Keywords
INTRODUCTION
Cardiac arrhythmias and conduction disturbances constitute a major group of heart diseases. Over the past 15 years, we have observed spectacular advances in our knowledge of arrhythmogenic substrates and of the mechanisms that trigger and contribute to the maintenance of arrhythmias, as well as the development of therapeutic approaches and implantable devices that have revolutionized the management of these diseases. However, with the exception of atrial fibrillation (AF), which has been the subject of numerous population-based studies that enable us to estimate the true frequency of this arrhythmia,1-4 there has been no parallel development in the knowledge of the prevalence and incidence of the rest of these diseases. Due to the lack of information, the real importance of the problem and the demands of the management of these diseases continues to be little known from the point of view of the population and health care in terms of both the allocation of material and human resources and the devising of training programs for specialists.
The objective of our study was to analyze the incidence (existing and newly diagnosed cases) of cardiac arrhythmias and conduction disturbances in a general cardiology clinic. We also proposed to determine the percentage of our patients who require referral to units specialized in the management of arrhythmias because of evidence that they might benefit from an electrophysiological study (EPS) and/or device implantation.
PATIENTS AND METHODS
We analyzed the rhythm or conduction disturbances in 2045 patients who came to the cardiology outpatient clinic of our center on those days on which the authors responsible for data collection (Drs Vázquez and Muñoz) were present. This situation was conditioned exclusively by organizational aspects of the unit and in no case by clinical considerations; thus, the sample was representative of the patients that come to our clinics. These patients are sent to us from primary care centers, for consultations requested by other hospital services and for check-ups scheduled by the cardiologists themselves. All the cardiology units in the health care area of our center depend on our service. Thus, the only means of being referred to cardiology from primary care is through our outpatient clinic. Moreover, none of our units are devoted exclusively to a given heart disease. As we have no electrophysiology laboratory in our hospital, we have to refer patients to other centers; however, all of them continue to be followed in our clinic, although some of them are being seen simultaneously at their hospitals of origin, mainly for monitoring of implanted devices. If a patient came to our clinic more than once during the period of data collection (November 2003 to June 2004), only the first visit was considered.
In addition to the analysis of the presence of arrhythmias and conduction disturbances in all the patients enrolled, we determined the prevalence of these diseases in the 704 patients (34.4%) who were being assessed in a cardiology clinic for the first time.
A patient was considered to present an arrhythmia when the in-office electrocardiographic recording, that provided by the patient or the Holter recording revealed any of the following rhythm disturbances: AF, common atrial flutter, regular narrow QRS tachycardia with no evidence of common atrial flutter, and sustained or nonsustained ventricular tachycardia. Ventricular tachycardia was considered to be any regular tachycardia with a wide QRS complex or one that differed from that of baseline rhythm and sustained tachycardia was that which lasted more than 30 seconds or required termination by means of some type of therapeutic technique. We included in the analysis those patients with an ejection fraction (EF) less than 30% due to ischemic disease, even in the absence of arrhythmias, as we considered that they should be assessed from the perspective of the prevention of arrhythmia-induced sudden death. Those patients with supraventricular or ventricular premature beats, regardless of their frequency, were excluded and those presenting frequent, highly symptomatic ventricular premature beats and requiring drug treatment were included only exceptionally. Atrial fibrillation was classified according to the clinical patterns established in the joint document of the American Heart Association, the American College of Cardiology and the European Society of Cardiology.5
The presence of second-degree or higher grade atrioventricular (AV) block, bifascicular block, or complete right bundle branch block was considered a conduction disturbance. Patients with sick sinus syndrome were also included. We established as a possible indication for EPS and/or device implantation a clinical picture compatible with class I or IIa recommendations according to any of the clinical practice guidelines of the American cardiology associations, the European Society of Cardiology or the Spanish Society of Cardiology, even in cases in which patient age, comorbidity or the personal criteria of the responsible cardiologist resulted in this option not being recommended to the patient or the refusal on the part of the patient. On the basis of these criteria, possible indications for EPS and/or device implantation were considered to be the following conditions: regular narrow QRS tachycardia,6 atrial flutter,6 an EF less than 30% due to ischemia, even in the absence of documented arrhythmias,7,8 symptomatic ventricular arrhythmias in the presence of structural heart disease,9 cardiogenic syncopal episodes in the presence of left ventricular systolic dysfunction of any etiology, even in the absence of documented arrhythmias,10 and cardiogenic syncopal episodes in the presence of third-degree intraventricular block.10,11
A real indication of EPS and/or device implantation was recorded when the procedure had already been carried out or was indicated on the day of the visit.
