Bifurcation lesions constitute a common group of lesions encountered on a daily basis in the catheterization laboratory.1 Although they are considered complex lesions, their management has favorably evolved in the last 10 to 15 years, with a new generation of highly effective stents now available. At the same time, the therapeutic strategy has been regulated and standardized,2 which has improved the success rates compared with previous years. Thus, all types of bifurcations can now be safely managed, including those of left main coronary artery disease.3
Bifurcation lesions can appear in different clinical and anatomical contexts. Among the former, they can cause stable angina or acute coronary syndromes. Regarding the latter, these lesions can concur with additional anatomical complexities, such as severe calcifications, diffuse lesions, thrombotic lesions, or chronic occlusions.4,5
There is little clinical information on bifurcations causing ST-segment elevation acute myocardial infarction (STEMI)6,7 because STEMI is itself a reason for patient exclusion in many randomized studies. However, 2 recent studies published in Revista Española de Cardiología have shed light on the field of bifurcation lesions causing STEMI.8,9
The first, by Salinas et al.,8 studied a series of 274 patients with STEMI and bifurcation lesions causing the infarction. The results of percutaneous treatment were compared with those of a control group of 2472 patients via propensity score matching and a 5-year follow-up. The main finding of the study is that patients with and without a bifurcation lesion in STEMI showed similar short- and long-term prognoses.
In the second study, Choi et al.9 attempted to determine the best strategy for the percutaneous treatment of bifurcation lesions causing STEMI in patients treated with primary angioplasty. To do this, the authors analyzed a series of 367 patients with STEMI and a culprit bifurcation lesion treated with either a simple (1 stent) or complex (2 stents) strategy. After comparing the clinical outcomes of the 2 groups of patients, they concluded that patients treated with a complex 2-stent strategy had a higher rate of major events during follow-up than those treated with a single stent (simple strategy).
Thus, although the 2 studies had different clinical objectives, both explored the same topic. Salinas et al. show that the long-term outcome (5 years) of patients with bifurcation lesions causing STEMI is similar to that of those with nonbifurcated lesions. Their work is valuable because it contains one of the most extensive series in the literature, is the only one with a propensity score-matched control group, and has the longest follow-up. The results are in line with those of previous publications reaching the same conclusions.6,7
Choi et al. compared the simple and complex treatment strategies for bifurcation lesions causing STEMI. This work is interesting due to the shortage of previous studies addressing the best treatment strategy for this type of patient with bifurcation lesions. Although many comparative studies have been published of simple and complex treatment strategies for bifurcation lesions, the subgroup of patients with STEMI has not been addressed in detail or has even been excluded from most of the studies. Only a small substudy of the DKCRUSH II trial10 specifically analyzed this subgroup of patients. With 30 and 33 patients in each respective group, the authors concluded that there were no significant differences between the 2 strategies. In contrast, the results of Choi et al. indicate that the simple 1-stent strategy achieves better results and has a lower incidence of events during follow-up than the complex strategy. These findings are consistent with those of most randomized studies in patients with bifurcation lesions outside the context of STEMI. However, some limitations of this study should be mentioned. The group of patients treated with 2 stents had some more unfavorable baseline and procedural clinical and angiographic characteristics than the group of patients treated with 1 stent. Although the authors attempted to correct this imbalance between the groups using a complicated statistical technique (inverse probability of treatment weighting, that is, weighting by the inverse of the probability of treatment), these results should be carefully considered and should not be interpreted in the same way as those obtained in randomized studies. Another limitation of this registry is that the vast majority of patients were managed with first-generation drug-eluting stents. These devices are no longer available and had a higher rate of long-term events than the currently used latest-generation drug-eluting stents.11–13 Therefore, the findings of this article should be cautiously extrapolated to current clinical practice.
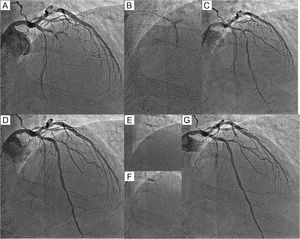
Despite these limitations, the work by Choi et al. is one of the few to compare the simple and complex treatment strategies for bifurcation lesions in the context of STEMI. Their results are similar to those of randomized studies conducted outside the STEMI setting, and their conclusions are in line with the usual practice of most catheterization laboratories and the current recommendations of the European Bifurcation Club.1 Thus, the provisional stent technique (Figure 1), as in other clinical situations, should be the treatment of choice for these bifurcation lesions with STEMI. The strategy can be summarized as follows:
- •
Once the main vessel has been recanalized, a guidewire should be placed in the side branch (Figure C, jailed guidewire technique).14 The size of the stent depends on lesion length and distal vessel diameter. After implantation, a proximal optimization technique (POT) must be performed, which involves dilatation of the proximal part of the stent with a short balloon to a diameter larger than that of the rest of the stent. In this way, the proximal stent is adapted to a vessel with a larger diameter than the distal part of the bifurcation. At this point, the state of the side branch origin must be assessed; if there is no significant stenosis or if the vessel is very small with a Thrombolysis in Myocardial Infarction (TIMI) grade 3 flow, the procedure is complete. In patients with a compromised origin in a significant branch (Figure D), a second guidewire must be passed to the branch to treat it at the same time as removal of the jailed guidewire. The balloon can be inflated at the same time as that of another balloon in the main vessel (kissing balloon) or by itself.15 A second POT (Figure F) is recommended, particularly if simultaneous inflation has not been performed. For most bifurcations, a good outcome is obtained with all of these maneuvers (Figure G). However, in a variable percentage of cases, a suboptimal result is obtained in the side branch origin and it is necessary to implant a second stent followed by a final kissing balloon.2
A: baseline angiogram of ST-segment elevation acute myocardial infarction; occlusion of the anterior descending artery and the diagonal branch. B: balloon dilatation of the anterior descending artery. C: artery with a lesion in a recanalized bifurcation and a jailed guidewire in the diagonal branch. D: angiogram after stent implantation in the anterior descending artery and the proximal optimization technique (POT). E: balloon dilation of the diagonal branch. F: second POT. G: final result.
In conclusion, bifurcation lesions causing acute coronary syndromes can be connected to additional anatomical complexities that can affect the outcomes of their percutaneous treatment. However, based on these 2 important articles, we can answer the question posed in the title and state that bifurcation lesions causing STEMI are not a different animal from bifurcation lesions in other clinical contexts.
CONFLICTS OF INTERESTM. Pan has received minor payments from Abbott for presentations.
.