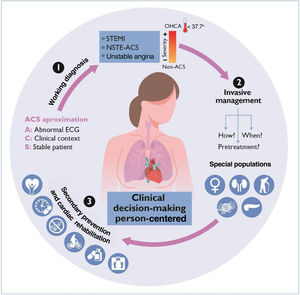
The European Society of Cardiology (ESC) has achieved a notable success by releasing a single document for the management of acute coronary syndromes (ACS),1 as patients presenting with ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation (NSTE-ACS) share many common pathways, such as the initial diagnostic work-up, antithrombotic regimes and secondary prevention strategies. Therefore, the document reflects more accurately the clinical setting. Moreover, the new guidelines are more dynamic and contain numerous figures that can help physicians in their daily practice, as well as a central illustration useful to disseminate key messages.
NOVELTIESThe 37 main new recommendations and/or significant changes can be categorized into several sections.
Antithrombotic therapyOn this topic, we wish to emphasize 2 new recommendations. First, it is recommended (I-C) to resume dual antiplatelet therapy (DAPT) for at least 12 months, after an ACS treated with either coronary artery bypass graft (CABG), percutaneous coronary intervention (PCI), or conservative strategy. Second, it is not recommended to de-escalate antiplatelet therapy within first 30 days after an ACS (III-B).
One of the most controversial aspects of these guidelines is the downgrading of pretreatment with P2Y12-inhibitors in STEMI patients undergoing PCI from class of recommendation I-A to IIb-B. This is mainly based on the results of the ATLANTIC trial,2 in which pretreatment with ticagrelor during transfer (31minutes before PCI) failed to show a benefit compared with administration immediately before angioplasty. Nevertheless, there was indeed a reduction in stent thrombosis and no increased bleeding risks. In addition, pretreatment with prasugrel was not explored.
Invasive strategy: timing and technical aspectsThe recommendation of an early invasive strategy (within first 24hours) in high-risk patients with NSTE-ACS has been downgraded from class I-A to IIa-A, since it has not been proved beneficial when universally applied, thereby resolving the controversy surrounding this recommendation.
Regarding technical aspects, for the first time, the guidelines recommend PCI in patients with spontaneous coronary artery dissection only if there are signs/symptoms of ongoing ischemia, a large area of myocardium at risk, and/or reduced anterograde flow (I-C).
Cardiac arrestThere is a dedicated section for out-of-hospital cardiac arrest (CA), in which the role of networking on system care has been enhanced by recommending transport of patients with CA and suspected ACS to a 24/7 PCI capable center (IC); moreover, transport to a CA center should be always considered (IIa-C). Neurological prognosis should be evaluated after 72hours (I-C).
Two previous recommendations have been modified. First, routine immediate coronary angiography is no longer recommended in hemodynamically stable patients without persistent ST-segment elevation (III-A) in light of several clinical trials, including the multicenter Spanish COUPE,3 as it does not provide a survival benefit over delayed angiography. Second, temperature control for patients remaining unresponsive after return of spontaneous circulation is still recommended, but the target has been relaxed to active prevention of fever (ie, >37.7°C) for at least 72hours (I-B).
Management of noninfarct-related arteries in patients with multivessel diseaseThe results of the COMPLETE trial4 have influenced the new guideline, upgrading the recommendation to perform complete revascularization, either during hospital admission or after discharge (within 45 days), from class IIa-A to I-A. A few days after the publication of the guidelines, the MULTISTAR-AMI trial (immediate vs staged PCI) was presented, showing a significant reduction in the incidence of MACE at 1 year for immediate (8.5%) vs staged PCI (16.3%).5 This study has a limited sample size and a noninferiority design, and several methodological aspects could be considered controversial; in addition, this large difference was mainly driven by higher periprocedural myocardial infarction in staged PCI.
Patients with cancer and acute coronary syndromeIn patients with cancer and ACS, PCI improves survival6 and therefore an invasive strategy should be preferred if survival ≥6 months is expected (I-B). Conversely, if the expected survival is short and/or bleeding risk is very high, a conservative strategy should be considered (IIa-C).