Patients considered to be diabetic, hypertensive or dyslipidemic were those for whom drug treatment aimed at correcting these diseases had been recommended. A rheumatic valvular lesion of any degree of severity was recorded as valve disease. Valvular lesions of any other etiology were reported as valve disease only if the degree of severity was greater than mild. In order for the disease to be considered ischemic, we required a previous diagnosis of myocardial infarction, a coronary angiographic study showing obstructive lesions or a clinical picture of typical angina pectoris considered as such by at least 2 cardiologists. Those patients who were active smokers at the time of the consultation, or had been within the preceding three months, were considered to be smokers, while ex-smokers were those who had given up smoking 10 years earlier. Antiarrhythmic medication did not include beta-blockers and implantable devices did not include pacemakers.
RESULTS
In all, 798 patients (39%) presented one or more of the rhythm and conduction disturbances under consideration. The clinical characteristics of all the patients appear in Table 1. Table 2 shows the rhythm and/or conduction disturbances detected.
Atrial Fibrillation
Atrial fibrillation was the arrhythmia most frequently encountered. It was present in one of every four patients in our study population, constituting two thirds of the arrhythmias or conduction disturbances diagnosed. Of these patients, 45.4% were men and the mean age was 69.8±10 years; 300 of the 524 (57%) did not present structural heart disease; the arrhythmia accompanied a valve disease in 150 patients (29%, rheumatic in 112 cases), coronary artery disease in 46 (9%), dilated cardiomyopathy in 17 (3%), and other diseases (hypertrophic cardiomyopathy, chronic constrictive pericarditis, congenital heart disease and heart failure with preserved systolic function) in 11 (2%). After being seen, 75.2% of the patients (394 of 524) continued or began anticoagulant therapy.
The patterns of clinical presentation of arrhythmia, patient age, comorbidity and the use of anticoagulants according to each of the clinical patterns are shown in Table 3.
Electrical cardioversion had previously been performed or was considered to be indicated at the time of consultation in 43 patients (8.2%) and 78 (15%) were receiving antiarrhythmic therapy (flecainide in 38 cases, amiodarone in 36, propafenone in 3 and sotalol in 1). EPS had been carried out or was indicated in 17 patients, although this procedure was proposed for the treatment of accessory pathways, atrial flutter, AV node ablation, or concomitant ventricular arrhythmias; in only 1 case was it proposed for the treatment of AF.
Atrial Flutter
Common atrial flutter was detected in 34 patients, in two of whom it was permanent. The mean patient age was 71.8±9 years and 61.8% of those affected were men. Although 70.6% of the patients presented no structural heart disease, 62% (n=21) were hypertensive and 29% (n=10) were diabetic. Three patients had undergone electrical cardioversion. EPS had been performed in 7 (for ablation of a cavotricuspid isthmus in 5, for AV node ablation due to uncontrollable AF in 1 and for implantation of an automatic defibrillator and performance of biventricular stimulation due to severe systolic dysfunction of ischemic origin and heart failure in one). Cavotricuspid isthmus ablation was recommended for 6 patients on the day of their visit.
In 21 cases (61.7%), the flutter was associated with AF; 7 patients (21%) were receiving antiarrhythmic therapy, and 16 (47%), anticoagulant therapy.
