The betterment of national health care systems should include, in addition to universal access to high-quality medical care independently of socioeconomic level or social background, structural changes with a cross-sectional focus on improving efficiency, productivity, and quality. Care should be geared toward the treatment of chronic conditions and the resolution of health problems at the appropriate care level, avoiding medical interventions that have no added value for the therapeutic or diagnostic process but that still represent a substantial proportion of the health care budget. Barriers to the transformation of health care systems include problems with coordination, both administrative and medical, the scarcity of professional incentives, and the rigidity of our health care organizations. It is thus necessary to identify and focus on opportunities for improvement.
We are convinced that such improvements are only possible through competent and committed clinical leadership that focuses on the individualized resolution of health care problems by introducing processes that guarantee the clinical implementation of diagnostic and therapeutic advances.1 However, we must recognize that, while clinical management is essential to guarantee the quality of the health care service, our current training in this aspect falls short. Accordingly, we should assess the development of skills for the implementation of information systems that include a universal electronic medical record common to the different levels of care. Teamwork is essential, not only among the health care professionals directly involved, but also with administrative staff at other levels and, if possible, experts in system development, implementation, and auditing.2–4 We should be prepared for the incorporation of artificial intelligence into clinical management and, specifically, into the making of decisions affecting care efficiency and quality.5 Practitioners should be integrated into a interconnected network that not only provides information, but also helps us to make and carry out clinical decisions. Artificial intelligence networks are already a reality in many areas of industry and finance and are beginning to make headway in medicine. However, in our profession, direct contact between patients and professionals seems irreplaceable. Nonetheless, we will have to accept a management model based on practitioner-patient interconnections that complement face-to-face interactions, one that helps us to adapt our decisions to the real needs of patients, health organizations, and society in general, under 3 main premises: efficiency, quality care, and transparency.
These considerations aim to promote the implementation of a “virtuous circle” in health care management that includes an electronic record of activity, particularly health outcomes, and the establishment of performance metrics, with external audits of our service. Such audits would not only permit us to obtain a quality accreditation, but also identify opportunities for improvement in all areas of management.
The current health crisis related to the COVID-19 pandemic provides an opportunity to adapt our health care organizations to a new reality that permits another form of clinical management. In this system, resources would be adapted to implement the required telemedicine procedures and promote health care networks that avoid duplication, thereby maximizing efficiency and quality of care.
FROM PROCEDURAL CARDIOLOGY TO HEALTH CARE MANAGEMENTAs mentioned above, clinical management, in our particular case cardiology, which we will call cardiac surgical management here, has a cross-sectional and multifactorial focus built around a central role for the organization of various types of care processes, from the most prevalent to high complexity interventions and support services. The various levels of care involved should also be taken into account in management and decision-making, with incorporation of the best scientific evidence available and with a clear definition of patients’ care pathways within the hospital. In this regard, cardiac surgery units under clinical management are suitable for the following reasons: a) the types of conditions managed; b) the relative independence from other health services in the hospital and the health care system as a whole; c) the various relatively robust quality metrics that are already accepted and available; and d) the socioeconomic impact of heart disease.1 However, our system is more based on the development of processes directed at small areas of our health care, which are sometimes overly specific and often highly technical and even fragmented within the same department. These processes tend to lack cross-sectional integration with other care processes and often fail to take into account continuity of care or transfers between different care levels.
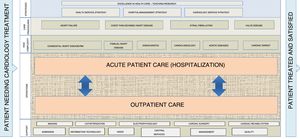
To provide first-class health care, training, and research, all cardiology and cardiac surgery services should have a “process map”, adapted to their specific characteristics. In addition, these departments should be situated within a health care network that includes hospitals of different complexities integrated with primary health care. An outline of a possible process map for a cardiac surgery department or unit is shown in figure 1.
This map must consider the integration of its strategic plan with that of the management area, which should include the hospital and primary care facilities, as well as that of the overall health care service of the autonomous region.
Its organization would affect both acute patients requiring hospitalization, including day hospital and critical heart patients according to Spanish Society of Cardiology recommendations,6 and outpatients whose transfer and continuity of care after hospital discharge should fall within the remit of primary health care and/or nursing.
