Yes, cardiovascular disease remains the primary cause of mortality worldwide. But the situation has dramatically changed for the better in recent decades, with a major decrease beginning with Western countries and now reaching Eastern European countries as well. The general trend to decreased cardiovascular mortality is observed both in countries having initially a high cardiovascular disease burden, and in countries with initially low cardiovascular disease rates, such as Spain, France, or other Mediterranean countries. In France, cardiovascular mortality has decreased by 56% in the 25-year period from 1980 to 2004, and cancer has now become the leading cause of death.1
All analysts concur in attributing this remarkable achievement to both improved primary prevention and improved treatment of established cardiovascular disease.2
A DECLINING INCIDENCE OF MYOCARDIAL INFARCTIONSeveral studies have recently documented a marked reduction in the incidence of acute myocardial infarction (AMI), thereby documenting the importance of primary prevention. For instance, in the Kaiser Permanente database from California, the incidence of ST-elevation myocardial infarction (STEMI) has decreased by more than 50% in just 10 years, and nonSTEMI incidence now follows the same trend.3 Likewise, in the Framingham heart study, AMI incidence declined by 50% from 1960 to 1999.4
IMPROVED CLINICAL OUTCOMES FOR PATIENTS WITH OVERT CORONARY ARTERY DISEASEBesides this encouraging background, data are also accumulating to document the improved outcomes of patients treated for ischemic heart disease. The study presented by Arós et al. in Revista Española de Cardiología confirms the major role of improved management of STEMI, one of the main causes of coronary heart disease mortality.5 The authors analyzed 28-day and 6-month mortality from 1995 to 2005 in patients included in the PRIAMHO I, II and MASCARA registries. All 3 registries were carried out in a large number of centers, which could be considered representative of the management of patients with AMI admitted to intensive coronary care units on a nationwide scale. Particular care was given to ensure consecutive inclusion of the patients admitted during the studies’ recruitment periods, so that the results presented here undoubtedly represent an accurate picture of the management of AMI in Spain at the turn of the century. During this 10-year period, the mean age of the patients admitted remained stable (63.8 to 63.2 years) as did the sex ratio, with about 20% of the patients being women in each of the registries. Early mortality, however, decreased from 9.5% to 5.9%, with a fully adjusted odds ratio (OR) of 0.62 for 28-day mortality. The reasons for this decline in mortality were sought. Interestingly, the OR was 0.43 when only presenting variables were included in the multivariate model; however, inclusion of management variables such as reperfusion therapy or prescription of recommended medications resulted in a higher OR (0.62), bearing witness to the importance of appropriate early management, but did not erase the independent favorable influence of the time period. In other words, improved outcomes appeared not to be related only to the use of recommended medications or procedures, but to a better comprehensive approach of patients with STEMI in the most recent period.
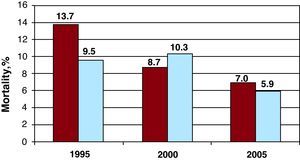
THE RESPECTIVE ROLES OF ORGANIZATION OF CARE AND REPERFUSION THERAPYIn this regard, although reperfusion therapy is obviously of paramount importance in the treatment of STEMI patients, it should not be considered the alpha and omega of STEMI management. In the 3 French surveys carried out at exactly the same time as the Spanish registries,6, 7, 8 mortality also decreased by about 50% (Figure 1), but a reduction in mortality was observed both in patients with primary percutaneous coronary intervention (PCI) or intravenous fibrinolysis and in those who received no reperfusion therapy.9, 10, 11, 12
Figure 1. Compared evolution of one-month mortality after ST-elevation myocardial infarction from 1995 to 2005 in the French 6–8 and Spanish 5 national registries.
There are several possible explanations for this remarkable achievement, beyond the broader use of recommended medications or procedures.
One of the most obvious is the better organization of care for patients with chest pain. Indeed, the results in Spain in 2005, which are quite similar to those observed in France at the time, are observed in spite of the fact that intravenous fibrinolysis still represented the reperfusion strategy in two-thirds of the patients getting reperfusion therapy at the time. This suggests that efforts must have been made to organize local or regional networks for the management of patients presenting with STEMI, with a resulting increase in the use of reperfusion therapy (from 60% to 72%), and appropriate selection of the most adapted reperfusion method. In fact, in contrast with the results of randomized trials comparing primary PCI with intravenous fibrinolysis,13 real-world data suggest that optimal use of fibrinolytic treatment may be particularly useful for patients not presenting to hospitals with PCI capability; thus, networks based either on distance from the PCI center, or on time delays from symptom onset, and with a strategy using either primary PCI or intravenous fibrinolysis, based on each individual situation, have shown mortality figures in patients initially admitted to non-PCI centers that compare favorably with those of patients admitted directly to a PCI center.14, 15 Likewise, the use of prehospital fibrinolysis in France yielded results which appeared quite similar to those of primary PCI.10, 11 To achieve its greatest benefits, however, reperfusion therapy must be implemented at the proper time. In this regard, it is essential to analyze the components of time from symptom onset to the beginning of reperfusion therapy; roughly, 3 periods can be considered: the first corresponds to the time elapsed from the onset of symptoms to the first call to medical attention; the second is the time from call to recording and interpretation of the first ECG, which will determine the nature of the acute coronary syndrome (STEMI or non ST-segment elevation acute coronary syndrome); the third is the time from diagnostic ECG to reperfusion (either ECG to needle for fibrinolysis, or ECG to balloon for primary PCI). The first time delay is partly independent of the organization of care, as it mostly depends on the patient or his/her environment; improving this time delay is crucial and requires education of the general population and also of patients with known coronary artery disease, in whom the time to first call is often hardly any less than for people without known heart disease. In the 2009 Euro Heart Survey AMI snapshot, which collected information on patients with AMI admitted to 485 centers in 47 countries over a 1-week period in December 2009, the median time from symptom onset to first call to medical attention was 105min, which is obviously exceedingly long (personal data). The second and third time delays (from initial call to ECG, and from ECG to reperfusion therapy) are crucial steps in the organization of care on regional and local levels, depending on the type and location of the first medical contact. The recent European Society of Cardiology guidelines on STEMI recommend that for patients with chest pain the diagnostic ECG should be performed within 10min of the initial contact, and preferably in the prehospital setting.16 Once the diagnosis of STEMI is made, the type of reperfusion therapy must be decided and, be it fibrinolysis or primary PCI, the patient must be brought to a PCI-capable center. Shortening time delays between diagnostic ECG and reperfusion is crucial, but it is a difficult task, even when the patients initially present to a PCI-capable center. In the 2009 Euro Heart Survey AMI snapshot, the median time delay from ECG to primary PCI was 115min, and the median time delay from ECG to fibrinolysis was 50min (personal data); in other words, more than half of the patients with STEMI got reperfusion therapy beyond the recommended timelines.