Regular Narrow QRS Tachycardia
Fifty-eight patients were diagnosed as having regular tachycardia with narrow QRS complex that did not meet the criteria for common flutter; in 8 (14%), surface electrocardiogram revealed the presence of permanent or intermittent Wolff-Parkinson-White syndrome. The mean age was 57±16.8 years (range, 14 to 83 years) and 21 patients (36%) were men. In 83%, there was no evidence of structural heart disease; coronary artery disease was documented in 9%, valve disease in 3% and congenital heart disease in 2%. Nearly half of the patients (n=28) were hypertensive and 7% were diabetic. One patient had undergone electrical cardioversion, and EPS had been performed or was indicated in 29 (50%), in every case, for the purpose of carrying out radiofrequency ablation of the arrhythmogenic substrate. Nine patients (16%) were receiving antiarrhythmic therapy.
Ventricular Arrhythmias and/or Ejection Fraction Less Than 30% Due to Ischemia
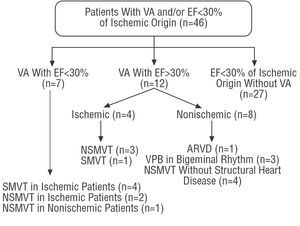
Ventricular arrhythmias and/or an EF less than 30% due to ischemia was detected in 46 cases. Figure 1 shows the distribution of these patients.
Figure 1. Distribution of the patients with ventricular arrhythmias and/or ejection fraction less than 30% of ischemic origin according to the disease detected. ARVD indicates arrhythmogenic right ventricular dysplasia; EF, ejection fraction; NSMVT, nonsustained monomorphic ventricular tachycardia; SMVT, sustained monomorphic ventricular tachycardia; VA, ventricular arrhythmias; VPB, ventricular premature beats.
Four of the 27 patients with an EF less than 30% without documented arrhythmias had a QRS complex of more than 120 ms. The patients with ventricular premature beats were included because this disturbance was accompanied by nonsyncopal symptoms, was very often coupled with bigeminal rhythm and required treatment with beta-blockers.
Eleven patients (24%) had automatic defibrillators, 3 of them with biventricular stimulation; EPS was indicated in another 2 at the time of their visit. One patient had undergone electrical cardioversion and 6 (13%) were receiving antiarrhythmic therapy.
The mean age of the patients with coronary artery disease was 72±9.1 years (range, 35 to 86 years) and 10 of them (27%) were over 75 years of age. In this group, 92% of the patients were men, 43% were hypertensive, 35% were diabetic, 8% were smokers, and 54% were ex-smokers.
Intraventricular Conduction Disturbances
Intraventricular block was, after AF, the most prevalent disturbance and was diagnosed in 157 patients. The incidence of each electrocardiographic pattern, the clinical characteristics and accompanying diseases appear in Table 4.
Two patients had undergone an EPS, which was indicated in another 5 after their visit. Two patients were receiving biventricular stimulation, one of them with a defibrillating device.
Changes in Sinus Node Function and Atrioventricular Conduction
A total of 58 patients had permanent pacemakers, 2 presented asymptomatic second-degree AV block and 7, sinus node dysfunction unrelated to syncope. Among the patients with pacemakers, 28 (42%) presented AF, and 6 (10%) had an EF less than 40%.
The mean age in this group of patients was 70.2±11.3 years, 54% were men, 43% were hypertensive, 22% were diabetics, and 54% had no structural heart disease.
Other Disturbances
Two patients presented syncopal symptoms and an EF less than 30% of nonischemic origin, in the absence of documented ventricular arrhythmias or conduction disturbances; EPS was indicated in both cases. One patient had a cardiac event recorder inserted to control repeated syncopal episodes of unknown etiology, in the absence of structural heart disease and rhythm or conduction changes. Finally, 1 patient had an electrocardiographic recording compatible with Brugada syndrome in the absence of symptoms or family history of sudden death, and no additional examinations were requested.