The availability of health care processes integrated among different levels of care for major diseases entails a definition of patients’ care pathways within the health system. For ischemic heart disease, it would include the management of acute coronary syndrome (ACS), heart failure, and arrhythmias, with special attention given to atrial fibrillation and valve disease. The organization of specific processes for highly complex conditions would include, among others, congenital and hereditary heart diseases, infective endocarditis, cardio-oncology, aortic conditions, and the treatment of cardiac arrest. All should be integrated with the support processes of our speciality, such as cardiac imaging, including advanced techniques (computed tomography and magnetic resonance); catheterization and interventional cardiology; electrophysiology with arrhythmia- and device-related interventions; and cardiac rehabilitation. Regarding cardiac surgery, and in line with the structure of “Heart Teams”, full integration is necessary: cardiology and heart surgery patients are common, as are many of the techniques, and it is thus essential to define the entire cardiac surgery process from first patient contact. As a shared area of medicine, we have always believed that cardiology should be able to evolve from two separate administrative services into a consolidated organization; this would boost efficiency, outcomes, and the incorporation of professionals from other areas, such as anesthetists and intensivists. Unless we do it, no one will.
Regarding support processes, we are clearly embedded within an immense health care system comprising the hospital itself and, in many cases, the managers of each area, including nursing, hospital medicine, and primary care. Respecting the role played by each of the different structural components of the health care organization and considering that chronic conditions and disease prevention are the main challenge faced by our health care system, we must accept that leadership from within the structures of primary care is required to achieve this objective. Management of our needs and outcomes requires a direct relationship with all hospital areas, but we believe that the central element around which everything should turn should be a regular scorecard overview of all of our activities, including a continuous quality analysis of our work.
HEALTH CARE PROCESSES FOR MAJOR DISEASES. ORGANIZATIONAL AND MANAGEMENT CONSIDERATIONSDue to their high prevalence,7 heart diseases are some of the best examples of conditions requiring the definition of a “patient care pathway” in the health care system, both within and beyond the hospital, and including public health services. It is a mistake to believe that a specialization such as cardiology is able to respond to all of the challenges of a health care process for major diseases. In many cases, it can lead to a more fragmented care system, more centered on our own interests than those of the patients or health care organizations. We are convinced that we have the responsibility to bring everyone together—health care professionals, managers, and patients—into a locally adapted organization of our health care processes. At the same time, these care networks should be integrated to avoid duplication, which, at best, increases health care spending and, at worst, creates large care disparities.
Processes should be designed to achieve outcomes at the appropriate care level. Thus, similar to chronic coronary syndromes, ischemic heart disease must include the patient's care pathway from the ACS through to discharge, with consideration of all care transitions. In the case of heart failure, the concept of “heart failure units” should be avoided, given that they are sometimes fragmented among services in the same hospital and without the necessary coordination among emergency care, primary care, and, in particular, nursing care. Regarding arrhythmias, atrial fibrillation would require special attention. Valve diseases should be managed under structural interventions.
On this point, the biggest questions for unit, cardiology, or cardiac surgery managers would be the following. Is the process map suitably defined for the corresponding organization? Do the maps include all of the health care professionals and administrators involved in the management of heart disease for the corresponding area? Are the maps integrated into care networks and have they incorporated telemedicine methods, which are more necessary than ever during the current health crisis? These questions need to be posed because their answers provide the best opportunities for improvement.
MEASUREMENT AS A MEANS TO IMPROVEMENTThe diverse complexity of patients and of the clinical practice organization underlies major variations both in the quality metrics for evaluating the organization of different care processes and in health care outcomes.8,9 Identification of these indicators and their regular compilation is crucial to identify the opportunities for improving the different health care organizations and, specifically, cardiology or integrated cardiovascular services. Multiple publications,10–12 particularly those concerning the management of patients with ACS and heart failure, have highlighted the importance of identifying indicators of health care quality and making them available for common knowledge, always to foster continual improvement. There are sometimes visible differences between centers, even those with the same resources: some find it difficult to accept that an immediate correction is necessary. Nevertheless, considerable evidence shows that measurement in medicine is the best driver of quality.