To reduce bleeding risks in patients with cancer, 3 new antithrombotic recommendations have been included (III-C) based on patients’ platelet count: avoid a) aspirin if <10 000/μL; b) clopidogrel if <30 000/μL; c) prasugrel/ticagrelor if <50 000/μL.
Finally, temporary interruption of cancer therapy and an urgent multidisciplinary approach is recommended when it is suspected to be a contributing cause of ACS (I-C).
Patients’ perspectiveAs a novel and truly positive aspect, the guidelines include a section on patients’ perspectives, shared decision-making, informed consent, patient-reported outcome measures (PROMs), and patient-reported experience measures (PREMs). The document recommends individualizing the care of patients with ACS by considering their needs, beliefs values and preferences, and ensuring shared decision-making (I-B). The “teach back” technique is suggested to ensure their understanding.
CONSEQUENCES OF IMPLEMENTATION IN SPAINClass I recommendations have been summarized and class III recommendations are given in the same proportion as in the previous guidelines. Thus, there are more class II recommendations (36%), making the decision-making process more challenging for physicians.
Antithrombotic therapyEven though interventional cardiology and stents have changed the prognosis of patients presenting with an ACS, there are still some drawbacks, including patients’ persistent ischemic risk due to stent thrombosis. DAPT has been the cornerstone for reducing thrombotic complications. The late onset of action of oral P2Y12-inhibitors is their Achilles’ heel. The strong evidence to support pretreatment withP2Y12-inhibitors due to their safety and efficacy in reducing the rates of definite stent thrombosis2 led to the implementation of this strategy in the routine care of patients presenting with STEMI. Nevertheless, it remains unknown whether this strategy improves patients’ clinical outcomes or coronary reperfusion.
Discouraging routine pretreatment with oral P2Y12-inhibitors in patients with both STEMI and NSTE-ACS might indirectly promote the use of alternatives such as cangrelor, the first and only intravenous P2Y12-inhibitor approved by the European Medicines Agency. There is a growing body of evidence from studies conducted in real-world settings showing the safety and efficacy of updated protocols combining intravenous cangrelor plus oral transition to prasugrel/ticagrelor.7 This shift of paradigm might be reasonable in STEMI when the time between diagnosis and PCI is expected to be short. The cost-effectiveness of more widespread use of cangrelor is unknown, but it could lead to savings due to lower use of GP IIb/IIIa-inhibitors, shorter in-hospital wash-out periods of surgical candidates, and fewer ischemic complications.
Improvements in stent technology (polymer-free stents, biodegradable polymers stents, etc) have fuelled debate on the optimal duration of DAPT after index ACS revascularization. Patients’ risk of developing either thrombotic or bleeding complications is dynamic, and DAPT duration should be individualized and re-assed. These guidelines have been highly consistent with this statement and present alternative antithrombotic regimes that better fit patients’ clinical characteristics.
Invasive strategiesThe role of nurses is pivotal in the early diagnosis and treatment of ACS. In Spain, nurses lead patient triage, so it is essential to emphasize their education and raise awareness of the importance of minimizing delays.8
Downgrading the recommendation for an early invasive strategy in patients with high-risk NSTE-ACS is more appropriate when considering that health care systems have limited resources (ie, weekends, night shifts) and current evidence has shown its lack of benefit.9 However, delayed revascularization combined with the absence of pretreatment could translate into more thrombotic events. Therefore, prospective registries will be needed to determine the implications of these recommendations if they are fully applied.
Novelties in the technical aspects of invasive strategies support the use of intravascular imaging, which will further aid in the PCI-decision-making process and might improve PCI-related outcomes in upcoming years.
Management of noninfarct-related arteries in patients with multivessel diseaseInvasive epicardial functional evaluation of noninfarct related arteries (non-IRA) is growing. However, its superiority over angiographic imaging is controversial, as the latter is recommended to evaluate lesion severity (I-B). The net benefit of performing systematic second-time coronary angiograms for patients and health care systems might be questioned if the main usefulness of functional evaluation is to rule out revascularization. When non-IRA revascularization is indicated, the benefit of immediate vs staged PCI remains to be determined and the indication should be individualized.