Incidence of Rhythm or Conduction Changes in Patients Being Seen for the First Time in a Cardiology Unit
Of the 704 patients who had never been seen in a cardiology clinic, 153 (22%) presented 1 or more of the rhythm and conduction disturbances being analyzed. The mean age was 68.3±13 years and 52% of the patients were men, 82% presented no structural heart disease, 13% had a valve disease, 2% had an ischemic disease, and 5 patients (3%) had an EF less than 40%. Their distribution according to the different diseases detected is shown in Table 5.
In 33 of the 81 patients with AF (41%), the attempt to achieve sinus rhythm was not considered to be indicated and it was decided to initiate treatment for permanent AF. Thirty-six patients (44%) were in sinus rhythm at the time they were examined and electrical cardioversion was indicated in the remaining 12.
Among the patients with ventricular arrhythmias, 3 presented ventricular premature beats and 1 had nonsustained monomorphic ventricular tachycardia; none of them presented structural heart disease.
An electrophysiological study was recommended in 7 cases (4.6%) : 5 patients with regular narrow QRS tachycardia, 1 with atrial flutter and 1 with syncopal left bundle branch block. Six patients (3.9%) began antiarrhythmic therapy (4 with flecainide and 2 with amiodarone).
Patients in Whom Electrophysiological Study and/or Automatic Defibrillator or Biventricular Stimulation Were Indicated
Table 6 shows the numbers of patients with a possible indication for EPS or device implantation, on the basis of the findings specified in the "Patients and Methods" section. In the "real indication" group, we included those patients in whom some procedure had been performed previously or was found to be indicated at the time of the visit. All the patients who were being seen for the first time were analyzed separately.
The number of patients with a possible indication for cardiac resynchronization in the group with systolic dysfunction of nonischemic origin and wide QRS complex is unknown since one of the essential requirements (the presence of persistent and incapacitating symptoms despite optimal treatment7) is difficult to establish objectively in a study of these characteristics. Of the 81 patients with systolic dysfunction (EF less than 40%) of any etiology, 25 (31%) presented advanced interventricular block, a finding that does not differ widely from that reported in a recent study.12 Twenty patients met criteria for intraventricular block and systolic dysfunction unrelated to ischemia.
The same reasons justify the interrogation of the group of patients with evidence of substrate involvement in AF and pacemaker implantation for drug-refractory AF.
DISCUSSION
Rhythm and conduction disturbances are among the most common findings in a general cardiology clinic. They are detected in nearly 40% of the patients examined and in 1 of every 5 of those being seen for the first time. Seven percent of all patients and 3.5% of those being seen for the first time present clinical pictures that suggest the need to consider the performance of EPS and/or device implantation.
Atrial fibrillation was the arrhythmia most frequently found in our study, and is detected in one of every four patients examined, once again justifying its being referred to as the epidemic of the twenty-first century.13 The high proportion of patients with rheumatic valve disease in our study, 1 in every 5 of those with AF, is another noteworthy finding. This situation is not reflected in other studies in which the percentage of patients with valvular disease ranges between 4% and 19%.1-14 In the recent survey of the European Society of Cardiology (http://www.euroheartsurvey.org/), only 10% of the patients included presented heart valve disease. Although in our study, the presence of rheumatic disease was significant, the incidence of newly diagnosed cases was nearly anecdotal in that only two patients had been unaware of their being affected by the disease prior to the study. If migration does not alter this trend, we consider that, over the medium-term, rheumatic heart disease will cease to be so prevalent among our population, a circumstance that may affect the incidence of AF.