We often settle for a general analysis (eg, European, Spanish, or regional) but we will only reach those patients who entrust their health to us via the local implementation of a health care organization for which we can be directly responsible. A system for periodic measurement must be established, with appropriate analysis to identify areas amenable to change and, if possible, the implementation of external auditing and accreditation systems. In short, this involves the establishment of what we have already defined as a “virtuous circle” of health care. In our opinion, measurement of the quality of care is one of the best tools for achieving a health care policy that provides for the general population. It would avoid unjustified duplication and oblige us to develop integrated health care networks. It is not enough to scatter health centers throughout an autonomous region with the intention of bringing health care to the average citizen: we all need access to highest-quality health care.
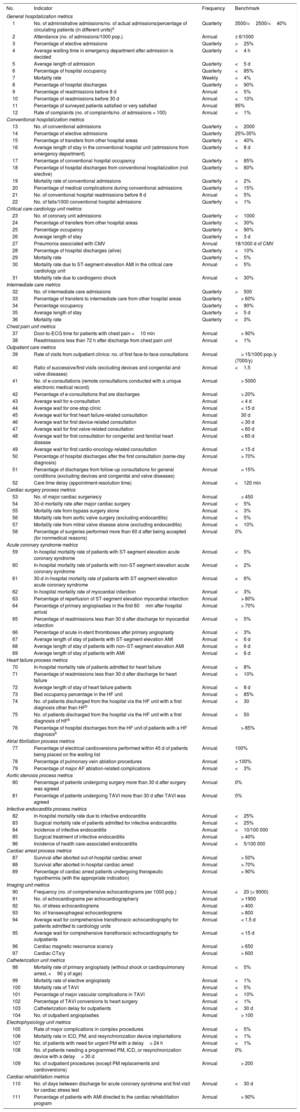
PROPOSAL FOR QUALITY ASSURANCE IN HEALTH CAREHere, we present a proposal for the organization of cardiology care in a Spanish tertiary hospital. It is geared toward both internally integrated processes and those of the different care levels and contains a proposed series of metrics, with prioritization given to those that measure the health care outcomes of our organization.
To identify metrics that reflect the efficiency of our organization, we believe that it is necessary to form a joint commission of members of cardiology and cardiac surgery departments, executive health care management, and external professionals involved in the organization and evaluation/auditing of clinical management. We should identify and clearly define quality metrics, agreeing on the measurement frequency and establishing the appropriate benchmarking standards. To draft these standards, we have followed the recommendations proposed in the consensus document of the Spanish Society of Cardiology and the Spanish Society of Thoracic-Cardiovascular Surgery (INCARDIO)13 and the annual report of resources and health outcomes provided by the Spanish Society of Cardiology (RECALCAR registry),14 as well as data obtained from health care quality evaluations performed by Spanish companies. To obtain these indicators, we need data from the management control system of the health area. This would be linked to the electronic medical records, to the software used for management control of the center, and, when necessary, to the actual records of the cardiology or cardiac surgery department; the latter should be periodically audited, externally, if possible, and by an accredited organization.
In table 1, we have listed 111 quality metrics that we have decided upon for our cardiac surgery unit, showing the metric, the frequency of measurement, the desired benchmark, and the source of the information. The general metrics included concern the following: hospitalization; conventional hospitalization (hospital ward) and critical care cardiology hospitalization (critical care cardiology, intermediate care, and chest pain units) with care metrics for patients with ACS; outpatient care, including e-consulting (interconsultations among primary care physicians through electronic medical records) and the cardiac surgery process; area-specific care processes such as heart failure, atrial fibrillation, aortic stenosis, infective endocarditis, and cardiac arrest; cardiovascular imaging units; catheterization and interventional cardiology units; and electrophysiology and cardiac rehabilitation processes. In general, both in our case and in the area as a whole and specifically for the cardiology department, we will aim to satisfy >90% of the metrics proposed by the executive management of the health care area and >85% of the complete list of 111. We are aware that this proposal needs to be adapted to the characteristics of each health care organization (unit, department, or area), which would require analysis of the resources and health care portfolio available. As we have already mentioned, our model concerns a tertiary hospital with practically all human and material resources allocated to the care of patients with heart disease.
