Background
Coronary bifurcation lesions are frequently observed in the catheterization laboratory and currently account for 15 to 20% of stenting procedures. The systematic use of drug-eluting stents (DES) in Rotterdam1 was associated with an increase from 8 to 16% in the number of bifurcation lesions being stented over a one-year period. This high incidence of coronary bifurcation lesions can be explained by the propensity for atherosclerosis to develop at branch points because of turbulence and high shear stress. Bifurcation lesions are also frequently under-appreciated for many reasons: special angulated views are required for visualization of the side branch ostium which can be hidden under the main vessel or overlapping branches. Moreover, many cases which were not originally considered bifurcation lesions, because only 1 branch was initially involved, ultimately turn into a true bifurcation case during the intervention. These "unexpected" bifurcation lesions are adjacent to a branch point and, in such cases, the side branch almost always becomes involved in the course of the angioplasty due to axial or circumferential plaque redistribution.
The accurate definition of a bifurcation lesion is a real issue. Indeed, the importance of a secondary branch cannot be measured by its reference diameter only. Other parameters such as length of the branch, size of the vascularized territory, left ventricular function and operator experience must also be taken into account. One way around the problem is to consider as a bifurcation lesion any lesion associated with a side branch, next to the main branch lesion, which the operator cannot afford to lose.
Consequently, operators must accurately visualize the configuration of a diseased coronary bifurcation in several views before starting the procedure in order to be able to delineate an optimal strategy.
Prior to the introduction of coronary stents, despite gradual equipment improvements and enhancements in technical approach, such as kissing balloon inflation, the immediate and mid term results of balloon angioplasty for bifurcation disease were relatively disappointing and the presence of a bifurcation lesion with a significant side branch constituted a frequent indication for coronary artery surgery. "Debulking" techniques, such as directional or rotational atherectomy, which were in vogue in the early 1990's, did not significantly improve outcomes of bifurcation angioplasty.
The Era of Bare Metal Stents (BMS)
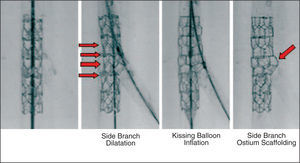
As early as 1992, it became clear that coronary stenting combined with dual anti-platelet agents would become the treatment of choice in the majority of coronary lesions. Nevertheless, the results of early experiences with first-generation stents in bifurcation lesions were relatively poor. More recent studies using second or third-generation stents have shown that coronary bifurcation stenting has gradually become an alternative treatment to coronary surgery, and that it is associated with acceptable immediate and mid-term results. Currently, in experienced centers using BMS, the angiographic success rate is >95% for the main branch and >88% for both branches with a MACE rate at 6 to 12 month follow-up of 18%-35% including a TVR rate of 12% to 28%. Many approaches involving techniques (Figure 1) of varying complexity,2-9 using 2 and even 3 stents have been proposed (culotte, simultaneous kissing stent, skirt stent). However, the simplest of these approaches using BMS (provisional side branch T stenting with final kissing balloon inflation) rapidly proved to be associated with the best mid-term outcome.10-14
Figure 1. Strategies for stenting bifurcation lesions.
Lessons From Bench Testing
The most important lessons stem from the finding that the opening of struts towards the side branch (Figure 2), results in stent deformation at the main branch level opposite the ostium of the side branch. This contributed to major strategic changes in the approach to bifurcation treatment. Indeed, final kissing inflation, by re-apposing the stent against the vessel wall, may reduce the risk of stent thrombosis as well as the occurrence of restenosis, especially when DES are implanted.15
Figure 2. Stent deformation.
The second finding which now seems obvious is that the opening of struts towards the side branch results in at least partial coverage of the side branch ostium (Figure 2). Thus, given the fact that in the majority of coronary bifurcation cases there is no side branch involvement at the beginning of the procedure (false bifurcation) or only ostial involvement in the majority of true bifurcation lesions, placement of a single stent followed by final kissing inflation may constitute an optimal treatment of the lesion in the majority of cases. Whatever the technique used, a thorough knowledge of these phenomena is essential in delineating the optimal treatment strategy and in paving the way for development of new dedicated systems.