Permanent AF was the predominant clinical entity in our study, contrasting with the findings in the aforementioned European survey (https://www.euroheartsurvey.org/) and in patients hospitalized in our own center, where this clinical pattern was detected in only a third of the cases.15 Thus, it is evident that the distribution of the patterns of clinical arrhythmias depends on the health care setting in which they are being analyzed, although in no case did permanent AF represent more than 50%. Anticoagulant therapy was widely employed among our patients and, although the results differ to some extent from those of other groups,16,17 we consider that, in general, they are representative of the current trend in Spain and contrast with the situation of a decade ago.18,19 Nevertheless, the use of anticoagulants still differs according to the clinical presentation of the arrhythmia, and they are less frequently administered to treat the intermittent form, a circumstance that agrees with the general practice in Europe (https://www.euroheartsurvey.org/). This approach is justified, in part, by the younger age and lower risk of thromboembolism shown by our patients with intermittent arrhythmia, as has been reported previously.20 However, we consider that the differences observed between the paroxysmal and the persistent patterns are not explained by this fact, and that the permanent or persistent presence of arrhythmia continues to be determinant for the prescription of drug treatment, despite the fact that the information currently available recommends that it be the thromboembolic risk factors, rather than the clinical presentation of the arrhythmia, that influences the form of treatment.20-22
The prevalence of atrial flutter is low in our study. The mean patient age was greater than that of the patients with AF, and AF had been documented in 2 of every 3 of the subjects in this group, thus confirming previous reports of the frequent association between these 2 arrhythmias.23-25
Although the number of patients with ventricular arrhythmias and/or left ventricular systolic dysfunction is not inconsiderable (1.6% of all the patients, according to the MADIT II criteria), it should be pointed out that, as could be expected, the outpatient cardiology clinic is not the gateway to the health care system for patients with this type of heart disease and, thus, newly diagnosed cases are exceptional at this level of care.
The difference between what we have referred to as a possible indication for EPS and the real indication or performance of the study should not, in our opinion, be attributed to ignorance of the clinical practice guidelines or to their improper application. These documents include, as class I recommendations, radiofrequency ablation in patients with brief and/or sporadic episodes and even certain isolated episodes of narrow QRS tachycardia.6 Although the procedure can now be performed in our setting with a high probability of success and low rate of complications,26 its purpose is not to prevent fatal or disabling complications, which are exceptional in this group of diseases, but to provide an effective treatment aimed at improving quality of life. Thus, in situations in which the patient considers that the disease does not keep him or her from performing normal daily activities, other therapeutic options may be valid. In our study, 50% of all the patients with this type of arrhythmia underwent an EPS; however, radiofrequency ablation was recommended in only 28% of those being seen for the first time.
A different approach should be employed to justify the fact that only 36% of the patients with ventricular arrhythmias and indication for EPS and/or an EF less than 30% of ischemic origin27 and 63% of those presenting syncope in the presence of advanced intraventricular block10,11 were referred for EPS and/or defibrillator implantation. In the first case, the recent inclusion of this indication,7,8 together with the advanced age of a significant proportion of the patients, may have influenced our decision. In the second case, the fact that our center does not have an electrophysiology laboratory is one reason why in patients with preserved EF and advanced age, we opted for permanent pacing without prior EPS.
Although it is evident that this report is not a population-based prevalence study and that it has all the limitations of studies focusing on a single center, we consider that it can provide information on the real demand generated by these diseases in our health care system given that our clinic is the only option for specialized outpatient cardiological care, within the public health system, available to the population in our area. If we extrapolate our data, a hospital that provides care for 10 000 patients a year in its outpatient clinics will have 3400 who have never been examined by a cardiologist; the possibility of performing an EPS and/or device implantation will have to be considered in 120 of the cases. These data are based on currently accepted indications and do not include indications that are presently a subject of debate, such as those related to biventricular stimulation,28,29 or those that have yet to be fully established and developed in our setting (substrate ablation in AF), the introduction of which will require a radical change in the situation. Given that our study was based on the presence of documented arrhythmias, we have not included the indications for EPS in the absence of electrical or structural changes, despite the presence of highly specific clinical conditions (family history of sudden death, hereditary heart diseases, etc), in which the symptoms (palpitations, dizziness, etc) could influence this indication; we consider, however, that the importance of the latter situations, from a quantitative standpoint, is limited. Finally, we feel that our data may serve as a support for planning the allocation of human and material resources, as well as for establishing indicators for health care quality, designing continuing education activities or devising training programs for new specialists.
Correspondence: Dr. E. Vázquez Ruiz de Castroviejo.
Navas de Tolosa 4, P 1, 6.o D. 23003 Jaén. España.
E-mail: vazquez89@arrakis.es