Proposed quality indicators for a cardiology or cardiac surgery department
| No. | Indicator | Frequency | Benchmark |
|---|---|---|---|
| General hospitalization metrics | |||
| 1 | No. of administrative admissions/no. of actual admissions/percentage of circulating patients (in different units)a | Quarterly | 3500/<2500/<40% |
| 2 | Attendance (no. of admissions/1000 pop.) | Annual | ≤ 6/1000 |
| 3 | Percentage of elective admissions | Quarterly | >25% |
| 4 | Average waiting time in emergency department after admission is decided | Quarterly | <4 h |
| 5 | Average length of admission | Quarterly | <5 d |
| 6 | Percentage of hospital occupancy | Quarterly | <85% |
| 7 | Mortality rate | Weekly | <4% |
| 8 | Percentage of hospital discharges | Quarterly | >90% |
| 9 | Percentage of readmissions before 8 d | Annual | <5% |
| 10 | Percentage of readmissions before 30 d | Annual | <10% |
| 11 | Percentage of surveyed patients satisfied or very satisfied | Annual | 95% |
| 12 | Rate of complaints (no. of complaints/no. of admissions × 100) | Annual | <1% |
| Conventional hospitalization metrics | |||
| 13 | No. of conventional admissions | Quarterly | <2000 |
| 14 | Percentage of elective admissions | Quarterly | 25%-35% |
| 15 | Percentage of transfers from other hospital areas | Quarterly | <40% |
| 16 | Average length of stay in the conventional hospital unit (admissions from emergency department) | Quarterly | <8 d |
| 17 | Percentage of conventional hospital occupancy | Quarterly | <85% |
| 18 | Percentage of hospital discharges from conventional hospitalization (not elective) | Quarterly | >80% |
| 19 | Mortality rate of conventional admissions | Quarterly | <2% |
| 20 | Percentage of medical complications during conventional admissions | Quarterly | <15% |
| 21 | No. of conventional hospital readmissions before 8 d | Annual | <5% |
| 22 | No. of falls/1000 conventional hospital admissions | Quarterly | <1% |
| Critical care cardiology unit metrics | |||
| 23 | No. of coronary unit admissions | Quarterly | <1000 |
| 24 | Percentage of transfers from other hospital areas | Quarterly | <30% |
| 25 | Percentage occupancy | Quarterly | <90% |
| 26 | Average length of stay | Quarterly | <3 d |
| 27 | Pneumonia associated with CMV | Annual | 18/1000 d of CMV |
| 28 | Percentage of hospital discharges (alive) | Quarterly | <10% |
| 29 | Mortality rate | Quarterly | <5% |
| 30 | Mortality rate due to ST-segment elevation AMI in the critical care cardiology unit | Annual | <5% |
| 31 | Mortality rate due to cardiogenic shock | Annual | <30% |
| Intermediate care metrics | |||
| 32 | No. of intermediate care admissions | Quarterly | >500 |
| 33 | Percentage of transfers to intermediate care from other hospital areas | Quarterly | > 60% |
| 34 | Percentage occupancy | Quarterly | <90% |
| 35 | Average length of stay | Quarterly | <5 d |
| 36 | Mortality rate | Quarterly | <3% |
| Chest pain unit metrics | |||
| 37 | Door-to-ECG time for patients with chest pain <10 min | Annual | > 90% |
| 38 | Readmissions less than 72 h after discharge from chest pain unit | Annual | <1% |
| Outpatient care metrics | |||
| 39 | Rate of visits from outpatient clinics: no. of first face-to-face consultations | Annual | > 15/1000 pop./y (7000/y) |
| 40 | Ratio of successive/first visits (excluding devices and congenital and valve diseases) | Annual | <1.5 |
| 41 | No. of e-consultations (remote consultations conducted with a unique electronic medical record) | Annual | > 5000 |
| 42 | Percentage of e-consultations that are discharges | Annual | > 20% |
| 43 | Average wait for e-consultation | Annual | < 4 d |
| 44 | Average wait for one-stop clinic | Annual | < 15 d |
| 45 | Average wait for first heart failure-related consultation | Annual | 30 d |
| 46 | Average wait for first device-related consultation | Annual | < 30 d |
| 47 | Average wait for first valve-related consultation | Annual | < 60 d |