Cardiac arrestIn the past few years, hyperinvasive strategies such as routine immediate angiography in stable patients without persistent ST-segment elevation or therapeutic hypothermia were thought to provide survival benefits to patients with a nonfatal CA. Currently, new evidence has provided principles to establish a more contemporary postresuscitation care and has reminded us the need to search for new lines of investigation in this field, even if trial results may not be fully extrapolated to all clinical CA scenarios (ie, lower rates of bystander resuscitation and use of automatic defibrillators). The role of CA centers could be the solution to standardize management and provide optimal care.
Patients with cancerAs the proportion of patients with cancer and ACS is rising, we need to be prepared to offer them strategies that reduce all-cause mortality such as PCI (especially if expected survival ≥ 6 months) and appropriate antithrombotic regimens (adjusted to coexisting thrombotic/hemorrhagic risks). Providing high-quality care to this population will certainly demand specialization and the creation of multidisciplinary teams.
Patients’ perspectiveGlobal access to information has improved patients’ knowledge of various cardiology conditions and treatments, and has contributed to establishing shared decision-making processes. Person-centered care instead of patient-centered care must be the gold-standard of clinical practice. To achieve it, health care systems must also provide health care-related personnel with the necessary time and resources.
Secondary preventionThe current guidelines maintain the recommendation to participate in a cardiac rehabilitation program following an ACS (I-A) as soon as possible and to adopt a healthy lifestyle (I-B). As referral rates, participation, and implementation continue to be low, telerehabilitation is presented as an optimal alternative.10 It is important to optimize the use of our resources, including the regular practice of aerobic and resistance exercise, psychological and pharmacological interventions, in order to achieve educational, medical and pharmacological adherence and improve cardiovascular outcomes during follow-up.
GAPS IN KNOWLEDGERegarding the levels of evidence of the recommendations, only 29% are A and 38% C, reflecting that there are still many gaps in evidence despite the accumulation of new scientific evidence since the publication of the previous guidelines.
Diagnostic accuracy and management in STEMI and NST-ACSNormal coronary arteries are found in a significant proportion of patients with a suspected STEMI diagnosis leading to activation of the reperfusion network. Optimizing STEMI diagnosis in these patients could reduce the need for transfer between hospitals and promote a more rational use of health care resources. In this regard, research on the use of machine learning techniques for improving ECG diagnosis of STEMI is warranted.11
The applicability of some of the guidelines’ recommendations to current clinical practice is challenging. A significant proportion of very high and high-risk NST-ACS patients do not undergo an early invasive strategy, especially those admitted to non-PCI capable centers. Achieving this goal might require reorganization of networks, like those for STEMI.
Acute coronary syndromes with unstable presentationCardiogenic shock (CS) is associated with high mortality. Obtaining scientific evidence in this setting is extremely difficult, mostly because of the complexity of including critical patients in randomized trials and their clinical heterogeneity (cause/severity of shock). Regarding the role of intra-aortic balloon pump and mechanical circulatory support (MCS) in patients with AMI-related CS, most trials have failed to show significant benefits. Better definition of CS phenotype (severity, presence of CA) would probably help in the design of future trials. Likewise, there is a need for clearer definition of aspects such as the unloading strategy in veno-arterial extracorporeal membrane oxygenation patients, the timing of percutaneous MCS support, and the selection of high-volume centers.
As mentioned above, patients with CA differ in terms of their etiology and clinical profile. Assessing the potential impact of emergent angiography according to the clinical profile and burden of cardiovascular risk factors might help to reduce areas of uncertainty. Notwithstanding, the use of artificial intelligence techniques in the assessment of ECGs in patients with CA might identify patterns related to coronary artery occlusion.
Special populations: elderly and comorbid patientsWhile the management of robust elderly patients should probably be the same as in younger patients, evidence is lacking on the optimal management in older patients with frailty an ACS. The benefit of a routine invasive strategy in older frail patients has been recently investigated in the MOSCA-FRAIL trial.12 An initial conservative approach was a reasonable alternative to a routine invasive strategy among older frail patients with NSTE-ACS. These findings should be validated in larger, adequately powered trials, and the interaction between the burden of frailty and the benefit from an invasive strategy should be investigated.