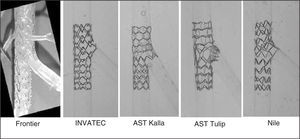
Dedicated Devices
Dedicated devices providing easy side branch access throughout the procedure, good side branch ostial scaffolding and allowing provisional side branch T stenting (Figure 3) are currently being developed. The MultiLink Frontier stent (Guidant Corporation) has been evaluated in a pilot study of 105 patients. Procedural success was obtained in 93% of cases and at 6 months the cumulative MACE rate was 17% (including a TLR of 13%). There were no deaths and no stent thrombosis. A new generation of DES multilink Frontier stent will be evaluated in 2005. A comparable approach has been developed by Advanced Stent Technologies with the SLK-View stent and more recently the Petal stent which is currently being evaluated. A new dedicated stent and delivery system manufactured by INVATEC is also under evaluation in a small pilot European dual center study. A self-expanding nitinol drug eluting stent (DEVAX) designed for bifurcation lesions employs a reverse tapering conical design to spread the carina, theoretically decreasing plaque shift into the side branch to avoid the necessity for side branch stenting. This device is currently under evaluation in a European multicenter Registry. These new devices will probably simplify the technical approach and, hopefully, make bifurcation stenting easy for everybody.
Figure 3. Dedicated devices for bifurcation lesions.
Drug-Eluting Stents for Bifurcation Lesions
The next advance in the interventional treatment of bifurcation lesions involves the prevention of restenosis with drug-eluting stents. However, the problem raised by the technical approach has not yet been solved and new techniques such as modified T stenting, crush or simultaneous kissing stent have been proposed in order to simplify the technical approach and reduce the risk of side branch restenosis. The crush technique consists in wiring both branches of the bifurcation which are preferably predilated. The first stent is advanced into the side branch. A second stent is advanced into the main branch to cover fully the bifurcation. The side branch stent is retracted into the main vessel so that its proximal edge is 4-5 mm proximal to the carina and then expanded at high pressure. The side branch stent delivery balloon and guidewire are removed. The main branch stent is then expanded and "crush" the side branch stent proximal to the carina. Rewiring the side branch through the main branch and crushed side branch stent with final kissing balloon inflation is strongly recommended. However, recent published data16-21 did not demonstrate any benefit associated with these techniques. An excess of restenosis was observed when using 2 stents as well as an increased risk of stent thrombosis.
Contribution of the Present Study
The study by Pan et al22 published in this issue of Revista Española de Cardiología confirms that the implementation of the strategy of provisional side branch T stenting results in a very low risk of restenosis. Indeed, the results of this study conducted in patients presenting with true bifurcation lesions show that the risk of restenosis was 3.6% in the main branch and 1.8% in the side branch with a rate of side branch stenting of only 29%. Another interesting finding of this study, in which patients had angiographic and IVUS follow-up at 6 months, is that there was a certain degree of stent underexpansion under the side branch origin. Even if such relatively inadequate expansion of the stent underneath the side branch origin may increase the risk of restenosis and thrombosis, the authors only report a single case of restenosis at this level and no case of stent thrombosis. Similar observations were made in the sirolimus bifurcation study23 as well as in more general settings.
The degree of poor stent expansion distal to the side branch origin using a provisional side branch T-stenting strategy observed by Pan et al22 seems to be magnified when the crush technique is applied as pointed out in recent publications19-21 and, currently, final kissing balloon inflation is strongly recommended in combination with this technique.
Caveats
The fact that the performance of final kissing inflation does not alter these data with the provisional T stenting approach is rather surprising. The small number of patients included in the study and the absence of randomization could account for the absence of significant differences. Another explanation may lie in the fact that, in cases where kissing inflation was not performed, the strategy and successive dilatation phases in the main branch and side branch are unknown. One could hypothesize that when final kissing inflation was not performed, operators decided to perform a final dilatation in the main branch which may have corrected stent deformation due to the opening of the side branch as efficiently as kissing inflation. Furthermore, it is possible that in some cases, the stent strut toward the side branch was not opened due to the fact that predilatation of the side branch was systematically performed in the study before main branch stenting indeed, in such a case, stent deformation is not likely to occur.
Implications
These data are consistent with those currently available in the DES literature showing that the strategy of provisional side branch T stenting in the treatment of coronary bifurcation lesions is associated with a very low rate of restenosis and an excellent safety profile compared with other more sophisticated strategies. The question as to whether final kissing inflation should be performed remains unanswered and only a randomized study could provide an answer. However, it is certain that when the struts of a stent are opened toward the side branch, the subsequent main branch stent deformation observed in bench tests should lead operators to complete the procedure by performing final balloon inflation at least in the main branch stent.
Correspondence: Dr. T. Lefèvre.
Institut Cardiovasculaire Paris Sud.
Rue du Noyer Lambert. 91300 Massy. Francia.
E-mail: t.lefevre@icps.com.fr