| 48 | Average wait for first consultation for congenital and familial heart disease | Annual | < 60 d |
| 49 | Average wait for first cardio-oncology-related consultation | Annual | < 15 d |
| 50 | Percentage of hospital discharges after the first consultation (same-day diagnosis) | Annual | > 70% |
| 51 | Percentage of discharges from follow-up consultations for general conditions (excluding devices and congenital and valve diseases) | Annual | > 15% |
| 52 | Care time delay (appointment-resolution time) | Annual | <120 min |
| Cardiac surgery process metrics | |||
| 53 | No. of major cardiac surgeries/y | Annual | > 450 |
| 54 | 30-d mortality rate after major cardiac surgery | Annual | <5% |
| 55 | Mortality rate from bypass surgery alone | Annual | <3% |
| 56 | Mortality rate from aortic valve surgery (excluding endocarditis) | Annual | <5% |
| 57 | Mortality rate from mitral valve disease alone (excluding endocarditis) | Annual | <10% |
| 58 | Percentage of surgeries performed more than 60 d after being accepted (for nonmedical reasons) | Annual | 0% |
| Acute coronary syndrome metrics | |||
| 59 | In-hospital mortality rate of patients with ST-segment elevation acute coronary syndrome | Annual | <5% |
| 60 | In-hospital mortality rate of patients with non-ST-segment elevation acute coronary syndrome | Annual | <2% |
| 61 | 30-d in-hospital mortality rate of patients with ST-segment elevation acute coronary syndrome | Annual | <6% |
| 62 | In-hospital mortality rate of myocardial infarction | Annual | <3% |
| 63 | Percentage of reperfusion of ST-segment elevation myocardial infarction | Annual | > 80% |
| 64 | Percentage of primary angioplasties in the first 60min after hospital arrival | Annual | > 70% |
| 65 | Percentage of readmissions less than 30 d after discharge for myocardial infarction | Annual | <5% |
| 66 | Percentage of acute in-stent thromboses after primary angioplasty | Annual | <3% |
| 67 | Average length of stay of patients with ST-segment elevation AMI | Annual | <6 d |
| 68 | Average length of stay of patients with non–ST-segment elevation AMI | Annual | <6 d |
| 69 | Average length of stay of patients with AMI | Annual | <6 d |
| Heart failure process metrics | |||
| 70 | In-hospital mortality rate of patients admitted for heart failure | Annual | <8% |
| 71 | Percentage of readmissions less than 30 d after discharge for heart failure | Annual | <10% |
| 72 | Average length of stay of heart failure patients | Annual | <8 d |
| 73 | Bed occupancy percentage in the HF unit | Annual | <85% |
| 74 | No. of patients discharged from the hospital via the HF unit with a first diagnosis other than HFb | Annual | <30 |
| 75 | No. of patients discharged from the hospital via the HF unit with a first diagnosis of HFb | Annual | <50 |
| 76 | Percentage of hospital discharges from the HF unit of patients with a HF diagnosisb | Annual | > 85% |
| Atrial fibrillation process metrics | |||
| 77 | Percentage of electrical cardioversions performed within 45 d of patients being placed on the waiting list | Annual | 100% |
| 78 | Percentage of pulmonary vein ablation procedures | Annual | > 100% |
| 79 | Percentage of major AF ablation-related complications | Annual | <3% |
| Aortic stenosis process metrics | |||
| 80 | Percentage of patients undergoing surgery more than 30 d after surgery was agreed | Annual | 0% |
| 81 | Percentage of patients undergoing TAVI more than 30 d after TAVI was agreed | Annual | 0% |
| Infective endocarditis process metrics | |||
| 82 | In-hospital mortality rate due to infective endocarditis | Annual | <25% |
| 83 | Surgical mortality rate of patients admitted for infective endocarditis | Annual | <25% |
| 84 | Incidence of infective endocarditis | Annual | <10/100 000 |
| 85 | Surgical treatment of infective endocarditis | Annual | > 40% |
| 86 | Incidence of health care-associated endocarditis | Annual | <5/100 000 |