Moreover, the number of comorbidities such as anemia, chronic kidney disease and neoplasms among patients with ACS is expected to increase due to continuous population aging.13 Most recommendations on ACS management in these special populations have level of evidence C since these patients are almost systematically excluded from clinical trials. Designing clinical trials including these complex patients to assess the impact of different antithrombotic strategies and the role of an invasive strategy is warranted. In this regard, the role of blood transfusion among patients with anemia and ACS remains poorly understood. The REALITY trial14 might be useful to improve clinical practice addressing the potential effect of a restrictive vs liberal strategy while awaiting further powered trials.
Finally, sex and gender differences are well known in ACS but there is a lack of evidence on the benefit, dose, and timing of treatments in women as they are systematically underrepresented in clinical trials. Differences might change after adjustment for confounders; indeed, women with ACS living in high-income countries had a lower postdischarge mortality risk than men in the analysis of EPICOR-EPICOR Asia registries.15 The benefit was attenuated in lower-income countries. Specific research in women with ACS is necessary to adapt their management and improve outcomes.
Therapeutic adherenceThe SECURE trial16 demonstrated an increase in therapeutic adherence and a reduction in events among patients with ACS receiving the polypill including aspirin, ramipril and atorvastatin. Multimodal assessment of therapeutic adherence is now highly recommended. Future studies should include adherence assessment by multimodal and objective methods.
Patient-centered outcomesMost studies analyzing prognosis and the impact of antithrombotic drugs or invasive strategies in older patients with ACS have focused on cardiovascular events as the main endpoint (reinfarction, need for revascularization, or cardiovascular mortality). In this regard, it is important to note that in older ages clinical events are mostly due to noncardiac causes, and assessing noncardiac readmissions and their mortality is crucial. In addition, adapting endpoints to PROMS and PREMS (days alive out-of-hospital, quality of life, patients’ experience) is currently a real need to obtain solid scientific evidence and improve the clinical outcomes of these complex patients in routine clinical practice.
CONCLUSIONSThese comments aim to highlight the new recommendations, improvements, and questions on the implementation of these guidelines in Spain and to identify the gaps in evidence on ACS (figure 1). However, we encourage readers to consult the full text of the ESC 2023 guidelines to delve deeper into specific details and improve their daily practice.
Central illustration. New approach in acute coronary syndrome: person-centered to individualize working diagnosis, invasive management, treatment, and secondary prevention. ACS, acute coronary syndrome; ECG, electrocardiogram; NSTE-ACS, non-ST-elevation acute coronary syndrome; OHCA, out-of-hospital cardiac arrest; STEMI, ST-elevation myocardial infarction.
None.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENo artificial intelligence has been used.
CONFLICTS OF INTERESTThe conflict-of-interest declaration documents of all authors can be seen in the supplementary data.
SEC Working Group for the 2023 ESC guidelines for the management of acute coronary syndromes: Rut Andrea (coordinator), Ana Viana-Tejedor (coordinator), Albert Ariza, Gemma Berga, Roberto Martín-Asenjo, and Sandra O. Rosillo.
SEC Guidelines Committee: José Luis Ferreiro (president), Pablo Avanzas (secretary), Rut Andrea, Araceli Boraita, David Calvo, Raquel Campuzano, Victoria Delgado, Laura Dos Subirá, Juan José Gómez Doblas, María Antonia Martínez Momblan, Pilar Mazón, Domingo Pascual Figal, Juan Sanchis, José María de la Torre Hernández, David Vivas.
See related article: https://secardiologia.es/cientifico/guias-clinicas/cardiopatia-isquemica/14531-2023-esc-guidelines-for-the-management-of-acute-coronary-syndromes.
The names of all the authors of the article are listed in alphabetical order in Appendix A.
Corresponding author.
E-mail addresses:randrea@clinic.cat (R. Andrea); ana_viana_tejedor@hotmail.com (A. Viana-Tejedor).