Benchmarking processes, however, may help in improving these delays, as was recently evidenced by the third Euro Heart Survey on acute coronary syndromes: from 2006 to 2008, the delay from admission to reperfusion at the participating institutions (which regularly monitored their own performance) decreased from 60 to 45min for primary PCI and from 20 to 15min for intravenous fibrinolytic treatment.17 In the Spanish registries, the main improvement in time delays was observed for the symptom onset to monitoring time (from 135min in 1995 to 95min in 2005), which reflects the addition of the symptom to call and call to ECG delays, whereas the door to needle times decreased to a lesser extent (from 60min in 1995 to 43min in 2005), and the door to balloon times actually increased from 2000 (median: 80min) to 2005 (95min). This finding therefore mainly reflects an improved organization of care at the very early stage of myocardial infarction, and leaves room for further improvement in the subsequent steps (from ECG to reperfusion).
A FURTHER POSSIBLE ROLE OF PREVENTIONAlthough a better organization of care is likely to be a major determinant of improved acute outcomes in STEMI patients, there is also some evidence that the initial severity of STEMI might be less at present than 10 or 15 years ago. In the Spanish registries, the proportion of patients with severe signs of heart failure (Killip class III or IV) tended to decrease from 13.5% in 1995 to 11.3% in 2005. During the same time period, the proportion of patients with any sign of heart failure (Killip classes II to IV) in the French registries decreased from 35% to 24%; likewise, from 2000 to 2010, the proportion of patients with signs of heart failure on admission decreased from 20% to 15.5% (personal data). Although these data will need confirmation, it may well be that the efficacy of primary prevention of coronary artery disease has led not only to a decrease in the incidence of AMI, but also, when myocardial infarction occurs, to less severe forms.
OUTSTANDING ACHIEVEMENTS DO NOT MEAN THAT THE FIGHT AGAINST CORONARY HEART DISEASE IS OVEROverall, the data from the PRIAMHO I and II and from the MASCARA registries are an additional piece of evidence of the outstanding achievements of cardiology in recent decades. This is all the more satisfying as it does not appear to be the result of a single therapeutic breakthrough in our field, but rather of many diverse improvements in the management of coronary artery disease, ranging from the successes of primary prevention by public health measures, such as the smoking ban implemented in most European countries, to the use of medications that treat specific risk factors such as hypertension or hyperlipidemia more effectively, and to the more widespread use of reperfusion therapy making the best of the two available options, fibrinolysis and primary PCI, without forgetting the major contribution of the general organization of care for patients with prolonged chest pain.
Although we have reason to be proud of this collective effort, we should certainly not think that we can now rest on our laurels. From nearly everywhere in the world, we receive worrying news that our way of life, beginning with the way we eat and the fact that we appear to be more and more sedentary, leads to an epidemic of obesity, with rapidly rising figures for diabetes mellitus as its corollary. Also, the most recent data on smoking in France suggest that after a continuous decrease in the last 20 years, the figures are now rising again, particularly in younger women; in this regard, the increase in the proportion of women under the age of 50 years among AMI patients in the French registries (from less than 4% in 1995 to more than 11% in 2005) should sound as an alarm bell. If we are collectively unable to restore an appropriate balance between the time we spend walking and the time we spend in front of TV or computer screens, and do not make amends with our way of life, there is much to fear that we will lose at least part of the recent gains in terms of cardiovascular disease prevention.
We have lived an incredible experience in the past 30 years, but in spite of our successes, the time has not come to slacken our efforts to fight coronary artery disease.
CONFLICTS OF INTERESTProf. Danchin has received research grants from Astra-Zeneca, Eli-Lilly, GSK, Merck, Novartis, Pfizer, Sanofi-Aventis, Servier, and The Medicines Company. He has also received fees for speaking in industry-sponsored symposia and/or consulting for AstraZeneca, Bristol-Myers Squibb, Boehringer-Ingelheim, GlaxoSmithKline, Lilly, Menarini, Merck, Novartis, Novo, Pfizer, Sanofi-Aventis, Servier, and The Medicines Company.
.
Corresponding author: Division Maladies Coronaires et Soins Intensifs, Hôpital Européen Georges Pompidou, Assistance Publique des Hôpitaux de Paris, 20 rue Leblanc, 75015 Paris, France. nicolas.danchin@egp.aphp.fr