| Cardiac arrest process metrics | |||
| 87 | Survival after aborted out-of-hospital cardiac arrest | Annual | > 50% |
| 88 | Survival after aborted in-hospital cardiac arrest | Annual | > 70% |
| 89 | Percentage of cardiac arrest patients undergoing therapeutic hypothermia (with the appropriate indication) | Annual | > 90% |
| Imaging unit metrics | |||
| 90 | Frequency (no. of comprehensive echocardiograms per 1000 pop.) | Annual | <20 (< 9000) |
| 91 | No. of echocardiograms per echocardiographer/y | Annual | > 1900 |
| 92 | No. of stress echocardiograms | Annual | > 400 |
| 93 | No. of transesophageal echocardiograms | Annual | > 800 |
| 94 | Average wait for comprehensive transthoracic echocardiography for patients admitted to cardiology units | Annual | < 1.5 d |
| 95 | Average wait for comprehensive transthoracic echocardiography for outpatients | Annual | < 15 d |
| 96 | Cardiac magnetic resonance scans/y | Annual | > 650 |
| 97 | Cardiac CTs/y | Annual | > 600 |
| Catheterization unit metrics | |||
| 98 | Mortality rate of primary angioplasty (without shock or cardiopulmonary arrest, <90 y of age) | Annual | <5% |
| 99 | Mortality rate of elective angioplasty | Annual | <1% |
| 100 | Mortality rate of TAVI | Annual | <5% |
| 101 | Percentage of major vascular complications in TAVI | Annual | <10% |
| 102 | Percentage of TAVI conversions to heart surgery | Annual | <1% |
| 103 | Catheterization delay for outpatients | Annual | <30 d |
| 104 | No. of outpatient angioplasties | Annual | > 100 |
| Electrophysiology unit metrics | |||
| 105 | Rate of major complications in complex procedures | Annual | <5% |
| 106 | Mortality rate in ICD, PM, and resynchronization device implantations | Annual | <1% |
| 107 | No. of patients with need for urgent PM with a delay> 24 h | Annual | <1% |
| 108 | No. of patients needing a programmed PM, ICD, or resynchronization device with a delay> 30 d | Annual | 0% |
| 109 | No. of outpatient procedures (except PM replacements and cardioversions) | Annual | > 200 |
| Cardiac rehabilitation metrics | |||
| 110 | No. of days between discharge for acute coronary syndrome and first visit for cardiac stress test | Annual | <30 d |
| 111 | Percentage of patients with AMI directed to the cardiac rehabilitation program | Annual | > 90% |
AF, atrial fibrillation; AMI, acute myocardial infarction; CMV, controlled mechanical ventilation; CT, computed tomography; HF, heart failure; ICD, implantable cardioverter-defibrillator; PM, pacemaker; pop., population; TAVI, transcatheter aortic valve implantation.
Based on the premise that what is not measured does not exist, we are convinced that these kinds of proposals not only help us to determine the quality and the efficiency of our health care activity, but also permit us to both identify opportunities for improvement in health care management programs and recognize concrete quality objectives for cardiology patient care. The comparison of our results with those of referral centers in the area is another of the possibilities that can only be performed with measurement of our activity, which should be included in the “virtuous circle” formed by measurement, comparison with a standard of excellence, internal and external auditing of outcomes, and identification of opportunities for improvement.
As mentioned above, we believe that the COVID-19 pandemic has drastically altered the provision of care to patients with different conditions in many centers, including cardiovascular care. Therefore, management programs that permit us to restore health care, both acute and elective, are more necessary than ever. The present situation presents an opportunity to reflect on the changes required by each area and the establishment of systems that focus on the efficiency and quality of our health care services.
CONFLICTS OF INTERESTThe authors declare that they have no conflicts of interest in relation to the current document.